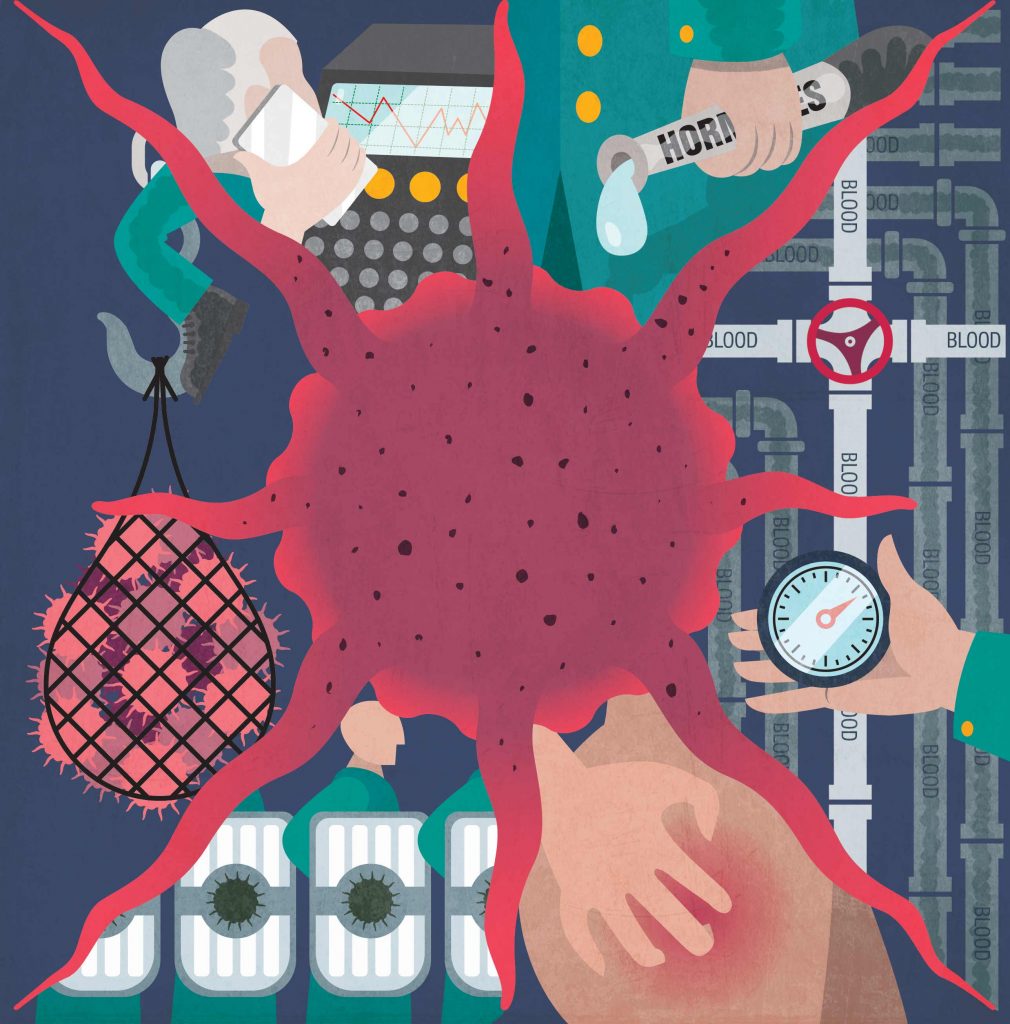
No cancer cell can survive, thrive, proliferate, infiltrate or metastasise without concerted help from the tumour microenvironment (TME). So shouldn’t treatment strategies aim to modify what’s happening around the cancer as much as directly targeting the cancer itself? Janet Fricker looks at some key TME battlefronts, and hears from people leading efforts to move treatment paradigms towards an integrated ‘battlespace plan’.
Last September, in a lyrical essay published in The New Yorker, Siddhartha Mukherjee brought to the attention of the wider public a paradigm shift in the understanding of cancer. Using the analogy of Lake Michigan, where quagga mussels have supplanted plankton due to multiple changes in the ecosystem, he explained how alterations in the environment at distant metastatic sites allow cancers to take hold. Mukherjee, a cancer biologist and oncologist perhaps best known for writing the Pulitzer prize-winning book The Emperor of All Maladies, explored how the focus in oncology is shifting from ‘the seed’ – the cancer cell – to ‘the soil’ – the environment in which cancer cells live.
No tumour is an island. There is now widespread recognition that cancers do not grow in isolation, and that both primary and metastatic cancers inhabit unique ecosystems, known as the tumour microenvironment (TME), that can have a major influence on patient outcomes. “The TME concept of cancer has been embraced by the cancer community. If you look at the American Association for Cancer Research’s membership, the largest subgroup – with 7,888 members – is TME, indicating the current strength of the field,” says Kenneth Pienta, a medical oncologist from John Hopkins, credited with first making the analogy between ecology and cancer.
The TME, the ecosystem in which cancers grow, consists of a myriad of different cell types, often referred to as ‘stromal cells’, which include: cancer-associated fibroblasts, endothelial cells (that compose blood vessels within the tumour), fat cells, nerves, and cells of the immune system.
Both the cancer cells themselves and stromal support cells manufacture a multitude of chemicals, including cytokines, such as tumour necrosis factor and interleukin-6, that provide cross-talk with positive and negative signals between the tumour and surrounding cells, which help it to grow, build a blood supply, invade, and metastasise. “People used to think of cancer as a ball of genetically altered cells growing out of control, but we now know that cancer cells hijack normal tissue support systems to form a rogue organ made up of a whole host of cells that help the tumour to grow, spread and resist treatment,” says Fran Balkwill, who leads the Centre for Cancer and Inflammation at Barts Cancer Institute, London.
In addition to the local TME, investigators are also considering the cancer holistically in relation to other body systems that can influence cancer genesis, survival and proliferation, including the microbiome and hormones.
Cancer cells cannot grow without a corrupted microenvironment, both locally and during metastatic colonisation of distant tissue sites, where they must create favourable microenvironments that support the growth of the secondary mass. The primary tumour is able to shape the microenvironment of the secondary mass. “Thus the metastatic TME is influenced by the primary TME, because it receives signalling messages from the primary tumour,” says Michael Schmid, who has spent many years studying aspects of the TME, and is currently leading research on the tumour microenvironment in pancreatic cancer metastasis at the Institute of Translational Medicine in Liverpool, UK.
An underappreciated aspect of the TME is its relative abundance in comparison to cancer cells in some solid tumours, adds Schmid, who originally trained at the University of Bern, Switzerland. For example, in pancreatic cancer the microenvironment can represent up to 80% of the tumour mass. “One of the reasons pancreatic cancer has the deadliest outcomes may be due to its large microenvironment creating more signals to help cancer cells to grow, survive and spread,” he says.
While stochastic events – the accumulation of random mutations within specific pathways in particular cell types – have long been known to play a role in cancer aetiology, the TME is now understood to be a decisive factor in determining whether those mutated cells proliferate, remain in an indolent micro-hyperplasia, or are cleared by the immune system. “The genetic damage is the match that lights the fire, but the tumour microenvironment is the fuel that fans the flames. For cancers to take hold you need both,” says Balkwill.
The angiogenesis battlefield
Currently approved anti-angiogenic therapies target the vascular-endothelial growth factor VEGF, and include the monoclonal antibody bevacizumab (Avastin) and the TKIs sunitinib (Sutent) and sorafenib (Nexavar). In clinical trials, benefits have proved relatively modest, with the drugs only temporarily slowing tumour growth, and tumours often becoming resistant. Major research efforts are currently underway to identify biomarkers predicting patients likely to respond to different angiogenesis inhibitors.
Investigators are also exploring other potential mechanisms where tumours can be vascularised without angiogenesis. These include ‘vascular mimicry’, where the plasticity of tumours allows them to form channels that serve as irrigation systems for tumours; vessel co-option, where tumours hijack pre-existing capillaries from surrounding tissue; and intussusceptive angiogenesis, where pre-existing vessels split into daughter vessels.
Other avenues of investigation include looking at the impediment to effective drug delivery presented by the tortuous capillaries induced by angiogenesis. Recently, Diana Passaro (The Francis Crick Institute, London) showed increased nitric oxide (NO) production made blood vessels leakier in mouse models and patient xenotransplants of acute myeloid leukaemia. “When the vessels are leaky, bone marrow blood flow becomes irregular and leukaemia cells can easily find places to hide and escape chemotherapy, while normal tissue stem cells are displaced to the periphery,” explains Passaro, who demonstrated NO blockers in combination with chemotherapy compared to chemotherapy alone slow leukaemia progression.
Evidence is now emerging that, in addition to its role on the angiogenesis battlefield, VEGF may be active in the immune system battlefield, as an inhibitor of T-cell infiltration of tumours. “Anti-VEGF antibodies may also work by reducing the immune suppressive environment,” says Francesco Bertolini (European Institute of Oncology, Milan).
Potential strategies of attack
At present, with the exceptions of hepatocellular carcinoma and kidney cancer, where sorafenib and sunitinib are active as single agents, anti-angiogenic regimens are given only in combination with standard chemotherapies. VEGF inhibitors are also being investigated in adjuvant (post-surgical) settings with the idea of halting angiogenesis to prevent micrometastasis, and in neoadjuvant settings to downsize tumours.
Given the finding that anti-VEGF agents may reduce immune suppressive environments, trials are underway to see if agents have synergistic effects with check point inhibitors.
On the vascular leakage battlefront, Passaro anticipates that translation of the vascular pathologic phenotypes observed in mice to human patients, together with the characterisation of the optimal agents to block vascular leakiness, will provide strong evidence to start clinical trials using vascular normalisers combined with chemotherapy to improve survival in leukaemia patients.
A new battlespace in the war against cancer
The new focus on the TME – looking at the soil not just the seed, the fuel not just the spark – is giving an important boost to the whole prevention agenda, by turning attention to what can be done to promote a healthy ecosystem that denies cancer cells the environment they need to develop, survive, thrive and spread. This is the approach emphasised, for instance, by Pienta and also by Mukherjee in his New Yorker article, which was titled ‘Cancer’s invasion equation’.
For others, however, our growing knowledge about the support services that cancer cells rely on is opening up new strategies for treating the disease that go beyond the current paradigm of targeting the mutations in the cancer cells themselves to taking on the entire cancer support system. Interest in this approach is increasing as expectations are tempered about what can be achieved by personalised cancer medicine targeted at individual cancer cell mutations.
One of the chief battle strategists behind this new approach is Douglas Hanahan, who is best known for two articles published in Cell (2000 and 2011), co-authored with Robert Weinberg, that conceptualised the complexity of cancer into a logical set of common ‘hallmark’ traits (currently eight).
Hanahan heads a research group on cancer development and progression at the Swiss Institute for Experimental Cancer Research in Lausanne, and has a particular interest in the role of the heterotypic tumour microenvironment and the accessory cells that collaborate with cancer cells to manifest malignant disease. He argues that we need to take Nixon’s War on Cancer to the “intergalactic level”, by adopting the ‘battlespace’ approach developed by the US Department of Defense, which involves “integrated information management of all the significant factors that impact on combat operations by armed forces”.
“We need a battlespace plan for attacking cancer that integrates all the relevant information about significant factors that impact on therapeutic efficacy in the particular cancerous theatre of operation,” he says.
The neurogenesis battlefield
The role of neurogenesis in promoting cancer progression was revealed five years ago in a landmark study that involved injecting human prostate cancer cells into mice and systematically disabling different parts of the nervous system. Researcher Claire Magnon and colleagues revealed contributions from two parts of the autonomic nervous system: the adrenergic pathway (also known as the sympathetic nervous system) and the cholinergic pathway (also known as the parasympathetic nervous system) (Science 2013, 341:1236361). “We found a dual effect that the adrenergic pathway stimulated the early stages of cancer progression, while the cholinergic pathway activated cancer cell dissemination and metastasis,” explains Magnon, who at the time was working at the Albert Einstein College of Medicine, New York.
Further support for the concept was provided by studies from other labs showing the effects on cancer of surgical or pharmacological denervation of mouse models of gastric tumours (Sci Transl Med 2014, 6:250ra115); pancreatic cancer (Cancer Res 2014, 74:1718‒27); breast cancer (Mol Oncol 2015, 9:1626-35); and skin cancer (Cancer Stem Cell 2015, 16:400‒12).
Additionally, in a retrospective analysis of prostate adenocarcinoma specimens, Magnon showed sympathetic and parasympathetic nerve fibre densities were two- to three-fold higher in patients with aggressive tumours compared to those with less aggressive tumours (Science 2013, 341:1236361).
The molecular mechanisms of cancer nerve dependence remain to be fully elucidated, with studies exploring how nerve cells influence endothelial cells and metastasis. “We have the suspicion that nerves are involved in all cancers, but this has yet to be proved,” says Magnon, who is now based at the French Alternative Energies and Atomic Energy Commission, in Paris.
Potential strategies of attack
Denervation, says Magnon, is likely to prove too risky a treatment strategy, since it can result in complications such as impotence for people with prostate cancer. A more practical approach, she suggests, would be therapies to block receptors of neurotransmitters. A major contender is repurposing of beta blockers, currently used to treat hypertension and arrhythmia, which work by blocking activation of adrenergic receptors by noradrenaline and adrenaline. Support for this approach comes from retrospective epidemiological studies in lung, breast, and prostate cancer, and melanoma, showing that patients taking beta blockers survive longer with lower rates of recurrence and metastasis. Whereas existing beta blockers primarily bind to the beta 1-adrenergic receptor, future drug development would aim to target selectively the beta 2 and beta 3 receptors implicated in cancer nerves.
Beta blockers might be used for the adrenergic pathway in early cancer, says Magnon, but different agents would be needed to block the cholinergic pathway in more advanced disease. Here she suggests scopolamine (a drug currently used for motion sickness), which could target muscarinic receptors.
Theatres of conflict
The significant factors in the cancerous environment commanding the greatest interest today are described below. Some have been known about, at least partially, for some time, while the role of others is only just beginning to be defined.
Angiogenesis – blood supplies
Angiogenesis – the development of new blood vessels – is a normal physiological process involved in embryo development, growth and wound healing. Its role as a significant factor in the development of cancer was first proposed in 1971, when Judah Folkman published his hypothesis that, in order to grow beyond 1–2 mm3, tumours trigger the growth of new blood vessels to carry nutrients and oxygen to cancer cells (NEJM 1971, 285:1182–6).
We now know that pro-angiogenic factors are secreted by cancer cells into the TME where they stimulate blood vessel growth. Of all the identified molecules leading to blood vessel formation, vascular-endothelial growth factor (VEGF), overexpressed in the majority of solid tumours, has been the main therapeutic target. The impact of anti-VEGF therapies has so far been limited, however. One of the main challenges in the angiogenesis battlefield seems to be that tumours produce multiple angiogenic molecules, they depend on different angiogenic factors at different stages of development, and they have alternative approaches for accessing blood supplies.
Neurogenesis – promotes growth and infiltration
For many years the role of nerve fibres in cancer progression was believed to be mechanical, offering ‘paths’ for perineural invasion. But now tumours are also thought to stimulate the formation of new nerve fibres within tumour masses in a process called neurogenesis, analogous to angiogenesis. Here it is believed ‘cross-talk’ occurs between cancer cells releasing neurotrophic factors stimulating nerve infiltration, and molecular mediators from nerve-stimulating cellular pathways that promote growth of cancer cells. Investigators have demonstrated that nerve fibres infiltrate breast, gastric, pancreatic, colon and prostate cancers.
The inflammation battlefield
Initial efforts to tackle cancer by targeting chronically inflamed environments focused on developing a class of non-steroidal anti-inflammatory drugs that selectively inhibit Cox-2, an enzyme induced by inflammatory stimuli known to be associated with carcinogenesis. Clinical trials of rofecoxib (Vioxx) and valdecoxib (Bextra) conducted in people with a history of colorectal adenomatous polyps demonstrated a significant reduction in the occurrence of colorectal adenomas (benign precursors of cancer). But interest waned after the two drugs were withdrawn in 2004/2005 due to their association with cardiovascular problems, and the anti-inflammatory spotlight shifted to aspirin.
Much of the evidence showing aspirin can be effective against cancer comes from the work of Peter Rothwell, professor of neurology at the University of Oxford, who, from 2010 onwards published a series of systematic reviews and meta-analyses of a large number of trials originally designed to look at the effects of aspirin on cardiovascular disease. The studies showed people allocated to aspirin developed fewer cancers, and that if people did develop cancer, it was less likely to metastasise.
Ruth Langley, professor of oncology at University College London, is now heading up a major phase III randomised controlled trial ‒ the Add-Aspirin trial ‒ to help find out whether regular aspirin use after treatment for a variety of early stage cancers can prevent or delay a recurrence. Looking at all the evidence gathered so far, however, Langley believes that, although aspirin inhibits Cox-2 to some extent, at the doses used (75‒300 mg once daily) the anti-cancer benefits are more likely derived from an anti-platelet effect and may therefore be more active in the immune than the inflammatory ‘battlefield’. “We think platelets facilitate the adhesion of cancer cells to the endothelium and protect circulating cancer cells from immune-mediated clearance by natural killer cells,” she says.
Potential strategies of attack
If the Add-Aspirin trial proves positive, it could open the way for aspirin to be used in metastasis prevention. “With aspirin there’s always the risk of increased bleeding. In deciding whether to use aspirin for individual patients we’ll need to do a risk–benefit analysis. But until we’ve demonstrated efficacy we can’t undertake that equation,” says Langley.
Other potential approaches to tackling cancer by addressing inflammatory environments include canakinumab, a man-made antibody targeting interleukin 1-beta, believed to be a mediator of TME inflammation. In the recent CANTOS study, designed to explore whether canakinumab could prevent recurrent vascular events in cardiovascular disease in patients with high inflammatory responses, it was noted that total cancer mortality and lung cancer mortality were significantly lower among patients treated with canakinumab than in the control group (The Lancet 2017, 390:1833‒42). The striking difference in lung cancer rates found in CANTOS have set in motion plans by Novartis for a phase I study looking at the combination of canakinumab and a PD-1 inhibitor in patients with non-small-cell lung cancer.
Inflammation – the spark and the fuel
The role of chronic inflammation in promoting cancer was flagged up by Harold Dvorak (Harvard University) in 1986, in an essay in the New England Journal of Medicine titled ‘Tumours: wounds that do not heal’. Dvorak drew attention to the many similarities between solid tumours and wound healing, including basic developmental mechanisms such as angiogenesis, tissue infiltrating lymphocytes, macrophages and mast cells.
It has long been known that chronic inflammatory diseases, such as pancreatitis, Crohn’s disease and chronic infection with human papilloma virus, as well as inflammation from long-term exposure to cigarette smoking, increase the risk of cancer.
Chronic inflammation is now known to favour all phases of carcinogenesis. At the initial phase, it produces the reactive oxygen species which induce the DNA mutations that drive cancer formation. At later phases, the cancer can hijack inflammatory pathways to promote tumour progression and metastasis through production of tumour-growth-promoting chemokines, prostaglandins, and leukotrienes.
Inflammation also mediates other aspects of the TME known to be associated with cancer risk, including obesity, hormone levels, and the makeup of the microbiome.
Metastasis – colonising new territories
Metastasis, whereby tumour cells colonise distant organs, is estimated to be responsible for 90% of cancer deaths. The metastatic cascade is a complex step-by-step process in which cancer cells detach themselves from primary tumours, enter the circulation or lymphatic system, adhere to specific sites, and begin to proliferate. Our growing understanding of the metastatic process indicates that the microenvironment plays an important role at both the primary and the distant site. It was David Lyden (Cornell University, New York) who in 2005 first proposed the term ‘metastatic niche’ to describe the phenomenon where primary tumours promote metastasis by establishing supportive environments at distant sites before cancer cells begin to spread. Finding ways to counter factors that favour metastasis is now a major area of research.
Unanswered questions in metastasis include why it only affects certain patients, the organotrophic attraction of cancer cells to different organs (e.g. breast tumours travelling to bone and pancreatic tumours to liver), and how in some patients micrometastases can remain dormant at new sites for decades.
The metastatic battlefield
“During embryonic development some cells migrate enormous distances in order to form distinct tissues and organs and it’s this process that gets exploited by cancer cells undergoing metastasis,” explains Erik Sahai, at the Francis Crick Institute in London. His lab is investigating the genetic and molecular changes in the cellular environment around a tumour that enable cancer cells to break away and start moving towards new sites.
One area of interest is the role of tumour-associated fibroblasts around primary tumours, which help cancer cells spread. “The fibroblast is like the guy at the front with a machete clearing a path through the jungle for the cancer cells to follow through,” says Sahai, who has demonstrated interaction between two different proteins: E-cadherin, located on the surface of cancer cells, and N-cadherin, expressed on the surface of fibroblasts (Nature Cell Biol 2017, 19:224‒37).
Research carried out by David Lyden at New York’s Cornell University, involving labelling tumour cells, indicates that a mechanism for metastasis involves transportation of exosomes directly from tumours to premetastatic sites, preparing the location for subsequent colonisation by cancer cells. Exosomes are small membrane-bound vesicles (30–100 nm in diameter) with cargoes of proteins, lipids, and nucleic acids that can be transported from one cell to another.
“We believe they’re responsible for creating the pro-inflammatory immune microenvironment and vascular leakiness responsible for metastatic cancer cells being able to survive,” says Lyden, who has demonstrated that 500 tumour samples from 30 different types of cancer secrete exosomes.
More recently, Lyden has shown that exosomes targeting different sites display different cell-adhesion receptor proteins (called integrins) on their surface, and that the integrin profile facilitates uptake into organs. For example, the alphaV beta5 integrin directs exosomes to the liver; whereas the alpha6 beta4 integrin promotes homing to the lungs (Nature 2015, 527:329‒35). “Integrins act like zip codes and go some way to solving the mystery of organotropism – why cancer metastasises to certain organ sites,” says Lyden.
Potential strategies of attack
In some countries, postmenopausal women with primary breast cancer are already prescribed adjuvant bisphosphonates ‒ drugs used in osteoporosis ‒ to reduce risk of developing bone metastases. The recommendation to use bisphosphonates for this purpose was made by an expert panel following results of a meta-analysis showing that, among 11,767 postmenopausal women treated for breast cancer, adjuvant bisphosphonates produced significant reductions in bone recurrence (relative risk 0.72) and breast cancer mortality (RR 0.82) (The Lancet 2015, 386:1353‒61).
Research by Alison Gartland (University of Sheffield) indicates the enzyme lysyl oxidase (LOX), released from the primary breast tumours, generates pre-metastatic niches within the bone, and that bisphosphonates change the bone microenvironment to prevent this from happening (Nature 2015, 522:106‒10).
In future, Lyden believes that gaining a better understanding of the metastatic niche could provide new strategies for inhibiting metastatic cell growth. Therapies might focus on stopping exosome production and packaging of contents (tumour proteins, lipids and genes) at the tumour level, or on developing antibodies to block integrins, so as to prevent exosomes fusing with target cells.
Quantifying the extent of exosome production might be used to personalise treatment, with patients producing high levels of exosomes (at greatest risk of metastasis) prescribed aggressive treatment following surgery, and those producing lower levels spared treatment.
Hormones – protectors and sustainers
The best known examples of hormone effects on cancer include the impact of testosterone on prostate cancer and oestrogen and progesterone on breast cancer. Other lesser-known effects include pancreatic cancer being affected by insulin-like growth factor and lung cancer by epidermal growth factor. The concept of removing hormones to treat cancer was first employed in 1896 by George Beatson, a surgeon from Glasgow, who used oophorectomy – surgical removal of the ovaries – to treat metastatic breast cancer.
Michael Pollak, from McGill University, Montreal, is leading efforts to research the role of the metabolic hormone insulin in promoting different cancers, and the potential clinical implications. “The behaviour of most normal cells is determined by their hormonal environments, with cell surface receptors detecting hormones that can alter cell behaviour,” Pollak explains. He estimates that around three quarters of cancers retain some responsivity to hormonal environments. “Although completely different from toxic carcinogens, hormones enable mutated cancer cells to live longer, so they’re more likely to divide and form tumours,” he says.
“We haven’t yet succeeded in applying general hormone principles optimally across all types of cancers,” he adds, but argues that “there are likely to be many more cancer types that have yet to be identified with receptors for different hormones that encourage growth, which could be targeted as treatments.”
The immune system – friend or foe?
The potential role of the immune system in countering cancer – recognising cancer cells as abnormal and eradicating them‒– has been postulated since the end of the 19th century. In 1891, after stumbling on the case of a patient whose cancer regressed after a severe skin infection, William Coley tried treating cancer patients with intratumoural injections of inactivated Streptoccus pyogenes and Serratia marcescens in the hope of ‘stimulating the body’s ‘resisting powers’. Later it became apparent that it was not the bacteria that were responsible for the antitumour effects observed, but rather that the bacteria activated the immune system to destroy tumours.
“Any change to our proteome caused by cancer-related genetic changes has the potential to be recognised as foreign by the immune system,” says Tim Elliott, who directs the new Centre of Cancer Immunology at the University of Southampton. A big problem, however, is that cancer cells are able to activate checkpoint inhibitor molecules, such as PD-1 and CTLA-4, which originally evolved to shut off immune responses so as to prevent the immune system from causing autoimmune diseases, such as type 1 diabetes and rheumatoid arthritis. This may help explain the disappointing vaccine trials in the early 21st century which, with a few notable exceptions (such as BCG vaccine in bladder cancer), either failed or had modest effects. “At the time we didn’t know about checkpoint blockade, and were recruiting a lot of well-intentioned cytotoxic T-cells to tumours, which got switched off,” says Elliott. Targeted therapies that block immune checkpoints have led to important survival gains particularly for certain patients with advanced melanomas.
The hormonal battlefield
While the role of sex hormones, and potential therapeutic implications, remain of great interest, in recent years it is insulin that has attracted the spotlight, with investigators exploring its potential role as a mediator between obesity and the heightened risk of cancer. Overweight or obese people have increased levels of blood insulin, since excess body fat leaves cells increasingly resistant to the effects of insulin, causing the pancreas to go into overdrive.
By binding to receptors on the surface of cells, insulin has been shown to have mutagenic and anti-apoptotic effects in several cancers, including breast cancer. Cohort studies have shown increased incidence of several malignancies including those of the bladder, breast, colon, endometrium, liver and pancreas in patients with type II diabetes. Furthermore, in mouse models of cancer, strong circumstantial evidence exists that if investigators experimentally raise insulin the rate of cancer growth increases.
Potential strategies for attack
Hormonal therapy is widely used in breast and prostate cancer to remove hormones to slow the growth of cancer. In breast cancer, tamoxifen blocks cell receptors for oestrogen and aromatase inhibitors (anastrozole, exemestane and letrozole) stop the production of oestrogen. Both classes of drugs are used in hormone-receptor-positive breast cancers as adjuvant treatments following surgery to stop oestrogen from encouraging cell growth, and also to slow growth of metastatic breast cancer. Androgen suppression therapy is used in prostate cancer, with approaches including luteinising hormone-releasing agonists for stopping production of testosterone, and anti-androgens for preventing testosterone from attaching to receptors on prostate cells.
More recently, in lung cancer, monoclonal antibodies such as cetuximab have been used to block receptors to prevent epidermal growth factor from encouraging cancer growth.
On the insulin battlefield, recent studies have explored whether metformin ‒ a biguanide, which lowers levels of glucose and insulin, and is the most widely prescribed drug for type 2 diabetes ‒ could be repurposed for the prevention and treatment of cancer. “Metformin has the advantage of being safe and well tolerated. However, unfortunately it only lowers insulin levels by around 20%, which has limited impact on hyperinsulinaemic patients, who usually have double or triple normal levels of insulin,” explains Michael Pollak, a leading researcher in this field, from McGill University, Montreal, Canada.
A phase II randomised controlled trial involving 121 patients with advanced pancreatic cancer, undertaken by Pollak and colleagues, showed no difference in overall survival between patients randomised to the control arm (standard of care) and the experimental arm (standard of care plus metformin) (Lancet Oncol 2015, 7:839‒47).
One avenue being explored is to focus on more potent biguanides. Pollak cautions, however, of the danger that the patient could become a type 1 diabetic if their insulin levels are lowered too far. “We don’t know if there’s a sweet spot that can be achieved where insulin levels are safe for patients, but damaging to tumours,” he says.
Metformin may also have a role to play in cancer prevention. A Japanese phase III randomised study of 151 patients who had colorectal adenomas resected by endoscopy found those assigned to metformin had a significantly lower recurrence of polyps and adenomas (P=0.034) after one year (Lancet Oncol 2016, 17:475‒83). “This looks encouraging, but prevention trials are not so advanced because they need thousands of patients and long-term follow-up,” says Pollak.
Microbiome – the local and remote impact of our gut residents
The human microbiota, including bacteria, archaea, protozoa, fungi, viruses, and bacteriophages, reside on internal and external surfaces of the body. More than 100,000 different species occupy the human ecosystem, and their cells are thought to outnumber human cells by a ratio of up to three to one.
The concept of bacterial infection leading to cancer is far from new – links between stomach cancer and Helicobacter pylori infection have been known for years, and are now understood to be mediated by chronic inflammation.
More recently, new knowledge has been emerging about the role our microbiome plays in the development and growth/inhibition of cancer both locally, within the gut, and – more surprisingly – remotely, anywhere in the body.
The makeup of the gut microbiome is one of the strongest factors currently known to predict response to treatment among people treated with immunotherapies for cancers including advanced melanomas and lung, renal and urothelial cancers.
Within the gut itself, studies comparing the microbiota of people with colorectal cancer against healthy controls have shown a greater abundance of bacteria previously reported as oral pathogens among those with colorectal cancer (Gut 2017, 66: 633-643).
The immune system battlefield
Immune checkpoint blockers, which boost the body’s own immune system rather than affecting the cancer cells, are considered one of the first successful ‘soil therapies’, changing the cancer’s ecosystem or TME. The antagonistic antibodies nivolumab (Opdivo) and pembrolizumab (Keytruda) target PD-1, ipilimumab (Yervoy) targets CTLA-4, while atezolizumab (Tecentriq) targets the PD-1 ligand PD-L1. All of them, in effect, remove a cancer imposed ‘brake’ on the immune system.
Although checkpoint inhibitors have been successfully used to treat some patients with metastatic melanoma, lung cancer, renal cell carcinoma and Hodgkin’s lymphoma, the approach only delivers long-term results in around one in four patients. A potential way forward, says Tim Elliott, who directs the new Centre of Cancer Immunology at the University of Southampton, could be to combine checkpoint inhibitors with vaccines.
A recent study by Vésteinn Thorsson (Institute for Systems Biology, Seattle, Washington), which used data from The Cancer Genome Atlas (TCGA) that analysed more than 10,000 tumours encompassing 33 diverse cancer types, identified six different subtypes for immune infiltration of tumours (Immunity 2018, 48: 812‒30). “The really exciting finding was that the six categories cut across all the different types of cancer,” comments Elliott. “There seems to be a strong correlation between having lots of immune cells infiltrating tumours ‒ in particular lymphocytes ‒ and good outcomes.”
A critical question, adds Elliott, is why some tumours attract lymphocytes while others do not.
In an intriguing case report where a number of different metastatic sites in a woman with advanced ovarian cancer were analysed by immunogenics, Martin Miller (Cancer Research UK, Cambridge Institute) showed that immune microenvironments differ between sites in the same patient, with progressing metastases characterised by immune cell exclusion and regressing and stable metastases infiltrated by CD8+ and CD4+ T cells (Cell 2017, 170:927‒38). Such findings suggest that multiple distinct tumour immune microenvironments co-exist within single patients.
“Our hypothesis is that the tumour itself can programme signalling pathways that have a strong effect on the immune microenvironment, which ultimately dictates whether immune cells can infiltrate the tumour,” says Miller. His team is now hunting for the signals that govern the TME in metastatic disease to understand how cancer cells create a pro-tumourigenic niche.
Potential strategies of attack
Strategies for improving the response to immune checkpoint blockade remain a very active area of research. This includes issues of dose, combinations, and sequences, as well as the potential benefits of combining checkpoint blockade with vaccines. Emerging understanding about the role of the gut microbiome in determining response to immunotherapy is also opening up new lines of research into the potential for modifying patients’ microbiota to optimise immune response (see next box ‘Microbiome battlefield’).
Other immunology approaches being explored in cancer include Chimeric Antigen Receptor (CAR) T-cell therapy, where T cells are engineered to enhance the response of the immune system against a specific tumour antigen. For the process, T cells are extracted from the patient’s blood through leukapheresis and then genetically modified to be specific to antigens expressed on tumours but not on healthy cells. They are then grown in large numbers ‒ ‘expanded’ ‒ and then infused back into the patient. Two new treatments for children with acute lymphoblastic leukaemia and for adults with lymphoma have been approved by the FDA, but the downside is that they are hugely expensive, costing around $475,000 per patient.
Towards a strategic battlespace plan
Greg Hannon, director of the Cancer Research UK Cambridge Institute, supports Hanahan’s call to extend the target of cancer treatment beyond the cancer cells into the environment that sustains the tumour, arguing that targeting the “genomically stable host cells” of the TME “offers the potential to get around some of the tumour’s problems of diversity, adaptability and plasticity.”
Tim Elliot, of the Cancer Immunology Centre in Southampton, agrees. “In future, to guide therapy we will need to obtain comprehensive pictures of the individual patient, taking into account the cancer genome, the TME and interactions between the two.” Such an approach would deliver the ultimate personalised therapy, he adds.
To do this effectively will require greater understanding of the extraordinary complexity of the TME – aptly described by Mukherjee as an “infuriatingly intricate web”. This in turn will require sophisticated modelling, with investigators taking a range of different strategies to delve into the complex ecosystems and probe the cross-talk between different components, to gain an accurate description of the interconnectivity of the TME and the plethora of molecular mechanisms and types of cells involved.
One such investigation is being led by Martin Miller (Cancer Research UK Cambridge Institute), who is using ‘big data’ to look for TME signatures in large tumour cohorts that can be linked to patient outcomes, to discern patterns that provide informative narratives about particular cells, pathways and molecules.
Another is the ‘CANBUILD’ project, led by Fran Balkwill at the Bart’s Cancer Institute, London, which is using tissue engineering and stem cell techniques to create a 3D ovarian cancer model composed of fat cells, fibroblasts, mesothelial cells and tumour cells, measuring a few millimetres across. “We hope to put various elements of the TME together and ask questions about what they do by strategically removing different components,” Balkwill explains, adding that the next step is to add blood vessels and macrophages. Ultimately it is hoped that the model can be used to test therapies targeting the TME.
But perhaps the most audacious endeavour so far is the IMAXT project, where an interdisciplinary team involving breast cancer genomic researchers, computational biology experts, mathematicians, microscopy experts, astronomers and game developers are collaborating to make a 3D virtual reality model of the breast cancer TME. The team, from the UK, Switzerland, USA, Canada and the Republic of Ireland, are gathering thousands of bits of information about every cell in the tumour to explore how they interact and influence each other.
Greg Hannon is the principal investigator of IMAXT. “We realised that to embrace the incredible complexity of the TME we needed to devise methods not just to quantify the number and type of cells present, but also to consider how spatial locations and 3D architecture influence function. We want to be able to capture who is talking to whom and what they are saying,” he says.
Working initially with biopsies of around 100,000 cells, the team are using Serial Two Photon Tomography (TM) technology to image tumour slices at submicron resolution and then analyse them for the genetic information in every cell.
Currently the team is imaging mouse tumours a millimetre across to perfect the technology, but they hope to move onto imaging tumour samples from the METABRIC project, where Carlos Caldas and colleagues categorised breast cancer tumours from over 2,000 women into 11 different subtypes (see ‘Don’t shoot the driver’, Cancer World 81, Spring 2018).
“Our initial goal is to achieve accurate representations of our samples. But, in the long term, if we collect enough information, we may be able to rebuild the tumours in virtual reality, allowing scientists to ‘walk into’ them and programme how they would respond to perturbations in TME,” says Hannon. Eventually, he adds, some version of the model could become a new pathological tool in the clinic to model treatment options for individual patients.
Undoubtedly, the tumour microenvironment holds the secret of many current mysteries around cancer that have eluded scientists. It could explain phenomena such as why breast cancers always metastasise to bone and not the liver, why some cancers suddenly regress, why micrometastases can lie dormant for many years before coming back as metastatic cancer, and why autopsy studies reveal that many apparently healthy people who have died of unrelated causes harbour small cancers. “If you look at what actually kills people with cancer, it isn’t the cancer cells themselves, but the ‘cancer swamp’ created by the TME,” says Pienta. “What people die of is the swamp gases, things like cytokines and chemokines, released by the TME that lead to cachexia and blood clots.” Since the overriding aim is to avoid death, greater understanding of the TME is of paramount importance.
The microbiome battlefield
Jennifer Wargo, from the MD Anderson Cancer Center, in Houston, Texas, believes differences between individual microbiomes explain why only around one in five patients respond to checkpoint inhibitors, such as nivolumab, pembrolizumab and ipilimumab. Wargo’s research group focuses on the genetics of melanoma and other cancers with the goal of understanding what allows them to grow, spread and evade the immune system. In studies she has shown that melanoma patients with more diverse gut microbiomes and increased concentrations of the Ruminoccaceae family of bacteria have better treatment responses (Science 2018; 359:97‒103).
To investigate causal mechanisms, Wargo transplanted faecal microbiomes from responding and non-responding patients into germ-free mouse cancer models. She found that mice receiving transplants from responding patients had significantly reduced tumour growth and higher densities of beneficial T cells, lower levels of immune suppressive cells and better outcomes when treated with checkpoint inhibitors than those receiving transplants from non-responding patients. “We think having the right bugs leads to the production of key metabolites, like short chain fatty acids that promote immune function,” she says.
A different mechanism may account for an association found between having the ‘wrong bugs’ and developing colorectal cancer. According to a study conducted by Paul O’Toole, professor of microbial genomics at University College, Cork, in Ireland, the microbiomes of people with colorectal cancer are distinguished from healthy controls by having a greater abundance of bacteria that have previously been reported as oral pathogens, including Peptostreptococcus, Porphyromonas and Parvinmonas. “Oral bacteria have different properties to gut bacteria, including secreting biofilms that allow them to adhere more efficiently to mucosal surfaces and remain in place longer,” says O’Toole. The result of this greater staying power, he argues, is that these bacteria are more likely to promote localised inflammation, which is “a final step in the development of cancer”.
Potential angles of attack
For people embarking on checkpoint inhibitor treatment, enhancing their impact would be very valuable. Defining what is meant by a ‘good’ microbiome in that context represents the greatest challenge, with no single magic bullet converting patients from responders to non-responders. To overcome this, Wargo hopes to start clinical studies by the end of 2018, where melanoma patients who do not respond to PD-1 based immunotherapy will be implanted with faecal transplants from those who do.
To modify the microbiome to protect against colorectal cancers, O’Toole believes that tweaking it through adopting healthy diets rich in fibre is the way to go. “The healthy diet microbiota disease paradigm suggests diets rich in fibre promote a wide range of gut bacteria preventing colonisation by oral bacteria, and these bacteria also produce short chain fatty acids (such as butyrate) that reduce inflammation,” he says. O’Toole has further suggested that microbiome testing could be used to identify people at increased risk of developing certain cancers and for early detection.





Leave a Reply