
New knowledge favours promoting peace over waging war
The world spends billions on trench warfare with cancer and makes slow progress with heavy collateral damage. New knowledge about the process of carcinogenesis and tumour growth is now fuelling calls for a change of strategy to focus on containing potential trouble and keeping the peace.
Prevention is better than cure, and nowhere is that more true than for cancer, where cures are not always attainable, treatment not always affordable, and the short- and long-term side effects can be severe.
In light of what we now know about cancer’s extraordinary ability to mutate in all directions and to outwit every therapy we come up with, strategies aimed at intervening as early as possible in processes that lead to tumour formation make perfect sense.
Yet research into preventing cancer has traditionally been relegated to the lowest priority, both in terms of public health initiatives and the sort of medical prevention strategies that have been successful in cutting heart disease.
Research into all aspects of cancer prevention typically receives only between 2% and 9% of the total cancer research spend (Molecular Oncol 2008, 2:20–32). The number of people involved in the medical prevention effort is tiny – almost non-existent in Europe – and has barely increased since pioneers like Michael Sporn, Professor of Pharmacology and Medicine at Dartmouth Medical School, in New Hampshire, began investigating chemoprevention back in the early 1970s.
Two profound developments, how-ever, may now be coming together to give prevention its big moment. The first of these is the growing recognition, in the words of the World Oncology Forum (worldoncologyforum.org), that current strategies for controlling cancer are demonstrably not working.
New treatments – the fruits of multi-billion dollar research efforts – are hugely complex, have limited efficacy and come at a cost that renders them unsustainable even in richer coun-tries. Middle- and low-income countries trying to get to grips with the disastrous rise in cancer among their citizens are focusing hard on prevention. It is no surprise that China leads the world in population-based prevention studies; with more than three million new cancer cases every year, focusing resources on treatment rather than prevention simply isn’t an option.
The second development is the emergence of a more holistic, systemic understanding of the nature of cancer, where the focus is less on the mutated cancer cell itself and more on the role played by the body’s own physiological processes in turning normal cells into cancer cells and enabling those cancer cells to thrive and spread.
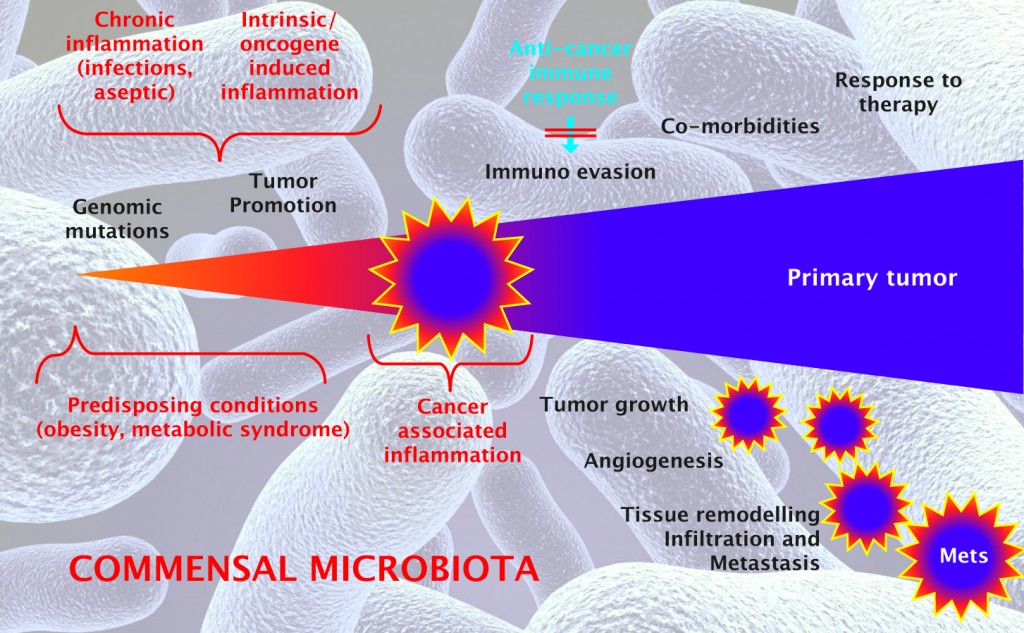
Explorations of the role of the tumour “micro-environment” in tumour formation and growth are expanding into a new and fascinating field that is examining the role played by our microbiota – the trillions of microbes, bacteria and fungi that live inside us.
Our immune response, inflammatory response, and angiogenic response (building new blood vessels) are all under the spotlight, together with a range of hormones that are related to nutrition.
Step by step, researchers are starting to reveal the mechanisms behind associations that have long been docu-mented at an epidemiological level, linking cancer risk with diet, exercise, and obesity. In doing so, they are strengthening the evidence-base for strategies aimed at intervening to prevent, suppress or reverse the carcinogenic process.
Prevent the preventable
This exciting time of joining dots and fitting together puzzle pieces formed the context of the third meeting of the World Oncology Forum, which took place in Milan in October 2015, under the title Prevent the Preventable.
For the European School of Oncology, who convene the Forum, it was a return to their philosophical roots.
ESO’s founder, the surgeon Umberto Veronesi, best known for pioneering breast conserving surgery and adjuvant chemotherapy, was an early advocate of developing preventive therapies to avoid the aggressive treat-ments that are needed for established cancers.
ESO has long been supportive of the efforts of people like Sporn in the US and Andrea DeCensi, a self-styled ‘heretical oncologist’ in Genova, Italy, who has pioneered a methodology for trialling “repurposed” drugs in a preventive setting.
It was satisfying for ESO, therefore, to host a Forum that positioned this traditionally marginal field of preventive therapies at the centre of a dis-cussion involving leaders in the field of cancer epidemiology on the one hand and biology on the other.
As with the previous World Oncology Forums, this was not an academic exercise. It was about coming up with recommendations on the role prevention, including medical prevention, should play within wider policies and strategies for tackling the rising tide of cancer.
What’s new?
Giorgio Trinchieri, head of the US
National Cancer Institute’s Cancer and Inflammation Program, presented what could come to be seen as an “ah-ha!” moment in expanding our understanding of the link between diet, lifestyle, environment and cancer risk.
Meet the commensal microbiota. These are the bacteria, fungi and vir-uses that live in our body all the time and don’t do damage, Trinchieri explains. They are on all the surfaces of our body that communicate with the outside environment: the skin, respiratory tract, gastrointestinal tract, urogenital tract. They are most abundant in the gastro-intestinal tract, particularly the colon.
These vast colonies comprise up to five times more micro-organisms than we have cells in our bodies, and include 1000–2000 different species. They can be highly responsive to changes in diet, environment and other lifestyle factors, and it turns out that they play a very important role in regulating or modulating numerous physiological functions.
Some of these functions, notably the inflammatory and innate adaptive immune response, play a key role in determining whether or not a cancerous mutation will go on to proliferate, thrive and metastasise. The really big surprise is that this regulatory role is not confined to the locations where these micro-organisms live: “If you have an inflammatory viral infection in your lung, the immunity in the lung will not be effective unless you have the presence of gut microbiota,” says Trinchieri.
The extent of the role of the microbiota in cancer has been convincingly demonstrated in a number of ways. With the first tumour oncogene, the rous sarcoma virus, it was shown that if you inject a virus into an adult bird you will get a tumour at the site of the infection or other parts of the body where it induces inflammation. But if you inject it into a germ-free embryo, you don’t get any tumour. Even if the cells where it was injected show a transformed phenotype, they won’t grow in the embryo without the right microenvironment, Trinchieri says.
“It could be the microbiota [acting directly] or it could also be that you need inflammation damage for the virus to induce a tumour, and the microbiota clearly plays a role in that. If it is sterile nothing happens. The virus puts the oncogenes in the cells but the cells don’t grow.”
Inducing a highly aggressive tumour into germ-free mice, by injecting mutated KRAS cells and knocking out their p53 tumour suppressor gene shows a similar result, he adds – virtually no tumour growth.
This is not to say that the mutated cell itself is irrelevant, Trinchieri stresses, but it does show the importance of the microenvironment, and the potential for intervening in the processes that regulate it.
“There’s no doubt a tumour is a genetic alteration of normal cells and a lot of money has been spent understanding the oncogene, the tumour suppressor gene, genotyping of tumours to find the different mutations. But a mutated cell would never be able to grow and metastasise if the seed doesn’t find the right soil, the right tissue, and right
micro-environment, particularly the right level of inflammation and innate adaptive immune response in the microenvironment that would allow this mutated cell to grow and form a tumour.”
Piecing the picture together
Inflammation and immune response
What we are learning about the role of the microbiota throws new light on an existing body of knowledge about the role inflammation and the adaptive immune system play in carcinogenesis and tumour development, some of which dates back to the earliest days of medicine.
As Trinchieri points out, similarities between cancer and inflammation were noted by the Greek physician, Claudius Galenus, almost 2000
years ago. Virchow, the “father of
modern pathology”, suggested in 1863 that cancers may grow at the sites of chronic inflammation. And twenty
years ago Harold Dvorak, now Professor of Pathology at Harvard, observed that inflammation and cancer share some basic developmental mechanisms (angiogenesis) and cells (lymphocytes, macrophages, and mast cells), and that tumours act like “wounds that do not heal”.
The key here is the word “chronic”. One of the lessons learnt in the painful and rocky road to developing the first effective immunotherapies is that there are two types of inflammatory responses.
Acute inflammation induces a strong active immune response, which can be harnessed to fight cancer. Chronic inflammation, by contrast, induces a different response, which actually promotes tumour growth, suppresses the immune response and favours metastasis.
This explains the reduction in many types of cancer seen in people who have taken low-dose aspirin, which acts in part as an anti-inflammatory, over a period of many years.
It also suggests a likely involvement of the microbiota, and its role regulating inflammatory and immune responses, in the mechanisms linking certain diets, environments and lifestyles with a raised risk of cancer. This in turn opens up possible new strategies for prevention.
We can alter some of these factors with diet and lifestyle changes or
become more sophisticated in directly altering and affecting certain microbiota species, says Trinchieri.
The cancer detectives of Linxian
The first strong evidence that nutritional interventions can not only significantly reduce the risk of developing and dying of cancer, but can actually reverse precancerous lesions, was generated by the Nutritional Intervention Trial. This was a Chinese population-based study, initiated in 1985, which looked at the impact of a range of vitamin and mineral supplements on rates of oesophageal and other upper gastrointestinal cancers, which are a particular problem in China.
You-Lin Qiao, head of the Depart-ment of Cancer Epidemiology at
China’s National Cancer Centre, presented some of the key findings, which included a 23% reversal rate of atypical oesophageal dysplasia, and a reduction in oesophageal and gastric cancers of 13% and 21% respectively. He also talked about the evidence being
generated by numerous subsequent and ongoing population-based trials, where China continues to lead the world.
Many findings are not directly trans-ferable to other parts of the world – evidence from countries where a full range of fresh food is always available suggests that it is a healthy balanced diet rather than dietary supplements that make the difference.
But some is of relevance, such as the importance of getting the diet right at a young age. The Chinese data will contribute to a broader picture in the context of findings generated in populations with different environments, lifestyles and genetics.
More important, perhaps, has been the proof of principle of this approach to cancer prevention. The meticulous epidemiological research that provided the scientific rationale for the Nutritional Intervention Trial started back in 1959, when China was among the poorest countries in the world. Immortalised in the 1972 BBC documentary, ‘The Cancer Detectives of Linxian’, this low-tech approach, which drew on traditional Chinese medicine and focused on changing behaviours, is to this day held up as a template for cancer control, by the WHO among others.

‘Meet-in-the-middle’ studies
Relying on population-based epidemiology to inform preventive strategies does, however, have its limits, as Paolo Vineis, Chair of Environmental Epidemiology at Imperial College, London, pointed out.
Vineis plays a leading role in the 500,000 strong European Prospective Investigation into Cancer and Nutrition (EPIC) study, which over the past decade has generated data indicating, for instance, that fibre and fish in the diet are protective against cancer risk, while red and processed meat significantly raise the risk.
He came to the Prevention Forum directly from participating in the expert meeting of the International Agency for Research on Cancer that evaluated processed red meat as carcinogenic to humans (Group 1), and unprocessed red meat as “probably” carcinogenic (Group 2A).
Vineis says that the problem with observational epidemiology is the difficulty in singling out different risk factors, which occur in patterns. “Disentangling single risk factors from others is not always straightforward.”
Vineis and his group at Imperial College are trying to pinpoint mechanisms that could give biological plausibility to the epidemiological findings and provide markers that could be used in prevention trials.
They call this “meet in the middle” studies, because they are looking for biological markers that are associated with both the disease and with particular diet-ary exposure.
“We did a small study using metabolomics. We looked at breast cancer and colon cancer in EPIC Italy, and we found eight metabolomic signals, or ‘features’, associated with colon cancer. Out of those signals associated with colon cancer, four were associated with dietary fibre. These were statistically significant after correction for multiple comparisons.
“One of these indicates a possible link with gut microbial fermentation of plant phenolics in the colon, so there is some biological plausibility there.”
This points the finger at the composition of the colonic microbiota, which would fit in with other evidence on colon cancer, including studies showing that two families of bacteria commonly found in the colon – bacteroides and clostridium – increase the incidence and growth rate of colonic tumours induced in animals.
This opens possibilities for preventive strategies that intervene directly, rather than through diet, to modify the microbiota, as Trichieri is suggesting.
A surprising role for nutritionally related hormones
Rising obesity rates are one of the big drivers of the escalating rate of cancer. Understanding the “bit in the middle” that links weight with cancer, with a view to learning how to lower the risk, is a challenge that Michael Pollak, Director of the Division of Cancer Prevention at McGill University, in Montreal, has made his own.
Speaking at the prevention forum, he talked about a surprising picture that is emerging, which implicates nutritionally related hormones – insulin, insulin-like growth factors, and many more – as the link.
“The more food you eat the bigger your insulin secretion, and cells are informed that it’s OK to use energy for proliferation and growth or storage,” Pollak explains.
He makes a link back to Thomas Beatson, the pioneering British doctor who made the connection between the ovaries and breast cancer, at the end of the nineteenth century. “The dietary energy supply influences some tumours by influencing the hormonal environment rather than the energy available to the tumour. The effect of macronutrient intake on cancer biology is just another context of hormonal dependency of neoplastic cells,” he says.
This has important implications for prevention, because it means that, essential though it is to eat moderately and exercise, this may not always be enough, and there may be other ways to intervene directly on this group of hormones, using diabetes as a model.
Experiments on mice show that prostate cancer grows faster when they are fed on a ‘junk food’ diet. However, if you then induce type 1 diabetes, the growth rates slows. “The glucose is very high, but insulin is low. It’s not the glucose they need. It’s the insulin,” says Pollak.
He is interested in the antidiabetic drug metformin as a potential preventive agent for people at high risk of insulin-related cancers. The safety and side-effect profile of metformin is well known, and use of the drug has been linked with a very significant reduction in cancer incidence in a major observational cohort study (Diabetes Care 2009, 32:1620–25).
Pollak accepts the study may be flawed and needs confirmation; however, he argues that there is a strong rationale for such a preventive effect. “Metformin acts on mitochondria to inhibit energy production. It gets to the liver and the liver cells feel energy stressed and keep the glucose for themselves. Glucose levels fall, so insulin levels fall, and insulin dependent cancers could then be hit, provided the magnitude of decline is sufficiently large.”
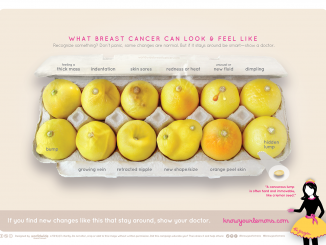
Change the strategy

The principle of preventive therapies is now widely accepted – and approved by the FDA – specifically for hormonal therapies in people at high-risk of breast cancer. The strong consensus at the forum was that extending this principle to other agents and other cancers is now a strategic imperative.
The evidence for the impact of aspirin, for instance, in reducing the risk of colon cancer through its anti-inflammatory effect, is undeniable (Ann Oncol 2015, 26:47–57), and demands urgent research to define who will benefit and the optimum dose and duration of treatment.
More generally, there is now a compelling case for paying more attention to denying precancerous lesions the environment they need to become cancerous and to thrive and spread.
The NCI’s Giorgio Trinchieri, put it this way. “When we look at cancer in the organism, it is like an invasive plant that grows in the wood and destroys the wood. We need to decide how to deal with that. The traditional way – the medicine battlefield strategy – is to go out with very strong weapons. We destroy the tumour, the pathogens, but we also destroy the body by doing that.”
The ideal, he argues, would be to see medicine more in terms of managing the environment. “We need to look at the habitat, the tumour, the microenvironment, the whole organism, and use prevention if we can, and the very targeted removal of the invasive species, and restore and promote the native species, thus re-establishing the homeostatic ecology of the healthy organism.”
While public health prevention measures will be essential to managing this environment – promoting healthier lifestyles, reducing exposure to carcinogens, e.g. through vaccination programmes against cancer causing viruses – preventive medical interventions could also play a vital role.
“By itself, a better lifestyle is not sufficient to solve the cancer problem; if the genetic burden is high enough, carcinogenesis results in invasive cancer, despite living an optimal lifestyle,” argues Michael Sporn, and he points to the example of BRCA mutation carriers.
“What good is it for a young woman to know that she has a BRCA mutation if all that we can offer her is bilateral prophylactic mastectomy, with the extra bonus of an oophorectomy? What is critically needed right now in the total effort to prevent cancer,” he argues, “is the development and eventual clinical testing of new, safe, and effective chemopreventive drugs. Big Pharma is not interested in such an approach, and woe-fully little is being done in this area.”
This is hardly surprising coming from Sporn, who has been arguing this line for most of his career. What has changed is that his views are now finding support among some leading pioneers in cancer genomics, including Bert Vogelstein, Director of the Ludwig Cancer Research Centre at Johns Hopkins, who is equally vocal in calling for a change in strategy.
In a high-profile piece in Science magazine (2013, vol 339, pp 1546–58), Vogelstein argues that, “The focus on curing advanced cancers might have been reasonable 50 years ago, when the molecular pathogenesis of cancers was mysterious and when chemotherapeutic agents against advanced cancers were showing promise. But this mindset is no longer acceptable.”
The experts gathered at the third World Oncology Forum, agree. They will be launching an appeal calling on policy makers and opinion leaders to provide leadership and resources to promote the development and implementation of new evidence-based strategies aimed at cancer prevention, risk assessment/early detection and early intervention, and tailored to specific communities, cancers and populations.
Tabella
The World Oncology Forum
The Prevent the Preventable forum was the third gathering of the World Oncology Forum (worldoncologyforum.org), which is convened by the European School of Oncology, in conjunction with The Lancet.
The first World Oncology Forum – a gathering of 100 international experts and journalists held in 2012 – was called to evaluate progress in the so-called “War on Cancer”. It called for a major change in strategy and launched the 10-point Stop Cancer Now! Appeal, aimed at governments, policy makers and leaders of the cancer community, which was published on World Cancer Day 2013 in The Lancet and leading newspapers across the world, inluding Le Monde, El País, the International Herald Tribune, the Neue Zürcher Zeitung and La Repubblica.
Tackling cancer is also being flagged up as a key international policy issue by The Economist, which has launched a series of conferences on the topic, starting in Boston last September, then London in October, with a third set for March 2016 in Singapore.





Leave a Reply