
Looking for anticancer activity among off-patent drugs that are already approved to treat other conditions might seem a sensible way to speed up access to affordable new therapy options. Linda Geddes asks how such a strategy can work in practice, when the drugs are so cheap but the cost of approval is so high.
When Pan Pantziarka’s teenage son, George, failed to respond to standard treatment for osteosarcoma, Pan did what many scientifically literate friends or relatives would do in this situation: he started searching Pubmed and reaching out to clinicians in the hope of finding an alternative.
The suggestions they came up with – things like the anti-diabetic drug, pioglitazone, and the non-steroidal anti-inflammatory drug, celecoxib – were widely used for other indications, had shown some anti-cancer activity, and even produced some promising phase I or II trial results. Yet for one reason or another they had been abandoned as oncology drugs.
It’s impossible to know if they would have changed George’s fate; he never got to try them because his oncologist was resistant to the idea. But even after his death in April 2011, the idea of repurposing drugs stuck with Pan. Today he works for the Belgium-based Anticancer Fund (anticancerfund.org), co-ordinating the Repurposing Drugs in Oncology (ReDO) Project, which seeks to identify existing drugs that could be turned into cancer treatments – either as additions to existing oncology drug regimens, or in combination with multiple repurposed drugs.
It’s an approach that’s starting to garner interest from others, besides desperate cancer patients. The cost of new cancer drugs is exploding. In 2013, $91 billion was spent on oncology drugs worldwide – almost double the GDP of Bulgaria. In 2014, no cancer drug was approved that cost less than $100,000 for a course of treatment, and in 2015 eight drugs cost more than $120,000. “If the current trajectory continues, then by 2030, we could see the first $100,000 per month treatment,” says Paul Cornes, a Bristol-based oncologist and part of the steering group for the European School of Oncology’s Working Party on Access to Innovation in Cancer Treatment. “The cost of cancer drugs has been rising five times faster than any other medicine. We’ve realised the power of targeted precision drugs, and they are expensive to make. But at some point this will bankrupt health systems.”
Repurposing the large arsenal of approved, non-cancer drugs might therefore seem like an attractive solution. Many of the drugs identified by the ReDO project, and other repurposing initiatives, are cheap and already have a large body of safety data. Assuming that they are effective, this should hasten the approval process and provide patients with more new options, sooner. But are they? This question is proving perplexingly difficult to answer – precisely because they’re so cheap and widely available.
Cancer drugs cost crisis
The current crisis in cancer drug costs has been building for some time. Aging populations mean more cancer, and in today’s world, patients demand access to the latest and very best treatments. But developing these drugs is expensive: the current cost of bringing a new cancer drug to market is estimated at $2–4.5 billion, including all the failures along the way. “We now believe that 90% of the cost of developing medicines isn’t the high-tech lab work, it is the clinical trials,” says Cornes. “But one reason why we’re having to run very large trials is because we’re looking to statistically prove small differences.”
The sad truth is that, in spite of all this investment, the improvement in survival yielded by targeted therapies is modest. “Some of the newer drugs are extremely expensive, but don’t bring very much,” says Mario Dicato, an oncologist at the Centre Hospitalier de Luxembourg, and co-chair of the ESMO World Congress on Gastrointestinal Cancer. He cites pancreatic cancer as one example. The addition of erlotinib to gemcitabine treatment around a decade ago increased costs by approximately $16,000 per patient, yet boosted median survival by just ten days. “Everybody uses this drug – including me – but in the end it’s just ten days, and in those patients where it doesn’t work you get the side effects,” Dicato says. “It’s a poor trade.”
That’s not to say oncologists should give up on targeted therapies. It is likely these will eventually be made to work better, and the costs will come down, but that is going to take time and investment. “In the meantime, we need to learn how to use these drugs to make big differences and not little ones,” says Cornes.
Part of the problem stems from our incomplete understanding of cancer biology. It’s becoming increasingly apparent that there are far more cancer-initiating and driving DNA mutations than we anticipated – a complexity that’s also reflected in the tumour microenvironment, says Francesco Bertolini, director of the Laboratory of Haematology–Oncology, at the European Institute of Oncology in Milan. This makes combinatorial approaches essential – at least in advanced tumours – and yet, “the cost of new drugs would no longer be sustainable if we use only on-patent drugs in combinatorial therapies,” he says.
Possibly though, we’ve missed a trick, says Cornes: “The question is, in our rush to commercialise targeted therapies, have we overlooked opportunities to improve cancer outcomes that would be much more cost effective?”
Repurposed drugs could be one such opportunity. “My opinion is that we could actually get more if we stopped putting all our efforts into the new, and spent more time tinkering with what we already have,” says Gauthier Bouche, medical director of the Anticancer Fund.
Tinkering with what we have
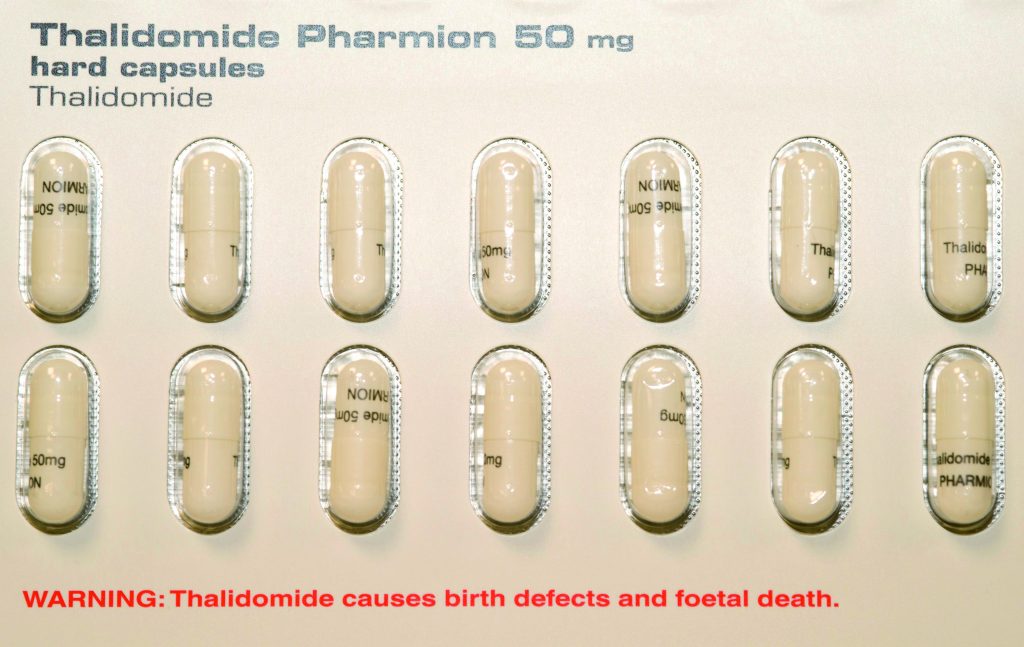
One of the earliest examples of a successfully repurposed drug is thalidomide. Originally developed as a sedative in the 1950s, it was later used to treat morning sickness in pregnancy – until babies started being born with severe deformities. Its resurrection came in the late-1990s, when clinicians at the University of Arkansas set up a trial of thalidomide in 84 multiple myeloma patients who had failed to respond to therapy, and were therefore expected to die within months. Twelve months later, 48 of them were still alive, a quarter of them event-free (NEJM 1999, 341:1565–71). Even so, thalidomide is an unpleasant drug, and treatment with it carries a high risk of neuropathy, so researchers started to develop less toxic analogues. One of them was lenalidomide, which today generates around $4 billion in worldwide sales per year.
Possibly there are other effective cancer medicines sitting undiscovered on pharmacists’ shelves. So far, the ReDO project has compiled a list of more than 70 non-cancer drugs for which there is some pre-clinical and clinical evidence of anti-cancer action, and published detailed reviews on the six most promising through the open-access journal ecancer. They are: the anti-helmintic drug, mebendazole; the antacid, cimetidine; the angina drug, nitroglycerin; the broad-spectrum antifungal agent, itraconazole; the antibiotic, clarithromycin; and the NSAID, diclofenac. As well as identifying these drugs, ReDO is working with clinicians in different countries to design and fund more advanced clinical trials. Trials are already underway of nitroglycerin in non-small-cell lung cancer, perioperative ketorolac in high-risk breast cancer, and fluvastatin-celecoxib in optic nerve gliomas.
Elsewhere, large clinical trials are investigating the potential of aspirin, the beta-blocker, propranolol, and the antidiabetic drug, metformin, in a range of common cancers, including breast, colorectal, and prostate cancer – as well as less common ones, such as angiosarcoma (see, for instance, Drug repurposing in oncology, CancerWorld May–July 2016).
Admittedly, few of these drugs are being proposed as an alternative to targeted therapies. “We don’t expect to find a magic bullet, so we are primarily looking at combinations – either with chemotherapy and standard therapies, but also combinations of repurposed drugs,” Pantziarka says. Many of these older drugs hit multiple targets, and because of this, clinicians often regard them as dirty drugs – and yet this could be their strongest suit. Take the painkiller, diclofenac: “It is a great anti-angiogenic drug, it modulates the immune system and it has some effect on sensitising the body to chemotherapy and radiotherapy,” says Pantziarka. “It does multiple jobs that are of interest to cancer, and it does it in one tablet.”
Patient-centric not patent-centric
It’s a more patient-centric approach than the one being taken by many pharmaceutical companies, which identify a molecular target and then tailor their research to the approval of the drug they’ve developed to block it. This in itself may boost the chances of success, says Bertolini: “The drug-centric approach selects the patients according to the needs of an approval process, the patient-centric approach combines drugs independently from the presence of a patent pending.”
In some cases, the idea is simply to see whether giving one of these drugs post-surgery could reduce the risk of recurrence. Add-Aspirin, a randomised clinical trial taking place in the UK and India, is currently recruiting 11,000 participants to help find out whether regular aspirin use after treatment for an early stage breast, colorectal, gastro-oesophageal or pancreatic cancer can delay or prevent cancers coming back.
However, some non-cancer drugs are being investigated precisely because they have the potential to hit specific targets, such as the STAT3 pathway, which often becomes activated in lung cancer patients taking an EGFR inhibitor like gefitinib (Iressa). “We know that when you are targeting one molecular pathway, the cells almost immediately activate parallel signalling pathways and develop mechanisms of resistance,” says Niki Karachaliou, Director of the Medical Oncology Department (Rosell Oncology Institute) at the University Hospital Sagrat Cor in Barcelona. “We are trying to understand what other pathways are being activated, what we need to target, and we’re then screening for compounds that have been reported to hit that target.” One STAT3 blocker they’ve identified is the anti-helmintic drug, niclosamide. Another is the diabetes drug, metformin.
“For a pharmaceutical company, it may be more appealing to search for a new drug from the beginning; however, patients want faster solutions,” Karachaliou says. “If the drugs are already used for other indications, we know the side effects, we know the doses; there are fewer uncertainties.”
All the same, it’s unlikely that AstraZeneca, which owns the patent on Iressa, would fund larger trials of metformin or niclosamide – even if they made Iressa work more effectively (its patent is due to expire next year). Instead they’re more likely to focus on their own next-generation antisense oligonucleotide inhibitor of STAT3, which is already in the pipeline.
This is a key problem facing those involved in drug repurposing. “A drug company that invests money in supporting a clinical trial is not guaranteed to recoup that money if the trial is successful, because some other manufacturer could come in and sell the same drug at a lower price,” says Pantziarka. Not only do those researchers who choose to go it alone have to secure funding to run a clinical trial, they will often have to buy the drugs and package them up themselves. Then, if the trial is successful, they will need to find a way of funding the application for a new license. The costs of licensing a drug in Europe are between €83,700 and €278,800 – plus an annual cost of €100,000 to maintain market authorisation.
Who will pay for market access?
“The question is who actually could and should pay for the work that would be required to get a license and market a drug for oncology,” says Nigel Blackburn, Cancer Research UK’s director of drug development, who is currently involved in phase I trials of a repurposed anti-inflammatory drug. “Pharmaceutical companies have to turn a profit at the end of the day, and if there is no prospect of them getting a return on that investment they won’t touch it. Meanwhile, there is no movement that I know of in any government or regulatory body to do anything about this: it just doesn’t seem to be on their radar.”
Possibly charities like Cancer Research UK could step into the breach; it is the biggest supporter-led cancer charity in the world, and spent around £435 million last year on research. But the extremely high costs involved in running clinical trials make this unlikely, Blackburn says: “A phase II trial will typically cost £20–30 million [€23–35 mn], and a phase III trial, £50–70 million [€58–81 mn]. We could do it, but we would have to stop an awful lot of the other things that we do.”
Another possibility, suggested by Bertolini at the EIO, would be public–private initiatives involving governments, health insurers or foundations. Using this model, governments or health insurers could potentially recoup their investment by lowering the overall cost of cancer treatment if the repurposed drug was shown to be effective in advanced disease or in preventing cancer recurrence. For foundations that focus on rare cancers, repurposing existing drugs may be the cheapest way to provide their patients with new treatments.
Who will champion their use?
In some cases, though, these drugs have been through extensive trials, show clear benefits – and yet they’re still not being used, because there is no-one to champion them. Take cimetidine, a patent-expired anti-ulcer drug. Five randomised trials have shown that adjuvant cimetidine – either around the time of surgery for colorectal cancer, or in the period afterwards – reduces the risk of death from recurrence, and a Cochrane meta-analysis also confirms this. But having scrutinised European, American and Japanese guidelines for the treatment of colorectal cancer, Cornes says he can find no mention of this data.
“Cimetidine is a drug whose side effects are known, it is inexpensive, and you can buy it over the counter in the pharmacy,” he says. “It fundamentally raises a question about what level of proof we want to accept in our next generation of guidelines for colorectal cancer.”
There’s also the question of what clinicians should tell their patients. Not every doctor is happy to prescribe drugs off-label – they may come under pressure not to from their peers or managers, or find themselves in trouble if something goes wrong. But in the absence of funding to run large randomised clinical trials or apply for new licenses, drugs repurposers and oncologists find themselves in a Catch-22 situation.
Some maintain that further data are necessary before drugs can be recommended to cancer patients – even ones as widely used as aspirin. Others, like Cornes, believe an honest conversation is the best approach: “We know that our patients are desperate for help, and that perhaps a third to a half of Europe’s cancer patients take unproven therapies alongside the therapy we give them,” he says. “Why don’t we give them the opportunity to take proven but unlicensed therapies, and discuss our uncertainties with them about the exact dose and schedule – things that a licence would force you to have?”
Most of all, however, Cornes believes the time has come for a debate about what constitutes good value in oncology. Is it pouring billions of dollars into producing targeted therapies that society then can’t afford to prescribe? Or is there value in revisiting the arsenal of drugs we’ve already got and finding smarter ways of using them? This principle doesn’t only apply to bathroom cabinet stalwarts, like painkillers, and to diabetes drugs, but to older cancer drugs as well. The STAMPEDE trial revealed that adding cheap, patent-expired doce-taxel to standard hormone therapy for prostate cancer added, on average, ten months to men’s lives, compared to standard treatment alone. And in the case of those whose cancer had metastasised, adding docetaxel increased survival by an average 22 months (Lancet 2016, 387:1163–77).
Although tinkering may be less financially rewarding from a commercial perspective than engineering new drugs, both are necessary, and even complementary, says Bouche, from the Anticancer Fund. “When you look at the history of medicine, tinkering is found at the early stages of multiple major therapeutic advances such as surgery, psychological interventions, hygiene, vaccines – but also drug development,” he says. Tinkering could also be part of the next big advance in cancer treatment – if we let it. But it needs to be incentivised.
Getting new options into the clinic
Cancer patients who no longer respond to recommended treatments need affordable new options now.
Many existing drugs that are off-patent, and whose side effects are already known, are likely to offer benefit to certain cancer patients, based on their mechanism of action or observational data or even multiple clinical trials.
Thalidomide (in multiple myeloma) and docetaxel (in advanced prostate cancer) are examples of off-patent drugs that have shown benefit well beyond what most novel drugs offer, and at a fraction of the price.
However, the low price of off-patent drugs, and lack of exclusivity, means that getting them approved for new indications is commercially unviable.
Exploiting the potential of repurposing off-patent drugs for use in cancer may require new incentives and a greater acceptance of uncertainty within the context of shared decision making.




Leave a Reply