The world is experiencing new and powerful forces in global health, from the Sustainable Development Goals, and ‘grand convergences’ to what is now the central totem in global health – universal health coverage. For cancer control, context is everything, and it still needs to find its place within these wider agendas.
Richard Sullivan is Director of the Institute of Cancer Policy and Conflict and Health Programme at Kings Health Partners Comprehensive Cancer Centre.
He will address a specific challenge in global cancer care in each issue of Cancer World.
Cancer is a very new addition to global health, which has been built almost entirely on the platforms of infectious disease, including HIV/AIDS, child and maternal health and other health aspects of the development agenda. Infectious diseases have been the main drivers of global health, where concepts such as immediate good and disease eradication have been powerful motivators for action and funding.
The problem is that cancer doesn’t score so highly on either concept, because it is as much about control as cure and outcomes are a complex convergence of multiple different factors. So while we in the cancer community might understand how things work, to outsiders – even other healthcare professionals – the treatment pathways are a bewildering black box.
Many countries already struggle to provide the very basic packages of health services. Adding cancer care systems in the context of other global health goals can seem like a bridge too far, particularly given that many countries are faced with having to deliver care for not only non-communicable diseases but all the ‘old’ enemies – continuing threats to maternal and child health, malnutrition and infectious diseases.
It’s now clear that disease eradication programmes, such as those for malaria, lymphatic filariasis, dracunculiasis, and onchocerciasis, are difficult and risky and will probably require a lot more effort, time, and money than initially expected. Between 1986 to 2015, for example, it cost an estimated $350mn to bring the number of dracunculiasis cases down from 3.5 million to under a thousand cases in three countries – Mali, Chad and South Sudan (NEJM 2013, 368:54–63).
This tells us two things. There’s still a huge amount of time and effort required to achieve the most fundamental population health interventions and, if Ebola and antibiotic resistance has taught us anything, you can never take your foot off the neck of infectious disease. In comparison, cancer control looks expensive and complex. And it is. The cost of basic treatment for a range of common cancers for the population treated in the dracunculiasis eradication programme would have been $118 bn. And that doesn’t include the capital costs.
National cancer control plans look rational and affordable in the context of high-income countries, but when it comes to countries with struggling economies, fragile public finances, poor social determinants of health, and multiple co-existing disease burdens from infectious diseases, chronic diseases and violence and trauma, national cancer plans are harder to deliver.
This poses a real challenge for how we approach global cancer control. The economic, structural and cultural reality for many countries is that the basic systems of healthcare, prevention and development are insufficient foundations upon which to build cancer control. Domestic funding and overseas development aid needs to be far more creative in the way that services are built up to provide the backbone for fully developed cancer care systems in the future. And this needs to be a public cancer system where private interests serve the greater good.
A public good
Global health is a public good and cancer control must be as well. All of this will require an open, two-way process of global cancer, engaging with and educating other parts of global health, be they development agencies such as USAID, or disease-specific groups such as HIV/AIDS, as well as a willingness of these other actors to positively engage with the complicated planning required for cancer control.
Cancer presents a challenge to the traditional structures and cultures of global health. Traditionally, norms and standards are set by the WHO, with operational responsibilities being a matter for gov-ernments or NGOs. But because of the breadth and depth of preventative measures and treatments needed for cancer control, many other actors are now setting norms and standards. This may be in site-specific areas, such as the Breast Health Global Initiative (Lancet Oncol 2014, 15:1421–23) or across domains, such as Global Surgery 2030 (Lancet Oncol. 2015, 16:1193–1224).
Some countries are developing their own quality standards, pathways and systems, such as the National Cancer Grid of India and the Chilean Cancer Forum (J Ind Soc Med & Paed Oncol 2014, 35:226–227). All this begs the question about long-term strategy and structures for supporting the development of affordable and equitable systems of cancer control within global health.
Progress outside high-income countries has been made through taking a wide and varied approach to building capacity and capability. There is no ‘one country’ model for building cancer systems, with much of the literature anyway a descriptive narrative rather than critical scrutiny. The real successes are heterodox solutions that build on political commitments in countries that are open, democratic and have transparent governance for sustainable health and development.
The tragedy of Libya and Syria, both of which had been held up as global models of how to deliver good health outcomes for low cost, is a cautionary warning about just how dependent global cancer control progress is on socio-political factors (J R Soc Med 2011, 104:490–492). Despite a lot of grand-standing no one ‘owns’ the cancer agenda in global health or has the universal solution to national cancer control plans. Instead we see a rich tapestry of creative ideas to tackle the problems we know exist and are becoming more adept at quantifying. It is easy to see how high income hegemony around global cancer, including some powerful vested interests in specific areas such as medicines, can distract us from looking beyond the usual suspects.
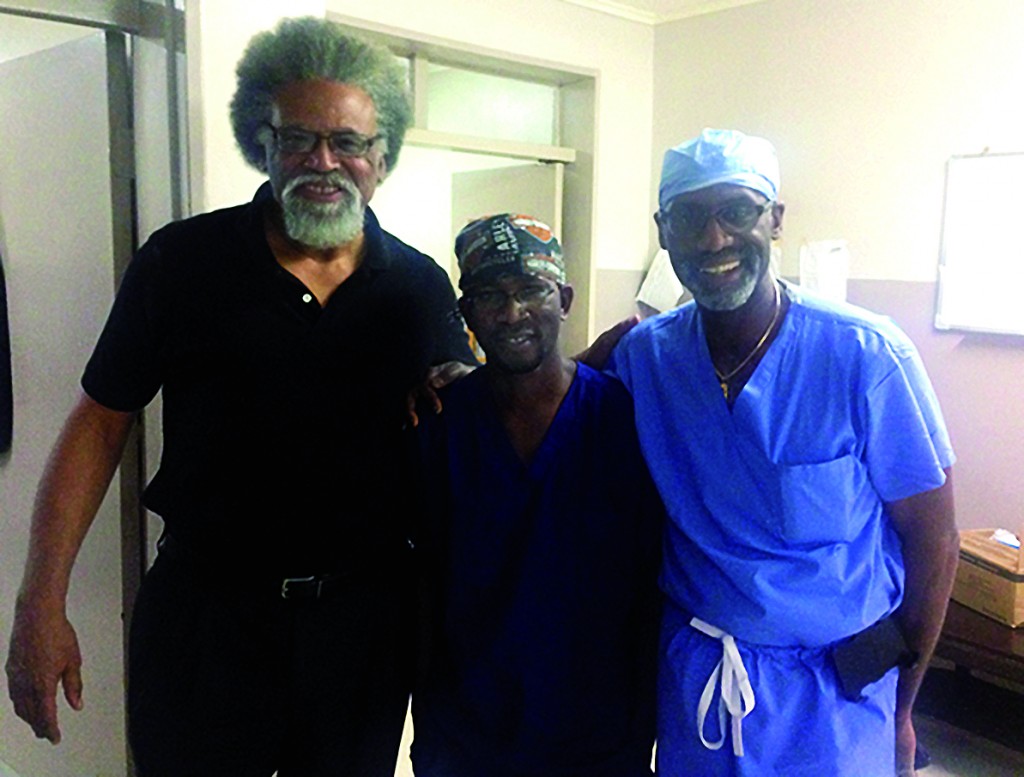
Long-term twinning partnerships between institutions have proved to be particularly effective for both adult and childhood cancers. A good example of the former is the AMPATH twinning model, between USA and Kenya (JCO 2016, 34:36–42); while the work done by St Jude’s Children’s Research Hospital (JCO 2016, 34:53–61) and by World Child Cancer (J Cancer Policy 2013, 1:e8–e19) are good examples of the latter. Building operational capacity using modality-specific approaches, as the Global Taskforce on Radiotherapy is doing, has also started to prove its worth as a focal point for action.
Much of the real progress, however, is being made through the collaborations between low- and middle-income coun-tries, such as the recent high-level partnership betwen India’s Tata Memorial Centre and Mongolia, and the work of University of Zambia–University of North Carolina to build up gynaecological-oncology surgery in other African countries such as Malawi.
Cuba’s contribution to medical training is also rarely recognised, even though workforce capacity in cancer care is the single biggest issue facing most countries and the Cuban medical schools have been superb at providing a global health workforce (The Lancet 2009, 374:1574–75). It is to these places and people that we should look for how we can achieve universal coverage of global cancer care.



Leave a Reply