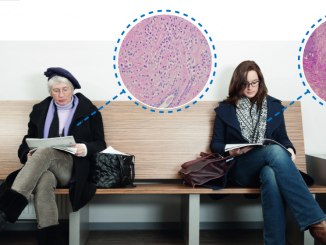
Most people carrying harmful BRCA mutations only find out after they are diagnosed with cancer, and often not even then. Population screening is costly and the results can be hard to interpret. But should we do it anyway?
TIrish Carlos walks through the door and recognises familiar faces. All looking and wondering. She gives them an inquisitive look… they must be pregnant. Why else would they be in a maternity hospital. But then again, why was she here?
Just a few months previously the dark-haired school teacher from the hilly seaside town of Cobh in Ireland had been standing on the same corridor holding a baby boy. This time excitement is replaced by anxiety. She sits down next to her husband Declan and waits to be called. The genetic service comes down from the Irish capital, Dublin, to the southern city of Cork once a month, and rents a room in the hospital. Trish has been waiting for eight months for today’s blood test.
They walk into the rented room. One like any other in the hospital, with a simple desk and examination bed. The geneticist explains that Trish is being tested for a mutation in a gene called BRCA1 that is linked to breast cancer. She goes through some of the symptoms and says that a mutation can give you a higher risk not only of breast cancer, but ovarian cancer as well.
They leave the room, walk down the corridor without talking and go straight to the car. Trish looks at Declan, dying to say…
Before she gets a chance, he says: “You don’t have to say it… I know what you’re going to say. You have all of them.”
“Yeah!” Trish knows he is talking about the symptoms, the little markers the geneticist had mentioned: early periods, abnormal growth of cells… She’d had a benign tumour removed, aged 13.
“Look it mightn’t be. It might be just coincidental.”
Trish is one of around 1,500 patients who are seen each year in Ireland for hereditary cancer. Most are related to breast cancer, says Andrew Green, director of Ireland’s National Centre for Medical Genetics. “The way people are identified is either because they themselves have had cancer at a young age or they have relatives at young age with breast or ovarian cancer.”
The BRCA genes are among the highest profile pieces of DNA that have been linked with cancer. Specific mutations in BRCA1 and BRCA2 genes increase the risk of breast and ovarian cancer. These genes produce tumour suppressor proteins, which help repair damaged DNA. If they’re not working properly, cells are more likely to develop genetic alterations that can lead to cancer. The harmful mutations are autosomal dominant, which means that you only need one copy of the faulty gene to have a higher cancer risk.
Currently, genetic tests are recommended in most countries when a family history indicates that harmful mutations could be present. Trish’s aunt Josephine had been diagnosed with ovarian cancer almost a decade ago, and because her sister had died of breast cancer, Josephine’s doctor had suggested BRCA testing. They discovered a BRCA1 mutation and recommended genetic testing to other members of the family. A few years later, this led Trish and her siblings to the maternity hospital.

Preventative measures can be taken by women with these faulty genes, which include regular breast screening, risk-reducing surgery and the use of cancer-preventing drugs. Actor Angelina Jolie, who has a BRCA1 mutation, highlighted risk-reducing surgery when she revealed that she had opted for a preventative double mastectomy, and more recently removal of her ovaries and fallopian tubes.
Six weeks later, Trish is back in the same room for her results. The geneticist opens the sealed brown envelope and says: “unfortunately, you have it” – a mutation in the BRCA1 gene, leaving Trish at very high risk of both breast and ovarian cancer. The geneticist is surprised that Trish isn’t more upset. “We had a feeling that I probably did,” she explains.
Her test result means that Trish is registered in the monitoring unit where she will have regular mammograms, ultrasounds, MRIs and blood tests. Abnormalities will be checked immediately in the hope that any cancer will be picked up and dealt with as early as possible. Down the line, preventative surgeries to remove the breasts and ovaries are also an option. “Do you have any questions?” The new mother sits there trying to take the information in. Is she being told that she could lose her ovaries, in of all places, a maternity hospital?
A failure of prevention?
If Trish had no suspicious family history, her mutation would not have been picked up unless she herself was diagnosed with cancer. The same would have been true for two of her sisters and other members of her extended family who were subsequently tested and found to carry the same mutation.
Mary-Claire King who was instrumental in finding the first breast cancer gene, BRCA1, in 1990, says “to identify a woman as a carrier only after she develops cancer is a failure of cancer prevention.”
Last September, together with two other leading researchers, she called for population screening for harmful BRCA mutations to be introduced. “Based on our 20 years’ experience working with families with cancer-predisposing mutations in BRCA1 and BRCA2, it is time to offer genetic screening of these genes to every woman, at about age 30, in the course of routine medical care,” they argued (JAMA 2014, 312: 1091–92).
Ephrat Levy-Lahad, a co-author of the JAMA article, and director of the Medical Genetics Institute at Shaare Zedek Hospital in Jerusalem, says that it wasn’t something that just popped into their minds. “It was based on data.”
“To identify a woman as a carrier only after she develops cancer is a failure of cancer prevention”
These data came from research on Ashkenazi Jews. Three BRCA mutations are common in this population, present in 1 in 40 people. Among the general population (excluding Ashkenazi Jews), the likelihood of having any BRCA mutation is about 1 in 400.
It was known that having a family history of cancer as well as a BRCA mutation is associated with a high risk of getting cancer. Levy-Lahad wondered if those with no family history had the same high risk.
“We tested 8,000 Ashkenazi men and 10% of them had a mother with breast cancer, which is what you would expect with breast cancer rates,” explains Levy-Lahad. The group found 175 BRCA carriers across the study population of 8,000, and “saw that cancer rates for carriers was just as high as it is in other families that are found in cancer genetics clinics.” This means that breast and ovarian cancer risks are high in women who carry mutations in BRCA1 or BRCA2, even if these women do not have a family history of cancer. It led Levy-Lahad to strongly feel that “every woman identified as the first in her family, only after she became infected, is a missed opportunity to prevent.”
“Breast and ovarian cancer risks are high in women who carry BRCA mutations even if they have no family history”
Not everyone agrees with King and Levy-Lahad that BRCA testing should be rolled out to every woman. Karuna Jaggar, executive director of Breast Cancer Action in the US, which played an active role in challenging the Myriad Genetics patent on the BRCA gene, has a number of reservations. “Here in the US, we generally live in a ‘more is better, information is knowledge’ culture that is pro-screening and fails to discuss its limits and harms,” she says.
While she respects King and agrees that more women need access to breast cancer testing, she worries about rolling out population screening without sufficient capacity to provide genetic counselling. “I see people who feel they were not informed about the harms and limits of the test before they engaged in it. I see people who talk about the way that family relationships are disrupted and they did not anticipate that. I talk to people who will never know if they lost insurance or their insurance premium went up because they had done BRCA testing, but they’re concerned about it.”
She feels it’s wrong to test people for mutations without full consultations about what the test does and doesn’t mean. “You cannot have informed consent without genetic counselling.”
A duty to counsel
The current requirement for genetic counselling, when a test is done in a clinical setting, means that waiting lists for BRCA tests are getting longer, because there are too few qualified professionals. In many countries, people with a family history are having to wait more than a year.
Judy Garber, Harvard Medical School professor and director of the Cancer Risk and Prevention Clinic at the Dana-Farber Cancer Institute, points out that most people in the general population will test negative and they probably don’t need as much counselling. “But we have a lot of data showing that women who do get genetic counselling and make informed decisions cope very well with the information, even when it’s bad.”
Ian Jacobs, vice-chancellor of the University of New South Wales in Australia, and a leading researcher in the area of women’s health and cancer, conducted a recent cost–effectiveness analysis of population screening in the Ashkenazi Jewish population in the north London. He hopes it may be possible to streamline the counselling approach so it’s much less time-intensive. “One could have a fairly light-touch counselling probably for most of the population, and a more intense counselling for people who have abnormal results.” He believes this would need to be properly evaluated in a trial before rolling out any testing. “You don’t [want to] cause more psychological harm than benefit.”
Trish puts a brave face on her diagnosis, but behind closed doors the psychological impact is very real. She feels that her breasts and ovaries are her female identity, and thinks forty is a very young age to be expected to give up all of that. She is scared senseless when she thinks about early menopause or losing her breasts, the one part of her body that she never had a problem with.
She feels her breasts and ovaries are her female identity, and forty is very young to be expected to give up all of that
She keeps having the same conversations with her husband, who she has loved since they met at school 21 years ago.
“You’re not going to find me attractive”… “You won’t want to have sex with me”… “You’re not going to love me.”
The constant ‘what ifs’ and the fear of losing him. Declan keeps saying that she has nothing to worry about, that they’ll deal with it together. But it’s the unknown implications that frighten her, sometimes to tears. She will have a lower risk of cancer, but how will it affect everything else?
Balancing costs and benefits
The research community are also wondering what the future holds. Jacobs feels that properly designed large-scale population studies are the way to find out whether BRCA screening should be part of it.
One of the factors that need to be considered is whether population screening is cost-effective. The study by Jacobs and his collaborators on screening in the Ashkenazi Jewish population in north London found that, in this population, it is (JNCI 2015, 107:dju380).
Evaluating the costs (test and counselling) versus savings (avoidance of cancer and cancer treatment) involved in testing for the three mutations that account for the great majority of harmful BRCA mutations in this population, they found “it works, is successful, there’s no psychological harm and is cost effective.” Jacobs adds that “there are few things in medicine that you actually save money by making an intervention, but it would seem that this sort of testing in that population saves money as well as saving lives.”
When it comes to the general population, however, the cost-effectiveness equation looks very different. The benefit is much lower because you would expect to find a harmful mutation in around 1 of 400 screened in contrast to 1 in 40 among Ashkenazi Jews. The costs will also be higher, because a wide variety of harmful BRCA mutations are found in the general population.
As Jacobs says, general screening would “involve mutation testing for the entire gene, so there is significant expense, though the cost of that is coming down considerably. One would also have to consider the psychological impact of [screening in] the general population where people are not expecting to have a high risk.”
Levy-Lahad says there is a lot of research being done on screening of Ashkenazi Jews in Israel, and adds that population screening there is only a few years away. She is not concerned about the lower frequency of BRCA mutations in the general population. “It’s going to be rare but it doesn’t mean it cannot or shouldn’t be done. If we’re talking about ultimately sequencing all of our genes, well let’s start with a couple and see how that goes. It would be a very interesting test case.”
“If we’re talking about ultimately sequencing all our genes, well let’s start with a couple and see how that goes”
An expensive test case, according to Jaggar, who says it will cost $150 billion to test all the women in the United States aged 30 or over. “I took a very conservative price of $1,000 per commercial test. It’s easily more than that!” She says that there are many women in the US who currently have cancer who aren’t getting the resources they need. “This is in no way to say that women with mutations are less important, it’s to say we need to decide how are we going to prioritise our healthcare delivery and our research agenda.”
Who benefits?
Another worry for diverse populations is that most genetic research is done on white people of European ancestry. This means that there is currently a lot less known about the genetics of other populations. Aside from Ashkenazi Jews, ethnic and geographic populations known to harbour specific harmful BRCA1 and BRCA2 mutations include Norwegians, Dutch, and Icelandics.
This is one of Garber’s concerns. “In the US, in the minority populations, not so many people have been tested, so variants would be a problem. That means we would be reassuring some people that they were fine when they were not.”
Variants of unknown significance (VUS) are a common problem in genetics due to the huge variation in the human genome. Like mutations, they are changes in the DNA that can be found during genetic tests. The meaning of a lot of that variation is not known. In the case of BRCA genes, that means with a VUS result it isn’t clear whether you have an increased risk of breast or ovarian cancer. “It’s not a yes or no,” says Breast Cancer Action’s Jaggar. “What are they supposed to do with that?”
These variants are one of Jaggar’s main arguments against widespread BRCA screening. “The existence of variants of unknown significance and their relative problems, [demonstrate] how complex genetic testing is. They highlight the necessity for genetic counselling and true informed consent.”
Levy-Lahad points out that “you never understand everything,” so only mutations that are known to be damaging should be reported back. She suggests there are ways around the unknowns, such as people contacting the testing centre every few years to check for new information.
The Israeli-based doctor says that it doesn’t make sense to stop testing because a small minority will find out something that is not yet fully understood. Jaggar thinks this proposal not to tell women is “deeply problematic”. She is concerned that this would “further the over-simplification and binary thinking” surrounding genetics. “We need more education for the public about this topic as it’s much bigger than BRCA.”
Garber also believes education is important and says it is currently unknown how women with little education would react to population screening of BRCA or any other genetic test. If they are given information about specific cancer genes, but not others, “they may misunderstand and may be falsely reassured,” says the Harvard professor. They may think “‘great… my test is negative. I can’t get breast or ovarian cancer’ which of course is not true”.
“If they are given information about specific cancer genes, but not others, they may be falsely reassured”
‘It’s inevitable’
Shirley Hodgson, professor of cancer genetics at St George’s, University of London, who sits on the Public and Professional Policy Committee of the European Society of Human Genetics, shares many of Garber’s concerns.
She argues that, before screening everyone, a proper framework needs to be in place to deal with the consequences of the test, “so that if somebody comes up positive, they have a standard course of action.” She is worried about the approach taken by 23andMe, a company that offers health and ancestry genetic testing, direct to consumers, for under €200.
The results include the three most common BRCA mutations, if you take the test in Europe. “They have a blurb that if you have a mutation, you are high risk and you should go and see your doctor,” says Hodgson. “I worry that something needs to be in place before you do the test, so people can realise what it is and give them enough information so that they can decline or accept what they’re in for.”
In the United States, the FDA have currently stopped the company issuing these results. Hodgson feels, however, that genetic population screening is inevitable. “I think that if we go slowly then hopefully people will understand sufficiently and the systems will be in place to deal with it.”
“Something needs to be in place before you do the test, so people can realise what it is and can decline or accept”
This inevitability of genetic screening is the one thing that most experts agree on. Jacobs feels King’s comments last year were a “push in the right direction” but further research is needed. Garber says that, in time “we should be able to do this for everyone, not just for their breast cancer genes but for all their genes with one test but we’re just not quite there yet.” Levy-Lahad, who co-authored the controversial article that spurred on this debate, also says that “it will probably take a couple more years,” as studies need to be conducted. “What you always hope for is that you can inspire discussion with scientific data that will ultimately lead to better care for people.”
Back in Cobh, Trish now has a second boy and at 35, has another few years before she opts for the preventative surgery that has been recommended by her doctors.
She finds that cancer patients and survivors are the most understanding of her situation. They put her on the same level and know what she might face down the line. “It’s a burden. Something you carry with you all the time.”
All women should have the right to be tested at diagnosis
 Florence Wilks, who lives in London, was diagnosed with ovarian cancer five years ago. Following rounds of chemotherapy, surgeries and two subsequent relapses, she is now on maintenance therapy. Though her mother died of cancer of the vulva, Florence had no family history of ovarian or breast cancer. She wasn’t offered BRCA testing when she was first diagnosed and only found out about it at a conference last year. After requesting a test she discovered that she had the BRCA2 mutation.
Florence Wilks, who lives in London, was diagnosed with ovarian cancer five years ago. Following rounds of chemotherapy, surgeries and two subsequent relapses, she is now on maintenance therapy. Though her mother died of cancer of the vulva, Florence had no family history of ovarian or breast cancer. She wasn’t offered BRCA testing when she was first diagnosed and only found out about it at a conference last year. After requesting a test she discovered that she had the BRCA2 mutation.
“It has implications for my future treatment but also for my family and children,” she says. Florence believes that all women should have the right to be tested on diagnosis: “The first step is to offer it to women who have been diagnosed with ovarian or breast [cancer], and once that is done it should be offered more generally to the wider population of women,” she says.
Routine testing for harmful BRCA mutations is a high priority for Ovarian Cancer Action in the UK. Acting chief executive Katherine Taylor says it is important but currently only happens in a few countries, such as Scotland: “It determines the patient’s treatment path,” and can help family members “make informed decisions about their healthcare.”
“My prognosis is a lot better now,” says Florence, who has been told that upcoming treatments work particularly well with women who have her BRCA2 mutation. “I now believe my future is much brighter. Each day is a gift and nothing is impossible. At one point I could not allow myself to think about my children’s weddings or grandchildren, but life is different now!”
Florence’s children haven’t decided if they want to be tested yet, but she feels that if they also have the mutation, they will have a better outcome than her due to enhanced screening and possibly preventative surgery.




Leave a Reply