Selected reports edited by Janet Fricker
New treatment option for premenopausal women with hormone-sensitive breast cancer
=>New England Journal of Medicine
In premenopausal women with hormone-receptor-positive early breast cancer the aromatase inhibitor exemestane plus ovarian suppression is more effective at preventing recurrence than tamoxifen plus ovarian suppression, a combined analysis of the TEXT and SOFT trials has found. The studies, which were led by the International Breast Cancer Study Group (IBCSG), in partnership with the Breast International Group (BIG) and the North American Breast Cancer Group (NABCG), were presented at the 2014 ASCO annual meeting.
Treatment with an aromatase inhibitor, such as exemestane, has previously been demonstrated to benefit postmenopausal breast cancer patients more than treatment with tamoxifen.
The phase III TEXT (Tamoxifen and Exemestane Trial) and SOFT (Suppression of Ovarian Function Trial) were both conducted to determine whether such benefit could be extended to premenopausal women by combining exemestane with ovarian function suppression. Between November 2003 and April 2011 the TEXT trial enrolled 2,672 premenopausal women and the SOFT trial enrolled 3,066 premenopausal women, from a combined total of more than 500 medical institutions in 27 countries. The women were randomly assigned to five years of adjuvant treatment with exemestane plus ovarian suppression or tamoxifen plus ovarian suppression. SOFT also included a third arm assigned to tamoxifen alone, which will be analysed in late 2014. Suppression of ovarian oestrogen production was achieved with use of triptorelin – a gonadotropin-releasing-hormone agonist – oophorectomy, or ovarian irradiation. The women could also receive chemotherapy as part of their adjuvant treatment.
Results show that after a median follow-up of 68 months, disease-free survival at five years was 91.1% in the exemestane–ovarian suppression group versus 87.3% in the tamoxifen–ovarian suppression group (HR for disease recurrence, second invasive cancer, or death =0.72, 95%CI 0.60–0.85; P<0.001).
Furthermore, the rate of freedom from breast cancer at five years was 92.8% in the exemestane–ovarian suppression group, versus 88.8% in the tamoxifen–ovarian suppression group (HR for recurrence =0.66; 95%CI 0.55–0.80, P<0.001). Overall survival did not differ significantly between the two groups (HR=1.14, 95%CI 0.86–1.51; P=0.37).
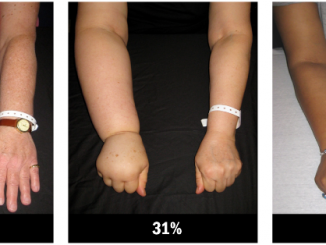
Grade 3 or 4 adverse events were reported for 30.6% of patients in the exemestane–ovarian suppression group versus 29.4% in the tamoxifen–ovarian suppression group, with hot flushes, musculoskeletal symptoms and hypertension being the most frequently reported symptoms.
“We conclude that for premenopausal women with hormone-receptor-positive breast cancer, adjuvant treatment with ovarian suppression plus the aromatase inhibitor exemestane, as compared with ovarian suppression plus tamoxifen, provides a new treatment option that reduces the risk of recurrence. Premenopausal women who receive ovarian suppression may now benefit from an aromatase inhibitor, a class of drugs that until now has been recommended only for postmenopausal women,” write the authors.
- O Pagani, M Regan, B Walley et al. Adjuvant exemestane with ovarian suppression in premenopausal breast cancer. NEJM, published online 1 June 2014 doi:10.1056/NEJMoa1404037
Exercise could enhance drug delivery
=> JNCI
Exercise enhances tumour perfusion and diminishes tumour hypoxia, a rat model of prostate cancer has found. The US investigators believe their study suggests that encouraging patients to exercise could enhance the delivery of tumour-targeting drugs.
Despite recommendation of exercise for cancer patients, the effects of exercise on tumour blood flow and oxygenation have been unknown. Previous studies have hypothesised that tumour blood flow may be elevated or reduced during exercise, which could exert an impact on tumour microenvironments.
In the current study, Bradley Behnke and colleagues, from the University of Florida, Gainesville, randomised 66 male rats aged four to six months to have rat prostate carcinoma cell lines (Dunning R3327-MatLyLu) injected into their ventral prostate (n=42) or saline (n=14). Both injections took place during a surgical procedure.
The saline control arm was intended to explore whether results were due to the cancer state or the surgical procedure.
After surgical recovery (>4 hours), the rats were placed on treadmills, and blood flow in the conscious condition was measured at rest and five minutes after the onset of exercise. The vasoconstrictor responsiveness of resistance arterioles was also investigated in vitro after the animals had been sacrificed, using the isolated microvessel technique.
Results show that exercise resulted in an approximately 200% increase in prostate tumour blood flow, which led to an increase in O2 delivery from a resting value of 3.0 ml O2/min/100 g to 9.3 ml O2/min/100 g during exercise.
During exercise, the average number of patent (i.e. open) vessels per field in the tumour was 14.3±0.6, which represents an increase from the resting number of 12.7±1.3 (Student t-test two-sided P=0.02).
Vascular resistance within the prostate tumour was statistically significantly greater at rest when compared with the prostate tissue of control rats. During the rest–exercise transition, prostate tumour vascular resistance decreased approximately 65%; whereas resistance increased slightly in the prostate of the control group.
In arterioles taken from rats that had been injected with tumour cells, the maximal constriction elicited by norepinephrine was blunted by approximately 95% versus rats with healthy prostate arterioles (the control group injected with saline) (P<0.001).
“Overall, these data demonstrate that exercise augments tumor oxygenation, which, considering hypoxia is associated with a more aggressive phenotype, provides a potential mechanism for the reduced rate of metastasis and tumor growth observed in most studies with chronic exercise and the beneficial effects of exercise after diagnosis of prostate cancer,” conclude the authors, adding that it is unknown whether the same response is observed in other solid tumours or at different intensities of exercise.
In an accompanying commentary, Lee Jones, from Memorial Sloan-Kettering Cancer Center, and Mark Dewhirst, from Duke Cancer Institute, write, “Mechanistically driven preclinical investigations in conjunction with biomarker-driven clinical studies will be required to unravel the complex and dynamic relationship between exercise, the host–tumor interaction, and response to therapy.”
- D McCullough, J Stabley, D Siemann et al. Modulation of blood flow, hypoxia, and vascular function in orthotopic prostate tumors during exercise. JNCI 4 April 2014, 106:dju036
- L Jones, M Dewhirst et al. Therapeutic properties of aerobic training after a cancer diagnosis: more than a one-trick pony? ibid dju042
Robotic-assisted lobectomy results in more complications and higher costs
=> Chest
Robotic-assisted lobectomy is associated with higher rates of intraoperative injury and bleeding than thoracoscopic lobectomy and is significantly more expensive, finds a population-based US analysis.
The perceived benefits associated with robotic-assisted surgery include less postoperative pain, fewer complications and quicker recovery times. Furthermore, in contrast to current minimally invasive methods, it is considered easier to train surgeons using robotic techniques. However, studies in hysterectomy patients have shown that robotic-assisted procedures (for both benign and malignant conditions) are no better than their laparoscopic counterparts.
For the current study, Subroto Paul and colleagues, from New York Presbyterian Hospital–Weill Cornell Medical College, identified 2,498 robotic-assisted procedures and 37,595 thoracoscopic lobectomies, performed between 2008 and 2011. The procedures were identified from the Nationwide Inpatient Sample (NIS), which contains information on 20% of all hospital discharges from non-government institutions in the US. Codes identified which patients underwent which procedures.
Results showed that the number of lobectomies performed by thoracotomy during the period declined from 74.6% of all lobectomies in 2008 to 59.4% of all lobectomies in 2011.
The unadjusted rate of any complication was 50.1% for robotic-assisted lobectomy compared to 45.2% for thoracoscopic lobectomy (P<0.05). Cardiovascular complications occurred in 23.3% of robotic-assisted lobectomy patients versus 20% of thoracoscopic lobectomy patients (P<0.05) and iatrogenic (due to activities of surgeons) bleeding complications occurred in 5% of robotic-assisted patients versus 2% of other patients (P<0.05). After risk adjustment, only the rate of iatrogenic bleeding complications was found to be higher among those who underwent robotic-assisted lobectomy (adjusted OR=2.64, 95%CI 1.58–4.43).
Robotic-assisted lobectomies cost $22,582 compared to $17,874 for thoracoscopic procedures (P<0.05).
The study also showed that a greater proportion of robotic-assisted operations were performed in smaller- to medium-size hospitals, non-teaching hospitals and hospitals with moderate lobectomy volumes.
“Our population based analysis of a national database demonstrates that robotic-assisted lobectomy does not offer any substantial benefit over thoracoscopic lobectomy; and may increase operative risk,” write the authors.
Robotic platforms, they add, provide no tactile feedback, and use of the high- definition three-dimensional operative cameras comes at the cost of a lack of surgical perspective. “Both of these factors can also lead to increased chance of injury by robotic arms by inadvertent excess use of force or their movement out of the field of view. This off-screen damage is neither seen nor felt with the greatest risk from surgeons who are not completely familiar with the technology.”
Recent introductions of robotic energy and stapling devices and dual consoles for two surgeons, they add, could in future decrease both the costs of robotic surgery and the potential for harm.
- S Paul, J Jalbert, A Isaacs et al. Nationwide Inpatient Sample (NIS) analysis of robotic-assisted lobectomy. Chest, published online 8 May 2014, doi:10.1378/chest.13-3032
Changes in health-related quality of life predict outcome in lung cancer
=>British Journal of Cancer
Changes in health-related quality of life (HRQoL) scores from baseline during treatment provide significant prognostic factors for survival in patients with advanced non-small-cell lung cancer, a secondary analysis of an EORTC study has found.
Many studies and meta-analyses have demonstrated that a patient’s baseline HRQoL can predict overall survival across different cancer types, independent of socio-demographic and other clinical prognostic factors. Few studies, however, have investigated whether change in HRQoL from baseline over time offers added predictive value.
In the current study Divine Ediebah, from the EORTC in Brussels, Belgium, investigated whether changes in HRQoL scores from baseline over time were associated with survival, independent of baseline HRQoL scores, in patients with advanced non-small-cell lung cancer. For the study, 391 patients with stage IIIB or stage IV disease enrolled in the EORTC 08975 study (comparing palliative chemotherapy regimens) had HRQoL assessed at baseline and after each chemotherapy cycle, using the Core 30 and lung cancer modules of the EORTC Quality of Life Questionnaire (EORTC QLQ-C30 and QLQ-LC13). The EORTC QLQ-C30 contains: five functioning scales (physical, role, emotional, cognitive and social), nine symptom scales (fatigue, pain, dyspnoea, appetite loss, sleep disturbance, constipation, diarrhoea, nausea and financial difficulties) and the global health status/QoL scale. The LC13 module contains eight scales assessing lung-cancer-associated symptoms: dyspnoea, pain, coughing, sore mouth, dysphagia, peripheral neuropathy, alopecia and haemoptysis.
The prognostic significance of HRQoL scores at baseline and their changes over time were assessed with Cox regression, after adjusting for clinical and socio-demographic variables. Three different change scores were calculated by subtracting the baseline score from the scores at the end of the first, second and third cycle of treatment.
Results showed that after controlling for covariates, every 10-point increase in baseline pain and dysphagia (difficulty in swallowing) was associated with 11% and 12% increased risk of death. Additionally, every 10-point improvement of physical function at baseline was associated with a 7% lower risk of death, and every 10-point increase in pain was associated with an 8% increased risk of death at cycle 1. Every 10-point increase in social function at cycle 2 was associated with a 9% lower risk of death.
“Our work suggests that the regular HRQoL assessments during the course of treatment could be an early signal of patient deterioration, and raises the hypothesis that interventions to improve pain, physical functioning, dysphagia and social function could have potential to improve survival outcomes,” write the authors, adding that appropriate care procedures should be taken when there is an indication that the patient’s HRQoL has deteriorated. The utility of this approach to patient management, they add, should be investigated in prospective studies in patients with non-small-cell lung cancer.
- D Ediebah, C Coens, E Zikos et al. Does change in health-related quality of life score predict survival? Analysis of EORTC 08975 lung cancer trial. Br J Cancer 13 May 2014, 110:2427–33
Melatonin improves sleep in breast cancer survivors
=>Breast Cancer Research and Treatment
Among breast cancer survivors melatonin use was associated with improvements in subjective sleep quality without any significant adverse effects, a US study has reported.
Sleep disturbances are common among breast cancer survivors and can have a significant impact on quality of life. Melatonin has been widely evaluated as treatment for jet lag and insomnia, with more limited evidence suggesting a potential role for melatonin supplements in the treatment of depression. It has also been observed that melatonin levels decrease with age, particularly around menopause and may affect hot flushes.
In the current study, Wendy Chen and colleagues, from Brigham and Women’s Hospital, set out to examine the effects of melatonin supplementation on sleep, mood and hot flushes in postmenopausal breast cancer survivors. Between March 2007 and March 2009, 95 postmenopausal women with a prior history of stage 0–III breast cancer, who had completed active cancer treatment (including hormonal therapy), were randomly assigned 1:1 to either 3 mg oral melatonin (n=48) or placebo (n=47) daily for four months. Women were instructed to take tablets nightly at 9 pm due to melatonin’s possible sedating effects. Sleep, mood, and hot flushes were assessed at baseline and four months using two self-administered questionnaires – the Pittsburgh Sleep Quality Index (PSQI) and the Center for Epidemiologic Studies–Depression (CES-D) questionnaire – as well as the North Central Cancer Treatment Group (NCCTG) hot flush diary, which records both the frequency and intensity of hot flushes over the past seven days.
Results showed that, at baseline, 52% of participants reported poor sleep in the month prior to enrolment. The mean change in PSQI score was –0.1 in the placebo group compared to –1.9 in the melatonin group (P<0.001) – with a higher PSQI score reflecting worse sleep quality. No statistically significant differences in change scores were noted, however, between the two treatment arms for any of the components of the assessed hot flush scores (P=0.19), or the average change in depression scores (P=0.66).
“In this double-blind randomized controlled trial, we have demonstrated the efficacy of melatonin in improving sleep among breast cancer survivors,” conclude the authors, adding that it is possible that higher doses than 3 mg melatonin might prove even more effective.
That the investigators did not see any effects on depression or hot flushes might be explained by the fact that the study was not powered to detect these differences, and also that the subjects were not clinically depressed and only 44 subjects reported hot flushes at baseline.
Future studies, say the authors, should evaluate the efficacy of melatonin in helping sleep in patients undergoing active cancer treatment, and whether sleep improvements translate into improvements in fatigue, since this is the primary complaint of many breast cancer survivors.
- W Chen, A Giobbie-Hurder, K Gantman et al. A randomized, placebo-controlled trial of melatonin on breast cancer survivors: impact on sleep, mood, and hot flashes. Breast Cancer Res Treat June 2014, 145:381–388
Adjuvant! Online inaccurate for older breast cancer patients
=> Lancet Oncology
Adjuvant! Online, a programme predicting 10-year outcomes for patients with breast cancer, does not accurately predict overall survival and recurrence in older people with early breast cancer, a study funded by the Dutch Cancer Foundation has concluded.
Optimum combinations of adjuvant endocrine therapy and chemotherapy in breast cancer now result in relative risk reductions of between 20% and 57% in 15-year mortality. In patients with a high absolute risk of recurrence, the potential benefit of adjuvant treatment is large. Such benefits, however, might be attenuated in the presence of increased comorbidities or old age, because of shorter life expectancy and competing causes of death. Adjuvant! Online is an online, open-access prediction program that predicts 10-year breast cancer recurrence, breast cancer mortality, mortality due to other causes, and expected benefits of specific adjuvant treatment options for individual patients. The model was developed using a large database derived from the Surveillance, Epidemiology, End-Results (SEER) registry, involving a population of 34,352 patients aged 35 to 69 years.
In the current study Gerrit-Jan Liefers, from Leiden University Medical Centre, and colleagues set out to investigate the discriminatory accuracy and calibration of Adjuvant! Online in a cohort of 2012 women aged 65 years or older diagnosed in the south west of the Netherlands between January 1997 and December 2004 with in-situ and invasive breast cancer. The women had a median age of 74.0 years.
For the study, investigators undertook two separate models, one in which comorbidity of all patients was defined as average for age (model 1), and another in which comorbidity was individualised and identified by an expert panel (model 2). The authors then entered this, together with patient and tumour characteristics, into the Adjuvant! Online program version 8.0 to calculate predicted 10-year overall survival and 10-year cumulative recurrence for every patient.
Results showed that 904 patients (45%) died during the follow-up and 326 (16%) had recurrence. Using model 1, Adjuvant! Online overestimated 10-year overall survival by 9.8% (95%CI 5.9%–13.7%, P<0.0001) and 10-year cumulative recurrence survival by 8.7% (95%CI 6.7%–10.7%, P<0.0001).
By contrast, using model 2, Adjuvant! Online underestimated 10-year overall survival by –17.1% (95%CI –21.0% to –13.2%, P<0.0001). However, when using model 2, Adjuvant! Online predicted cumulative recurrence accurately (–0.7%) in all patients (95%CI –2.7% to +1.3%, P=0.48).
“This study shows that Adjuvant! Online does not accurately predict survival and recurrence in older patients with breast cancer. We suggest that Adjuvant! Online’s predictions for older patients should be interpreted with caution,” write the authors. “Therefore, we propose that an improved prediction model specifically for older patients should be developed to individualise clinical decision making and improve outcomes in this heterogeneous and growing population.”
In an accompanying commentary Etienne Brain, from the Institut Curie, Saint-Cloud, France, writes, “Aside from showing the inadequacy of Adjuvant! Online for the older population with breast cancer, this work also stresses the crucial need for better methods to assess individual risks and potential benefit brought by treatments in older people.”
- N de Glas, W van de Water, E Engelhardt et al. Validity of Adjuvant! Online program in older patients with breast cancer: a population-based study. Lancet Oncol June 2014, 15:722–729
- E Brain. Breast cancer in older women: predicting adjuvant benefit.





Leave a Reply