
The recently concluded Partnership programme marked the first time that EU member states have taken a joint approach to improving cancer plans and the organisation of services. Was it a worthwhile exercise? And where do we go from here?
 Can countries improve the way they organise and deliver cancer care by working together at a European level? It’s hard to know until it’s been tried. As member states consider healthcare to be a purely national policy area, EU involvement has not been welcome and the option has not been on the table.
Can countries improve the way they organise and deliver cancer care by working together at a European level? It’s hard to know until it’s been tried. As member states consider healthcare to be a purely national policy area, EU involvement has not been welcome and the option has not been on the table.
Not, that is, until five years ago when a limited opportunity opened up with the establishment of the European Partnership for Action Against Cancer (EPAAC), “to more effectively coordinate activities and actions that are taken within different policy areas by Member States and other stakeholders, with the aim of reducing the increasing and unequal European burden of cancer.” (Communication from the European Commission COM/2009/0291).
The Partnership was set up by the European Commission in June 2009 to run for five years. The move was in response to sustained pressure from some member states, from the European Parliament and from many European advocacy groups, who wanted the EU to continue the efforts started with Europe Against Cancer, a programme that ran from 1987 to 2000.
However, this new initiative differed from its predecessor in three important ways.
- Its work was to be carried out through a ‘Joint Action’, led by representatives from participating member states, rather than through the Commission.
- Its budget was around 80% smaller, shared equally between the participating member states and the Commission.
- Along with health promotion, quality screening, statistics and indicators, its remit included healthcare policy and organisation – areas that had been out of bounds for previous European work on cancer.
Shared solutions to a common problem
European countries are struggling to cope with common problems of ageing populations, rising rates of cancer, more people living longer with cancer, and escalating costs of treatment, at a time of tight constraints on health spending, so working together to find solutions should make perfect sense.
Yet major differences in the organisation of healthcare across countries raise questions about how feasible or desirable it is to coordinate the search for solutions. National histories, cultures, and priorities are reflected in which healthcare professionals deliver what services in what settings, as well as in who is responsible for commissioning healthcare and how it is funded, governed and evaluated. These differences are jealously guarded under the principle of ‘subsidiarity’, which defines healthcare policy, among other areas, as the sole prerogative of each member state.
Differences in how healthcare is organised raise questions about the feasibility of finding common solutions
The great advantage of working together through a Joint Action was that this is a voluntary activity led and organised by member states that wish to be involved, and it was therefore free from any sense of ‘Europe’ telling countries how to run their health services. The potential downside, however, was the challenge of organising work across the full spectrum of cancer control, entirely through co-operation and compromise. Participants – not just member states, but also all interested partners, from professional groups, institutes, advocacy and industry, working at international, European, national or even regional levels – brought to the table their own agendas and were invited to a ‘horse trading’ session to agree the full programme of action. It took a little more than a year to get the whole thing up and running.
The Joint Action came to an end in March of this year, having run for its allocated three years. Tit Albreht, who served on the steering committee and led work on cancer plans, is positive about the interaction between representatives from member states and the results achieved, given the limited resources and timescale. He admits, however, to a certain early scepticism about whether the Joint Action format could be made to work. His country, Slovenia, had played a major role in getting the project off the ground – it was at the conclusion of their presidency in 2008 that the European Council called on the Commission to present an EU Action Plan that would expressly include consideration of “the appropriate framework for effective cancer control policies and sharing best practices in cancer prevention and care”. However, the idea that the programme would be patched together from the various agendas of interested parties, was not necessarily what they had had in mind.
Of the 10 ‘work packages’ that emerged from the horse trading, Albreht mentions, in particular, the one on healthcare. “The care issue finally worked out very well. But at that particular workshop, there were so many issues put forward that I thought it would be pretty amazing if they really could be managed within a single work package. It almost seemed like a separate project in itself.”
The work package in question had no fewer than 12 ‘deliverables’, including the “identification and assessment of best practices on organisational approaches to cancer care” – which might be seen as a field of study in its own right rather than merely one of 12 topics in one of 10 work packages of a three-year project. Other healthcare topics included the feasibility of harmonising clinical guidelines at an EU level, developing common standards in care for children with cancer, assessing palliative care needs, and implementing clinical guidelines.
The man in charge of delivering on these deliverables, together with 15 collaborative partners and 14 associated partners, was Josep Borràs, a professor of public health at the University of Barcelona, director of the Catalan cancer strategy, and scientific coordinator of the Spanish cancer strategy. Happily, this latter role, which involves reaching agreement between Spain’s highly autonomous regional health systems and the ministry of health, had given him plenty of experience in consensus building, and he welcomed the diversity of both the participants and goals.
Reports of the work done by the healthcare and other work packages can be found on the epaac.eu website and in a book, Boosting Innovation and Cooperation in European Cancer Control, which presents key findings, and is downloadable from the site. They document the successful completion of the overwhelming majority of the planned projects. For Borràs, however, while the outcomes are clearly important and will have an impact, the big achievement of the healthcare work package was that it demonstrated that, despite differences between healthcare systems, it is possible for European countries to work together to improve standards of cancer care. “We showed it is feasible, and probably useful, and raised the interest of all the stakeholders,” he says.
Cancer networks
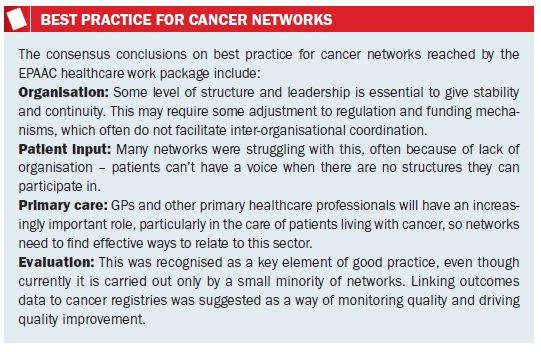
Borràs singles out the discussions about networks as a model for organising cancer care as one of the more significant in terms of showing the European added value.
Conducting the analysis of different models of cancer networks was quite a challenge, he says, because there are very different models. Some are strongly supported by health administrations, while others are more informal, “more of an agreement between organisations or between professionals that works quite fluidly, with nothing very strong from the organisational point of view.”
There was, however, no lack of enthusiasm, he says. “People were really interested in learning from other experiences, because the networks issue has been very local or regional and there are few forums to discuss experiences. Most of them don’t even have a proper evaluation to be published and discussed. There are a couple of assessments of networks in France, Spain or Italy, but there is not a body of knowledge. In that way the interest of the partners involved was very high and they were very happy with the experience.”
“The networks issue has been very local or regional and there are few forums to discuss experiences”
Three networks were analysed in detail: one in the Lombardy region of Italy, another in Belgium and the third in Spain. Participants from four further networks, in England, France, the Netherlands and Denmark, also contributed at a workshop on the topic, which developed a consensus over best practice that was felt to be valid across all health systems.
 With the EPAAC work now over, Borràs is looking forward to carrying on Europe-level work on networks and the organisation of cancer care through a new Joint Action, which will run for a further three years, under the title CANCON. This will be the final funding for joint actions on cancer and Borràs wonders how the opportunity to work together on these issues, which has engaged and enthused so many participants from so many countries, will be able to continue.
With the EPAAC work now over, Borràs is looking forward to carrying on Europe-level work on networks and the organisation of cancer care through a new Joint Action, which will run for a further three years, under the title CANCON. This will be the final funding for joint actions on cancer and Borràs wonders how the opportunity to work together on these issues, which has engaged and enthused so many participants from so many countries, will be able to continue.
Cancer plans
Albreht, who heads up the Centre for Health Care at Slovenia’s Institute for Public Health, reports a similar level of engagement and enthusiasm among people from the different member states working with him on mapping and analysing cancer plans in Europe, with a view to drawing up guidelines of best practice.
He points out that giving government representatives the chance to exchange information and experiences directly is much more productive than exchanges confined to academic discourse or conducted at ministerial level: “you didn’t have this political style of plenary discussion of what are basically professional issues, but it operated more as a sort of ‘back office’”. Representatives from Slovenia, the Netherlands, Belgium, Ireland, Malta and Italy formed a ‘core group’, with other countries, including Finland, Germany, Spain and France, also contributing a great deal. But it was the level of engagement and interest right across the 27 countries of the EU, plus Norway and Iceland, that was the most pleasant surprise. Albreht had anticipated having to spend time and effort getting countries to respond to the survey sent out to establish whether they had a cancer plan, and if so how it was organised and what it covered. In the event, few needed prompting, and the real problem became analysing the large amounts of detailed information that came back. Most countries also took great interest in the results of the survey, “which helped engage national and regional health authorities in the analysis of the plans,” says Albreht “and prompted them to take a more critical look at their own.” Interest in the results of the survey of cancer plans prompted countries to take a more critical look at their own.”
Participating in the work was harder for smaller member states, particularly those without their own cancer strategy; in some cases a single person in a ministry is responsible for all non-communicable diseases. But there are ways around this, says Albreht, such as appointing an expert to be the point of contact on cancer policy issues, “something I feel actually developed during the course of EPAAC in quite a few member states.”
There were also some warning shots fired by countries worried about being pressured into doing things against their will, he adds: “For instance, there were some member states who said: ‘If you are going to present a list of new indicators then you can forget about us ever discussing this’– though this was in fact never our intention.”
Their work was made easier, says Albreht, by the wide diversity of countries involved: small like Malta, large like Germany, highly centralised like France, and highly regionalised like Spain. Some had a strong emphasis on primary healthcare, community care, and nursing involvement, others were more geared to high-end care in a hospital setting. Each had a different funding mechanism and service delivery model. Albreht believes that this diversity made compromise easier. “If you are seeking solutions on the basis of what will work, for instance, in a decentralised system, then the centralised systems may feel that is not something they will want to pursue. I’m not saying that in the EU you have to go for the minimum common denominator at any cost, but you have to take note of important differences in health systems – and not just in health systems but simply in the way that a country operates.”
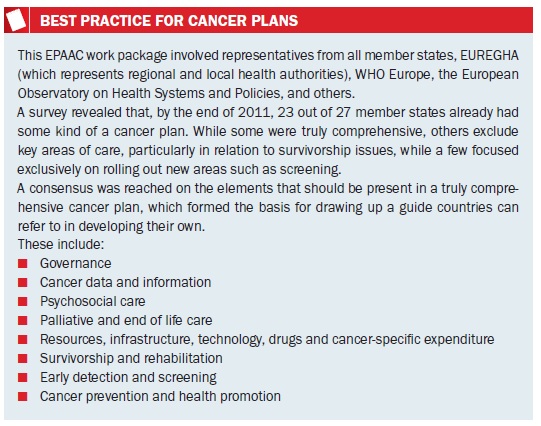
A consensus was reached about the key elements of a well-structured national cancer plan, which is shown below. A guide on how to develop cancer plans, with sections addressing each aspect, is currently being finalised and will be published on the epaac.eu website very shortly. The guide will also define a set of indicators by which countries can monitor progress on each aspect of the plan – which will be the bare minimum needed to do the job, Albreht hastens to add.
 Like Borràs, who led the work on models of cancer care organisation, Albreht believes that the experience and outcomes of the EPAAC Joint Action show that it is feasible and highly worthwhile to work together to find common solutions in healthcare. He is hopeful that a way will be found to continue the work started by the Partnership after CANCON finishes in 2017, though quite how this could be done remains an open question.
Like Borràs, who led the work on models of cancer care organisation, Albreht believes that the experience and outcomes of the EPAAC Joint Action show that it is feasible and highly worthwhile to work together to find common solutions in healthcare. He is hopeful that a way will be found to continue the work started by the Partnership after CANCON finishes in 2017, though quite how this could be done remains an open question.
“We don’t have a European Cancer Institute or any supranational institute that would take this over, and I’m not authorised to say one should be established, though we feel that a European Union body should be responsible for the future steps after 2017.” He sees the agreement to re-establish an EU committee of experts nominated by member states as a welcome start, “but of course an experts’ committee is not a structure that can deal with day to day challenges.”
One possible solution would be to extend the remit of an existing structure, such as the European Centre for Disease Control, in Stockholm, which currently only deals with communicable diseases. “There are people who ask: why do we invest this effort of having a 300-strong staff worrying about a problem that is clearly a known and important challenge for health systems, but is not comparable from the point of view of the burden of disease, cost, and cost in the burden of life. So there are voices that say there should also be a department for non-communicable diseases, and such a department could have an analytical and monitoring role, as opposed, for instance, to just being a data collection centre.”
His sentiments are shared by Josep Borràs. “Now we have shown that this is feasible and probably useful through many experiences within EPAAC, I think something more permanent should be provided by the EU, to promote these kinds of changes in a more permanent way. We are always demonstrating something – showing that it is feasible – and then we stop and have to begin again, but in a slightly different way, because continuing in the same way is not considered appropriate. So one of the issues here is to guarantee some kind of continuity.”
“We are always showing something is feasible, and then we stop and have to begin again”
Neither Borràs nor Albreht is a ‘eurocrat’, and both have taken high-level responsibility for improving cancer care in their own countries. Their verdict is that EPAAC did indeed demonstrate that countries can improve the way they organise and deliver cancer care by working together at a European level. The question now is whether these countries can agree a long-term way to allow this to go forward in a smooth and continuous fashion.






Leave a Reply