An undesired effect of preventive screening for cancer is often overlooked: it’s not only the tendency to diagnose more and more cancers that would be likely to grow slowly – and to increase overdiagnosis – but also the risk of misrepresenting the influence of specific risk factors that might instead have no real role, argue two researchers on the latest issue of the Annals of Internal Medicine. Focusing on mortality, instead of incidence and prevalence, might help.
 «Physicists have long understood that the act of observation can affect the phenomenon being observed» write H. Gilbert Welch and Otis W. Brawley, from the Dartmouth Institute for Health Policy and Clinical Practice, Hanover, New Hampshire and members of the American Cancer Society. «Measuring pressure reduces the air pressure in an automobile tire; measuring voltage reduces the amount of voltage in a circuit. Physicians would do well to understand how the act of observation can affect the apparent incidence of cancer—as well as apparent risk factors for this disease».
«Physicists have long understood that the act of observation can affect the phenomenon being observed» write H. Gilbert Welch and Otis W. Brawley, from the Dartmouth Institute for Health Policy and Clinical Practice, Hanover, New Hampshire and members of the American Cancer Society. «Measuring pressure reduces the air pressure in an automobile tire; measuring voltage reduces the amount of voltage in a circuit. Physicians would do well to understand how the act of observation can affect the apparent incidence of cancer—as well as apparent risk factors for this disease».
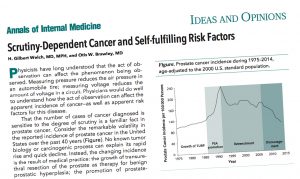
Their analysis cites several examples of what they call «self-fulfilling risk factors», besides and beyond prostate cancer, the «poster child for scrutiny-dependent cancer»: «Any type of cancer with a substantial disease reservoir of indolent, subclinical forms can be subject to the degree of observer scrutiny—the combined effect of the frequency of diagnostic and screening examinations (including the physical examination, imaging studies, and laboratory testing), their ability to detect small irregularities, and the threshold to label these irregularities as cancer».
The effect of scrutiny on the identification of possible risk factors was exemplified by Peter C. Albertsen in an editorial published in December 2016 on the Journal of Clinical Oncology: «Men with a family history of prostate cancer are frequently encouraged to undergo testing. This, in turn, leads to a higher biopsy rate, which, because of the large pool of subclinical disease, leads to higher rates of prostate cancer diagnosis in this group of men, thereby “confirming” the original hypothesis». If men with a family history are exposed to greater scrutiny, diagnoses of prostate cancer will increase in that sub-population, and this will spuriously «confirm» the role of familiarity.
Similar «self-fullfilling prophecies» may have distorted the picture in other contexts: for instance, sex is today listed among the main risk factors for thyroid cancer, «However, this risk factor may be more apparent than real, because thyroid cancer mortality in men and women is approximately identical in the United States. Women may simply be more likely to connect with the health care system; are thus more likely to have thyroid nodules detected and evaluated; and — given the substantial disease reservoir — are more likely to have cases of small papillary thyroid cancer diagnosed» explain Welch and Brawley.
Melanoma offers an even more complex scenario, in which sun exposure appears to be associated both to an increase in diagnoses and a halving of the risk of death from the disease (compared to melanoma patients with low sun exposure): «What might explain this paradox?» ask the reasearchers? «Sun exposure could be a self-fulfilling risk factor. Persons with sun-damaged skin (for example, those with multiple actinic keratoses) may be more likely to see dermatologists, undergo biopsy, and be diagnosed with a biologically favorable melanoma. These factors would explain the lower case-fatality rates associated with sun exposure».
Also for breast cancer, the degree of scrutiny affects not only the incidence – better, the apparent incidence – of disease but also the underlying tumor biology, because more scrutiny means that biologically indolent cases of breast cancer (low grade and luminal) are found. And might appear to be associated with «self-fulfilling risk factors» such as socioeconomic status, that in reality affect the individual propensity to undergo testing and have no influence on cancer itself.
«To avoid such misleading feedback loops, risk factor epidemiology must shift from diagnosis to “harder” outcomes — those more directly related to the disease process» conclude Welch and Brawley. «Although late-stage and metastatic disease are potential candidates, death from cancer is the most meaningful and least ambiguous outcome. As cancer diagnosis becomes increasingly sensitive to observer scrutiny, we hope that those investigating the risk for this disease focus on risk factors for death from cancer, not cancer diagnosis».






Leave a Reply