Progress in understanding resistance and learning how to combine and sequence therapies most effectively is being stifled because specimens donated by patients, and related data, are being hoarded and not shared. Peter McIntyre reports.
There are growing calls across Europe to make more effective use of tissue, blood and other specimens that patients have donated for research to speed up progress in treating cancer. These specimens, together with the linked clinical data about the patient they came from, offer an invaluable resource for researchers trying to identify biological traits that could help guide decisions on the best treatment options for each patient. But failures to share data, and the hoarding of precious biomaterials, are leaving clinicians and patient advocates increasingly frustrated at the lack of coordination in research. Patients who give permission for their tissue and blood products to be used are often unaware that it has effectively become the ‘property’ of a single research team or pharmaceutical company.
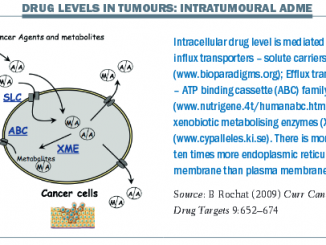
Denis Lacombe, Director General of the European Organisation for Research and Treatment of Cancer (EORTC), says that, despite rapid increases in understanding the genetic causes of cancer, lack of collaboration is hindering progress in treating the disease. It is only possible to fully understand the biology of cancer, including the mechanisms of relapse, recurrence, and resistance, if researchers have access to biological material and the capacity to link it to clinical data about the patient and the course of the disease, he argues. Without that knowledge, clinicians are left guessing at how best to use new treatments. “In the real world, we need combinations and sequences of drugs, but the way we function is industry brings drugs to the market one by one. Melanoma doctors don’t know the optimal duration of a checkpoint inhibitor, how long you have to treat a patient and how to sequence a checkpoint inhibitor with a BRAF, or MEK or CTLA inhibitor.” The industry is not going to address these questions, says Lacombe, so three years ago he spearheaded the launch of a bold EORTC collaborative programme.
SPECTA (Screening Patients for Efficient Clinical Trials Access) is a network involving clinicians and researchers from academia and industry, which seeks to channel patients quickly into relevant clinical trials, which it does by screening material from patients treated at participating institutions using high-quality next generation sequencing, gene expression and genomics.
Trial sponsors looking to enrol patients with specific mutations can find them through the SPECTA database, avoiding the need to screen thousands themselves to identify the subgroup they require. This can benefit sponsors and patients. But the wider cancer research effort also benefits, because the biomaterials from patients recruited for those trials remain in the SPECTA database, and their data are regularly updated, which builds up vital information about progression, recurrence and survival along the entire patient journey.

If patients progress on one trial and move on to another, their longitudinal data can reveal important information about resistance, the impact of sequential treatments, and how that relates to tumour biology, which would not be available if data for each trial were locked away under the control of the separate sponsors, as typically happens today.
Lacombe believes that the SPECTA system of holding materials and data within its collaborative research network could also facilitate clinical trials combining two drugs that are in development in two different companies, which has so far proved impossible. “Potentially, by more sharing we can change this paradigm,” he says. “Patients would maximise their chances to benefit from treatment, because we would be following them from recurrence to recurrence.”
Lacombe has criticised researchers who keep the equivalent of “butterfly collections” of tissue materials in freezers and cupboards, as wasting precious resources. “Butterfly collections decorate your room, but that is it,” he says. “And they fade away with time. In the EORTC, we have banned this notion of ownership which I think is very detrimental. We speak about: ‘Who is responsible for the chain of custodianship?’ Personally I feel more and more that it is unethical for commercial silos to keep biological materials. The reason is that, if a clinical trial is negative, the company will close the programme overnight and all the materials they have been collecting are difficult to access, if not impossible.”
Martine Piccart, Medical Director of the Jules Bordet Institute, Brussels, agrees. “If we look at what we have done over the past two decades, it has been incredibly disappointing. It is very difficult to find the biomarkers for response or lack of response to the new drugs, and the reason is that we never share results and put them in the public domain. So-called translational research is restricted to a single study of a few hundred patients, while it is obvious that the way to make progress in this very complex area is by at least sharing data. Companies do very good work as they have very good scientists. But they never share data with other companies.
“It is disappointing that even academic investigators are sometimes very negative towards sharing, and that has something to do with the need to publish. That must now change because it is a disservice to patients. I think it is not completely honest. It is a real nightmare and patients are totally unaware of this. They donate their material to science because they trust this will help future patients, not in my view a particular company or investigator.”
Piccart, who raised this issue at the European Cancer Congress last year, says that industry and academics need exclusive access to tumour material for a limited period to develop new tests and products, after which there should be open access to the material, with data uploaded to a public platform. She is calling for a cultural shift towards the clinical trials equivalent of The Cancer Genome Atlas (TCGA), which has collected samples from more than 11,000 patients across 33 tumour types. “The CGA project is a fantastic resource for scientists, but it is not connected to trials. Can you imagine if we could do something like that in trials, where data are connected to the clinical outcome of the treatment? That would be absolutely phenomenal. That is the only way we are going to move towards personalised medicine.” The costs of such collaboration could be shared. “We are all partners: the patients, the physicians the companies and the governments.”
Good biobanks share
Many biobanks are organising to share materials better. The Jules Bordet Institute has one of the oldest biobanks in Europe, with 15,000 samples collected over the past 25 years. The biobank steering committee is open to sharing for good proposals, especially for research into rare cancers. Biobank manager Ligia Craciun says that academic research is the first priority but there are also opportunities for collaborating with pharmaceutical companies. Craciun sits on the steering committee of the Belgian Virtual Tumourbank, which catalogues samples from 11 partners across the country, and the Jules Bordet also supports the European Research Infrastructure Consortium (BBMRI-ERIC), which promotes data and sample sharing across Europe.
Another good example is the Biobank for Translational Medicine at the European Institute of Oncology in Milan, which over the past four years has collected materials from 2,500 breast cancer patients and 500 patients with lung cancer, matching tumour tissue with normal tissue, blood serum and plasma. It is the European biobank for collaborative studies conducted by the International Breast Cancer Study Group (IBCSG) and for the ALTTO HER2 trial, coordinated by the Breast International Group, which compared two HER2 blockers used separately, in combination or in sequence in an adjuvant setting. As co-chair of the IBCSG translation research committee, Pruneri says that researchers involved in the studies do have the first call on tissues, but it is possible for other researchers to access them if they put a convincing enough case to the steering committee.
Calls for proposals to use biomaterial collected in the ALTTO trial is currently restricted to participating researchers, but Debora Fumagalli, scientific adviser to the Breast International Group, says that they eventually will open this up. “Researchers have invested tremendous energy and time into the trial and it is fair to give them some ‘protected’ time to propose research ideas that they have. However, our final goal is to open the access to the wider community in order to make the most benefit out of this precious data.”
Pruneri suggests a number of ways to improve the use of material for research. He believes that if hospital pathology departments can become biobanks – with all the quality control, consenting, anonymisation and safe data storage that entails – then material from about 30,000 breast cancer patients could be available across Europe for further research. Centres could use the fees they receive to cover the costs of data managers and specialist nurses. He also agrees with Lacombe about the need for a shift from traditional clinical trials towards studying multiple samples from single patients at different stages of recurring or continuing disease. “This is a new avenue of targeted research that can be accomplished only in a biobank that is actively banking tissue.”
Patient inspired biobanks
Some biobanks have been directly inspired by patients to improve research and treatment. When Ulla Ohlms was diagnosed with breast cancer in 2000, molecular tumour biology and biobanks were in their infancy. She became a founder member of Foundation PATH – Patients’ Tumor Bank of Hope, dedicated to improving research and treatment. The PATH biobank collates breast cancer materials from a network of seven centres in Germany. It has biomaterial from more than 8,300 patients, almost 6,900 fresh frozen tumour samples with matching normal tissue and 15,000 blood serum samples. It comes with clinical data and often with several years of follow up data.
The biobank has a majority of patients on its board and supports breast cancer research in academic centres and in industry. Tobias Anzeneder, manager director of the biobank, says: “We have seven of the best breast cancer centres in Germany that are very big on enthusiasm and engagement. Everybody is happy to make a contribution to research and form part of a successful resource for breast cancer. Gynaecologists and pathologists from the PATH breast cancer centres do all this work of consenting, labelling, data acquisition and sharing completely voluntarily. That is a very big plus.”
 Patient advocate Jayne Bressington was instrumental in starting a UK national GIST tissue bank after her daughter was diagnosed with a rare form of the disease, PAWS–GIST. She was dismayed to find little research into her daughter’s condition and no organised collection of material. When she took her daughter to the USA for specialist treatment, the UK hospital where she had been treated was willing to send tissue samples, but reluctant to send a second batch when the US hospital asked for it. Jayne Bressington said: “Patients are often are invited to sign a consent form about using their tissues for research. Most often a sample of tissue is stored in the hospital pathology lab, and that is where it stays. A researcher can only track materials down if they can connect with patients who are sufficiently proactive to say ‘I have had some tissue collected and it is in the hospital.’ My experience suggests that it takes strong determination on the part of the patient to make that happen.”
Patient advocate Jayne Bressington was instrumental in starting a UK national GIST tissue bank after her daughter was diagnosed with a rare form of the disease, PAWS–GIST. She was dismayed to find little research into her daughter’s condition and no organised collection of material. When she took her daughter to the USA for specialist treatment, the UK hospital where she had been treated was willing to send tissue samples, but reluctant to send a second batch when the US hospital asked for it. Jayne Bressington said: “Patients are often are invited to sign a consent form about using their tissues for research. Most often a sample of tissue is stored in the hospital pathology lab, and that is where it stays. A researcher can only track materials down if they can connect with patients who are sufficiently proactive to say ‘I have had some tissue collected and it is in the hospital.’ My experience suggests that it takes strong determination on the part of the patient to make that happen.”
Working with supportive clinicians in the UK, Jayne Bressington has helped to establish a national GIST tissue bank at the Northern Institute for Cancer Research in Newcastle, but it is proving difficult to build a national network of contributing clinicians. “My vision is that when these operations happen, the surgeon and patient will sign a consent form that automatically says that tissue can be transported to the national GIST tissue bank. That does not happen at the moment.” The plan now is to move the biobank to the Royal Marsden in London, which has the highest concentration of GIST patients in the country and an established biobank.
Promoting a culture of sharing
The UK is investing in biobanking at a national level. UK Biobank – a charity supported by the National Health Service – has collected blood, urine and saliva samples from 500,000 people who have also agreed to have their health followed. In another project, Genomics England, is sequencing the genomes of 100,000 UK citizens, half of whom have cancer, with the aim of supporting efforts to develop therapies and diagnostic tests. The anonymised data is made available to academic and industry researchers.
But a great deal of valuable material is also held in a myriad of biobanks belonging to different institutions or research groups. In 2007, the National Cancer Research Institute initiated a UK Confederation of Cancer Biobanks to raise standards, which included a statement promoting sharing and collaboration. Those working with tissue products, it said, “should use these samples, or make them available to others for use, in the best interests of the public and not solely in the interests of themselves or their organisations.”
Derek Stewart, the patient advocate who first chaired the Confederation said, “If we are funding a biobank from the public purse or charities that have raised money through public efforts, then I personally think it is unacceptable that those tissues are not being shared. If you receive the funding, there should be an onus to show what you are doing for the patients and public.”
In 2011, the National Cancer Research Institute and the Medical Research Council published a UK Funders’ Vision for Human Tissue Resources, under which research groups are expected to consider how to link with existing studies or trials that already have collected high-quality clinical data, rather than collect their own. If they do collect tissue, they should seek generic consent from patients so it can be used for a range of research, and make access possible through a publicly accessible directory. The vision says: “Sample collections must then be made more easily discoverable and accessible for use in high quality, ethical research.”
In May 2016, the first national directory of UK biobanks was published. Philip Quinlan, Director of the Tissue Directory and Co-ordination Centre, says they are encouraging 250–300 tissue banks in the UK to sign up. “There is a need to know more about what is going on. We are still in the discovery phase of making it possible to find the resources.”
The long-term aim is to improve research access to the biobank materials. “Members of the public and patients are incredibly generous and usually make donations with no strings attached. With that there is a duty to make sure they are used – not to do so is almost misuse.
“If people need to reserve them for a particular research study, that is fine, but in the longer term there is a real need to make sure those samples are used for the purpose they were collected.”
The Centre is also working with software companies to improve the technical ability of biobanks to share materials. “If a biobank wants to share, it should be as easy as flicking a switch.”
“My vision is that the consent form automatically says
that tissue can be transported to the national GIST tissue bank”
While there may be logistical and technical challenges in sharing biomaterials, there’s less of an excuse for failing to share the data generated by studies that use those materials, and here again there seems to be a need for a cultural change. Most biobanks ask researchers to provide feedback on the quality of the samples, but few require feedback on the research results or are equipped to handle this information. However, they put varying degrees of pressure on researchers to make their results known. Genomics England, for example, says “access may cost them less if they make their results available to all other researchers.”
Ligia Craciun from the Jules Bordet institute says that researchers who fail to publish their results would find it harder to win access to the materials in future.
In Munich, Anzeneder says: “PATH will always encourage you to publish. I ask how the research is going and when results will be published. As a biobank founded by patients, PATH has a big interest in seeing as much data shared as possible.”
Team science
As the Cancer Genome Atlas closes its data collection phase in 2016, Director Jean Claude Zenklusen counts the development of ‘team science’ as one of the most valuable outcomes, enabling researchers to uncover patterns and investigate questions that were not even imagined at the start of the project.
Martine Piccart says this kind of team work is too rare in medicine, where reputations are based on publications, and collaboration is not fully recognised – being ‘et al.’ in a publication does nothing for your career.
The situation is not much better in north America, where Lillian Siu, director of the phase I programme at Princess Margaret Hospital, Toronto, Canada, was recently asked to help the US National Cancer Institute (NCI) and a pharma company develop an antibody towards a biomarker for a rare lymphoma. The task was urgent and biobanks are reluctant to allow rare tumour samples to be used for pre-clinical analysis. After making 20 calls to pathology labs, Siu had to buy samples on the Internet for preliminary testing. “I think it is a pity because there are tons of data and samples out there if we had made a collective effort to biobank them. If there was a vision to do that many years ago, I would not have to go through so much to find the rare samples.”
In a presentation to the Cancer Therapy Evaluation Program in Maryland, Liu highlighted the importance of effective biobanking in improving the speed and effectiveness of research in the Experimental Therapeutics Clinical Trials Network (ETCTN), established by the NCI and partners to evaluate new therapies. She argued for the network to establish a virtual biobank with an inventory of tumour samples at different ETCTN sites, complete with histology and molecular genotype, and with clear guidance on how to obtain samples, including conditions under which ethics approval could be waived. She flagged the importance of including rare tumours, and also emphasised considerations of sustain-ability, which can be a big issue particularly with biobanks that serve broad clinical trials networks, rather than individual clinical trials. “You can do all this but if you don’t bank you have got nothing. We really have to think about how to do this in a way that is sustainable. To bank tumours you have to have core funding institutional support. It is not like it comes free.”
Lacombe, meanwhile, has been pursuing the EORTC vision for collaboration around its central platform for gathering biological and clinical data, by holding one to one conversations with “the big four” stakeholders in Europe: the European Medicines Agency, the European Federation of Pharmaceutical Industry Associations, the European Com-mission and the Innovative Medicines Initiative.
So far there are no signs of a breakthrough. “It is extremely difficult to provoke such a major change because it requires that people completely think out of the box, to share collections and so on. It is work in progress and we keep talking. Not everyone has necessarily understood the need for changing the way we are doing things.”
So far, SPECTA has recruited 1,000 patients with colorectal cancer and 150 lung cancer patients and is now recruiting for melanoma, neuro-oncology and rare tumours. It is steady progress, but Lacombe contrasts the situation in Europe with the NCI-MATCH trial in the US, which will base cancer treatment for 5,000 patients on individual molecular profiling. Supported by the NCI Clinical Trials Network, MATCH took just four months to reach its first recruitment target, and began its main phase of recruitment at the end of May 2016. Lacombe says NCI-MATCH has credibility because it is seen as indepen-dent and is backed by a trusted governmental body. “It has big visibility and it is very successful. They are getting a lot of trials and the programme goes well, and I think that here we are paying the price of a fragmented Europe.”



Leave a Reply