The risk of developing breast cancer varies widely from woman to woman in ways we are increasingly able to define. Marc Beishon asks: Is it time to move to population screening for risk, and tailor mammography schedules – and prevention advice – to each individual?
The past few years have arguably given us the most controversial, long-running dispute in healthcare – whether the benefits of mammography screening outweigh the harms. There is much at stake – not least the cost of running population screening programmes for many millions of women in the western world, and potentially in less well-off countries as well. Public health officials have been grappling with conflicting evidence about the merit of screening, and what to tell women who are invited to take part in one of the centrepieces of cancer control policy.
The prospect of finding some common ground may now be emerging thanks to work being done by a variety of groups to replace the traditional ‘one size fits all’ approach with one that personalises screening according to how each woman scores on a set of risk factors.
This could have profound implications, as women in low-risk groups could drop out of programmes after one or two screens, which could go some way towards satisfying those who argue strongly against routine population screening. More likely, for the next 10 to 20 years, screening will remain a regular event, but with screening intervals adjusted for risk. This would still be a radical change given that it is hard to turn around major public health programmes that have considerable bureaucracy and investment in certain IT systems and core beliefs.
There is a race of sorts to establish the evidence that a risk-stratification approach will work. Ahead is a group in Manchester, England, while others in the Netherlands and Sweden are following. A group in Italy is preparing a study on three regions in the country. These are cohort studies, not randomised controlled trials (RCTs), but in the US the first RCT on risk stratification is taking shape, which could be the precursor to a round of such trials, and which could mark the point at which screening practices change, given that the RCTs that support current programmes are now old and were carried out when treatments were different.
But it is the opportunity that such a risk-stratified approach offers for linking screening with prevention that is causing the greatest excitement among some in this field. As Jack Cuzick, an epidemiologist and prevention specialist at the Wolfson Institute in London, comments: “Screening and prevention go together beautifully, but there is currently no attempt to do this.”
Some women, mainly those with a high family risk, are already offered earlier and more frequent screening, but a big step would be intervening with a prevention strategy for all women attending screening, especially those at moderate to high risk.
“Screening and prevention go together beautifully –
but there is currently no attempt to do this”
“If we can find 20% of the population who will get 40% of cancers, we have the means to reduce their risk by about 50% with preventive therapy,” says Cuzick. “That could reduce breast cancer incidence by 20% if all high-risk women were identified and took up preventive therapy. Combined with lifestyle changes in the rest of the population, this offers a way to reduce overall incidence by as much as 25%.”
Andrea De Censi, director of medical oncology at Ospedali Galliera in Genoa, Italy, has been championing preventive strategies in breast cancer for nearly three decades, and sees moves towards risk-stratified screening as an important opportunity. “We know women at low risk do not want to abandon screening at present. The debate is how to focus on those at high risk to try to prevent cancers,” he says. Once this group has been identified, they may then want to collaborate on risk reduction, although De Censi is not sure all women actually want to know their risk – like smokers who avoid going to the doctor.
Stratifying by risk
There are three main steps researchers are now combining to better stratify risk, says De Censi. The first is to apply a well-studied risk tool, such as the Tyrer–Cuzick model (Jack Cuzick is the co-developer), or one of a number of others (the Gail model is widely used in the US, for example). Tyrer-Cuzick, part of IBIS (the International Breast Cancer Intervention Study), estimates the likelihood of a woman developing the disease within 10 years and during her lifetime, and takes into account factors such as age and weight, age of first menstrual period, whether she has had children, whether she has gone through the menopause, and if she is a current or past user of hormone replacement therapy (HRT).
Some of these may not remain constant: age of course, but also weight gain – which is now known to be a much more important factor than alcohol intake (which is not included in the models) – HRT use, and family history (which is a major predictor and can change as new events may occur in a family).
Already, these models can stratify women into those at high and moderate risk, and they have been validated, says De Censi.
A second step is breast density, which does not just mask lesions in dense tissue, but is associated with cancer risk, and is an ongoing field of study. “Density has been measured fairly subjectively, but now there are ways to apply computerised methods that will probably be more accurate,” he says. Importantly, density is also a surrogate biomarker in trials of prevention drugs like tamoxifen, he adds – a decrease in density is a sign that the drug is working.
The third step is to take a genomic profile from a blood or saliva sample – this is to assess frequency of common variations (single nucleotide polymorphisms, or ‘SNPs’) related to risk, but not the BRCA1/2 mutations that give rise to major risk (these are taken into account in Tyrer–Cuzick, but affect only relatively few women). Again, this is ongoing research.
One of the leading trials of this three-pronged risk-stratification model is an ongoing study called PROCAS (‘Predicting Risk Of Cancer At Screening’), led by Gareth Evans, professor of medical genetics and cancer epidemiology at the University of Manchester, UK. It’s part of a programme now called Prevent Breast Cancer, which aims to fill knowledge gaps on risk estimation, prevention strategies (both medical therapy and lifestyle changes) and the biology of breast cancer risk. The first phase of PROCAS ran from 2009 to 2015. It recruited more than 57,000 women who were invited for screening in a certain area, and the group has published data showing how the distribution of risk changes as first breast density and then SNPs information is added to the Tyrer-Cuzick model.
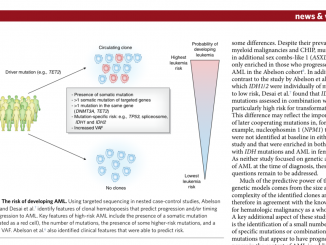
Risk stratification models
The PROCAS (Predicting Risk of Cancer At Screening) trial is investigating a breast cancer risk stratification model that starts with factors such as age, weight, and hormone-related factors (the Tyrer-Cuzick model), and then adds information about breast density and the presence of any of 18 SNPs associated with higher risk of breast cancer. The figure above shows how risk estimated according to the Tyrer-Cuzick model (the blue bars) changes when information about breast density (adjusted for age and body mass index, shown in brown) and SNPs (green) is added, with many women’s risk levels being either upgraded or downgraded.
Source: Genesis Breast Cancer Prevention Centre: Research Overview 2014/15. (2015) Genesis Breast Cancer Prevention Appeal, Manchester
Evans stresses that his team is yet to publish recent results from the latest phase of the project, but says they are close to being able to confirm from data on nearly 10,000 women who have provided DNA samples that about one in six (17%) are at moderate to high risk, of whom 6% are in the high-risk group, and have a 10-year risk of more than 8% of having breast cancer (moderate is 5–8%). That high risk doubles to 16% for the 20 years of the UK’s screening programme, which runs from age 50 to 70. Then there is 30% at below 2% risk – women who have a low incidence of breast cancer – and the remainder are in a 2–5% average risk group.
Evans hopes that risk profiling
will eventually start at entry
to the screening programme
“Importantly in the high and moderate groups, we are not just detecting what we would call overdiagnosis – there is less as a proportion of indolent DCIS [ductal carcinoma in situ] and grade I type cancers, and also more interval cancers [breast cancers diagnosed in the interval between scheduled screening episodes in women screened and given a ‘normal’ screening], which could justify more frequent screening for these women,” says Evans. “And we would potentially pay for this by reducing screening in the lower risk group.”
Stratified risk management
Evans adds that the 30% low risk group could be advised that their risk/benefit ratio is not enough to justify ongoing screening. The UK, he adds, is also in a unique position with three-year screening intervals, which would work well for the 2–5% risk group, while women classified as at moderate to high risk could move to two-year or annual screening, and possibly chemoprevention with tamoxifen or other drugs. The UK’s NHS, he adds, could at least set a benchmark for the rest of the developed world to move to three-year intervals for a large number of women, although again he emphasises that this is a preliminary indication.
“We have found that women are ten times more likely
to be motivated when advised in a risk management approach”
Like Cuzick, Evans hopes that risk profiling will eventually start at entry to the screening programme, which could be earlier in the UK than the current age 50. PROCAS has an ‘extension’ trial looking at starting at 47 and going up to age 73, although in the older age group, while risk continues to rise, there is more chance of overdiagnosis. But importantly, says Evans, women often believe wrongly that their risk disappears once they are no longer offered screening (and generally there is a poor understanding of breast cancer risk among women).
He is also of the view that the evidence supports the effectiveness of the current screening programme, but that informing women of their risk will give them a more informed choice on whether to attend screening or not, while those at higher risk could not only have more regular screens and chemoprevention, but could also take steps to cut their risk through modifying their lifestyles. “We have found that if you tell women they are at moderate or high risk, they are more likely to come for their following screening, and they will also take steps to cut their risk.
“Cynics say that identifying risks does not mean people will act, as we are bad at taking advice on our weight, and sticking to diets and exercising more – but we have found that women are ten times more likely to be motivated when advised in a risk management approach.”
Further, the vast majority (95%) of women in PROCAS wanted to know their risk, although there may be cultural barriers elsewhere, as De Censi suggests may be the case in Italy. Being given a high risk score can also be distressing, and Evans says his team is doing formal assessment of this, but he feels it can be counterbalanced by the benefits of more frequent screening and motivation to reduce risk.
As Evans points out, these sorts of risk-stratified prevention strategies could not only cut the incidence of breast cancers but also save the £20,000 [€22,000] or so it costs to treat a cancer. It’s also important that any intervention is at least cost neutral, he adds, given pressures on health spending and the budget allocated to screening.
Refining the models, building the evidence
Refining risk models with underlying genetic predisposition is also likely to improve, as more data emerges from even larger studies, such as the Breakthrough Generations Study, which is following more than 113,000 women across the UK for 40 years, and which in 2015 reported two new breast cancer susceptibility ‘loci’ (there are many SNPs associated with risk – PROCAS has been using a panel of 18).
“The next step with PROCAS is to do it live – if we can show it’s feasible and doesn’t cause harm, then we would also want to do a large RCT, where you offer one population the full risk strategy approach and compare mortality with a group that has screening as usual,” says Evans. The live version of PROCAS will provide rapid feedback of risk to women – in the first phase this was a lengthy process.
The ASSURE project focuses on tools
such as MRI and ultrasound to personalise screening
and increase sensitivity
Other groups in Europe working on risk stratification include the Karma project at the Karolinska in Sweden, which has a range of studies in train, including on prevention, breast density and cancer detection, and the Prisma team at Radboud University Nijmegen Medical Centre in the Netherlands. The latter institute is also coordinating the EU-funded ASSURE (‘Adapting breast cancer Screening Strategy Using personalised Risk Estimation’) project, which has several academic and commercial partners around Europe, and which has a particular focus on breast density and tools such as MRI and ultrasound to personalise screening and increase sensitivity.
As Nico Karssemeijer at Radboud notes, about 30% of breast cancers are detected between screening rounds, and a retrospective review has shown that almost a third of these could have been picked up in an earlier screening round, had the then-present signs of cancers been spotted at the time.
De Censi says he is helping to put forward a proposal in Italy to start a risk stratification study in three regions, and it will add insulin resistance to the factors taken into account in the PROCAS project.
Meanwhile in the US the first RCT of risk-based screening is underway, called WISDOM – ‘Women Informed to Screen Depending On Measures of risk’), and funded by the Patient-Centered Outcomes Research Institute (PCORI). It addresses the more aggressive approach to screening in the US, in which many women have annual screening starting at age 40, despite mortality rates being no lower than in Western Europe (and despite recent changes in recommendations to start screening later). The trial aims to randomise 100,000 women between the ages of 40 and 74 into a risk-based screening protocol (including a genomic profile of more than 150 SNPs), or annual screening as usual. The primary outcome measures are the proportion of cancers diagnosed at stage IIB or higher, and the rate of biopsies performed.
The principal investigator of WISDOM is Laura Esserman, a breast surgeon and head of the Carol Franc Buck Breast Care Center at the University of California, San Francisco. She is known as a ‘rebel’ in the US for combating overdiagnosis and overtreatment, particularly of DCIS, which has soared in incidence since screening started, but also overuse of treatments such as radiation therapy. As an indication of her status, she has been recognised by Time magazine as one of the 100 most influential people in the world. While she believes that personalised screening could be the way to go, the study protocol rather gives the game away: “The investigators believe this study has the potential to transform breast cancer screening in America.” But there will be a lot of work to do in building the evidence to a level that will dispel the fear that Esserman says many American women feel if they were to forego the current regime.
Evans is somewhat sceptical about WISDOM, as he expects confounding from women who will go for annual screenings anyway, given the easy access in the US. The WISDOM group has though done a pilot that has shown that randomisation is feasible. Evans also makes the point that this study is really only comparing variations in screening, and not the merit of screening per se – but concedes that carrying out a new RCT on screening vs no screening to update the evidence base in a fundamental way is not likely to happen soon.
Policy and practice
Whether the risk/prevention advocates can actually make headway against the breast screening ‘machine’ is a moot point, as Cuzick reiterates. There will need to be substantial changes to IT systems and processes to incorporate risk data, nurses will need training in the approach, and counselling will be needed for women at high risk, he says. He also questions how far women will act to reduce their risk, despite the evidence from PROCAS (with which he is also involved). He would like to see primary care doctors do more to support patients to take action – a new study shows that even a very brief referral to a weight management group is effective (Lancet 2016, http://bit.ly/obesity_intervention).
Cuzick also points out that a risk-stratified approach to screening is not new: it is already applied in cervical cancer, where in the UK the younger age group of 25–49 is invited every three years, in contrast to every five years for the 50–64 age group, because the disease develops more rapidly in younger women.
Mortality from breast cancer has been declining in most developed countries, and the arguments will no doubt continue about the extent to which screening can take the credit for this drop and for lowering the incidence of metastatic disease. Advances in understanding of cancer biology raise challenging questions about the reliance on the size of a tumour, the mainstay in screening, and even lymph node status, in prognosis, as some cancers are molecularly more aggressive, which is why groups such as Prevent Breast Cancer, in Manchester, are trying to do much more than just improve conventional screening.
However, as De Censi comments, wearing his ‘prevention hat’, mortality is only part of the picture, as preventing an invasive cancer that would not have metastasised, subject to standard treatment, also gives substantial gains in quality of life and wellbeing – and cost savings.
As a medical oncologist, he says his prevention interest is not widely shared with colleagues immersed in the world of anti-cancer drug treatments, while the screening side is dominated by epidemiologists. “Prevention is in its infancy,” he laments. But the signs are that the wheels are turning slowly towards seeing risk-stratified screening in the prevention field – although as well as professional collaboration, there may also have to be much better awareness of the concept of risk among the public.
Mammography: the latest evidence
Do the risk reduction benefits of mammography outweigh the harms? In September, Harry de Koning, professor of public health and screening evaluation at Erasmus University in Rotterdam, summed up the evidence and the points of contention at a meeting convened by University College London as part of its Frontiers in Oncology series.
Mortality benefit
In 2015 an expert group convened by the International Agency for Research on Cancer (IARC) concluded that there is sufficient evidence to show screening is effective in reducing mortality from breast cancer in the age groups 50 to 69, and 70 to 74, but evidence of effectiveness in younger age groups is limited (NEJM 2015, 372:2353–58).
The risk reduction among women aged 50–69 was estimated at 23% among those invited to screening and 40% among those who actually attended. The research was done to update IARC’s handbook on mammography screening, first issued in 2002, and takes account of 40 case-control and cohort studies conducted in the interim.
Further, the last update of the influential Cochrane review says that screening is likely to reduce breast cancer mortality.
A 2014 Netherlands’ case control study of screening attenders versus non-attenders showed that screening halves the risk of dying from breast cancer, and Dutch women are currently informed that about 775 fewer women die from the disease each year thanks to screening.
The proportion of cancers picked up at an advanced or metastatic stage in six European countries, including the Netherlands, was 42% in 1990/91 without screening but by 2013 this was much lower in the Netherlands, at 23%.Earlier detection or better treatment?
Critics have argued that mortality reductions have come mainly from new treatments and better organisation of breast services.
A number of recent studies have looked back at the data in various ways. A recent paper in the New England Journal of Medicine (vol 375, pp1438–47), for instance, questions evidence about the drop in the proportion of larger tumours detected with the introduction of mammography, arguing that “the more favourable size distribution was primarily the result of the additional detection of small tumours.”
De Koning replies that the study only looked at data up to the year 2000, and has an arbitrary cut-off point for looking at tumour size.
There is also evidence to show that screen-detected cancers are independently associated with better prognosis (see for example JNCI 2011, 103:1–13), he notes. Another paper examined mortality from ER (oestrogen receptor) positive and negative cancers according to the relative contributions of adjuvant therapy and screening. Adjuvant therapy had a bigger impact than screening in ER positive cancers, but about the same in ER negative ones (JNCI 2014, 106:dju289).Overdiagnosis
Estimating the extent of overdiagnosis is difficult, and studies that fail to adjust for breast cancer risk and/or lead time tend to overestimate the problem.
The 2015 IARC expert review did confirm that there is sufficient evidence that screening does detect cancers that would never have been diagnosed otherwise.
But it is the extent of this overdiagnosis that is crucial, and there has been much debate about how to explain the excess incidence in screened populations. In 1994, de Koning and colleagues put forward a model that predicted that there would be a big (temporary) drop in incidence – well below the unscreened incidence rates – when women leave the screening programme at the upper age limit, because their cancers had already been detected. Critics have said this has not been observed, but de Koning has now produced data from the Netherlands that does indeed show quite a close fit with the predictive model (see the graph in The Breast 2016, 27:182–83).
A modelling technique called ‘age-period-cohort’ is also being used to quantify the impact of screening mammography on incidence of DCIS (ductal carcinoma in situ), and early and late stage cancers, accounting for influences of birth cohort and changes in secular risk factors (ie risk factors associated with a particular period).
One such study found that, while mammography contributes to ‘markedly elevated’ rates of DCIS, it also contributes to substantial reductions in the incidence of metastatic breast cancer (Cancer Epidemiol Biomarkers Prev 2015, 24:905–12).
De Koning himself estimates the overdiagnosis rate at between 1% and 11%, and points to a model on the Netherlands that shows that, of 1,000 women aged 40 or over, who are invited to screening and followed over their lifetime, it is estimated that 124 will have a false-positive screening result, but only three will be unnecessarily diagnosed and treated. He adds though that: “Without diagnosis there is no benefit – for every three breast cancer deaths prevented, one woman is overdiagnosed.”
De Koning is currently coordinating a new EU-funded programme, EU-topia (eu-topia.org), which aims to measure the impact of screening for breast, cervical, and colorectal cancer and provide countries with tools to manage their own programmes in terms of health outcomes and cost-effectiveness, and also aims to identify inequalities across Europe.
Preventive strategies for women at high risk
Women are not all the same – and nor is their risk of breast cancer. Screening women for risk levels can not only reduce unnecessary testing in women at low risk, but also give women at high risk the information they need to take informed decisions about taking steps to lower their risk. These include lifestyle changes and, in those at highest risk, chemoprevention.
Currently, two selective oestrogen receptor modulators (SERMs), tamoxifen and raloxifene, are approved in the US and recommended by NICE in the UK for those at moderate to high risk (in the UK for those with familial breast cancer history). Take-up rates, however, are reported to be quite low – one in six.
Aromatase inhibitors such as exemestane and anastrozole are also being trialled for postmenopausal women (raloxifene is also only for postmenopausal use – only tamoxifen is approved for premenopausal chemoprevention). NICE recently recommended anastrozole rather than tamoxifen for women with a family history of breast cancer.
The data from trials of all these agents are good in terms of reducing breast cancer incidence of ER+ tumours, although there are side effects. Studies show that tamoxifen taken for five years decreases invasive breast cancer risk by 30–40%, and exemestane reduces incidence by 65%. However, mortality benefit has not yet been shown, even after long follow-up in one tamoxifen study. Some commentators are asking whether chemoprevention has now reached the end of the road (JAMA Oncology 2015, 1:1033–4).
Proponents of chemoprevention, including Jack Cuzick, argue that follow-up is not yet long enough to evaluate mortality, and there simply haven’t been enough deaths in the study groups to show a mortality reduction. Nevertheless, he notes a projection of an 18% mortality reduction in ER+ disease (Lancet Oncol 2015, 16:67–75).
Other compounds being studied for potential benefits in women at high risk of breast cancer include genistein (a component of soy), omega 3 fatty acids, vitamin D, bisphosphonates, statins, metformin, and even some vaccines. None of these have yet been shown to be preventive in RCTs (Trends in Breast Cancer Prevention Springer, Switzerland, 2016).




Screening – whether at a molecular level or by mammography, has, to a greater or lesser degree, have the potential for psychological harm, even if designated screen negative, for what woman is not forced to think about the possibility of having cancer if offered such screening? Chemo-prevention adds the physical risk of long term consumption of a molecule that may cause symptoms and potentially serious disease in a fraction of patients after long term use. Lifestyle changes have minimal risk of harm above the baseline level (the knowledge that all women have a finite, though variable chance of developing breast cancer. They have the advantage of having a positive effect on many diseases at once (unlike breast cancer screening) such that the net benefit is considerably greater than screening for individual disease predisposition may be justified if risk is known to be very high, e.g., in familial cancers. While the initiating and continuation of lifestyle changes, largely through standardizing the delivery of education about risk factors from an early age, associated with research and actions relating to social attitudes, {e.g., making it simpler and more enjoyable to take regular exercise, while encouraging gradual changes through progressive legislation relating to the content of salt and sugar in commercial foods), the human body may, eventually, return to the average size and shape that prevailed before the obesity epidemic. The affect of this on cancer will need to be studied, but many surveys of e.g., the British diet and similar topics have existed for many years. I have not reviewed these, but it would be possible, as no doubt is being done, to relate past lifestyles and body shapes to changes in cancer incidence. I wonder why we have not seen more data of this kind.
I absolutely agree with Ian Magrath that we need to pay more attention to using the knowledge we have to prevent breast cancer, which means introducing the actions he mentions early in life, and continuing throughout life.
Risk-based screening seems a cost-effective approach to screening, until you realise that it is entirely dependent upon the assumption that screening is effective. Basing decisions on comparing self-selected groups of women who accept invitations to be screened with those who do not is wrong. Such comparisons are biased, as George Knox pointed out many years ago when we were trying to evaluate cervix screening, and later re-enforced in the review of the US Breast Cancer Detection and Demonstration Project. The recent evidence from Norway re-enforces the evidence accruing that breast screening is not reducing the incidence of advanced breast cancer, necessary if a mortality reduction is to be seen.
Instead, we need to concentrate on promoting early diagnosis of breast cancer by public and professional education, and the prompt application of effective therapy, while all the time pushing the primary prevention agenda.