
Epidemiologists have long been warning of the rapid rise in cancer rates hitting low- and middle-income countries. But it takes a journalist to get across how those statistics are playing out in peoples lives. Jason Gale, who covers Asian Healthcare for Bloomberg Markets, received a Best Cancer Reporter Award for his piece on the cost of cancer in India, reprinted below.
Oncologist Bhawna Sirohi hurries to the front of a packed seminar room at Mumbai’s Tata Memorial Hospital on a Thursday afternoon in April. Cramming this meeting into her 12-hour workday, she greets more than three dozen breast cancer patients united by the bright scarves covering their bald heads.
Sirohi says that when she began her job at Tata Memorial, Asia’s largest cancer treatment center, last year, she realized she could never give the 50 to 60 patients she sees each day enough individual attention. Doctors at India’s premier oncology hospital typically have less than 10 minutes apiece for 1,000 newcomers a week. They often examine three people at a time in a single room.
During Sirohi’s 11 years at London’s Royal Marsden hospital, she saw no more than 35 people a day and spent about 45 minutes with new patients. At Tata, she decided her best option was to co-host once-a-month group sessions for women coping with breast cancer.
“In London, I would have a nurse holding the patient’s hand, sitting with them, giving them a cup of tea,” says Sirohi, 45, in her 8-foot-by-8-foot (2.4-meter-by-2.4-meter) office. Ten floors below, hundreds of people shift on metal seats, lean against walls or lie on the stone floor waiting for doctors.
“Here, they have been given devastating news; I deliver it at least seven times a day,” she says of patients with terminal cancers for which there are no treatments. “Sometimes you do it for 23-year-olds, which is very tough.”
Cancer is sweeping through India, taxing its doctors and stressing a health-care system already overburdened by some of the world’s sickest people. The country is home to 17% of the global population but suffers from 21% of the disease burden, the World Health Organization says.
One person in India dies from cancer every 50 seconds. Hundreds of thousands more face surgery and years of treatment – driving a quarter of their households into poverty and making cancer the disease most likely to impoverish, according to the World Bank.
Breast cancer is gaining in alarming ways. A decade ago, it moved ahead of oral cancer, in which India ranks no.1 worldwide, to become the country’s fastest-growing malignant disease.
India will lose $20 billion in economic output from 2012 to 2030 as a result of breast cancer, the Harvard School of Public Health in Boston projects.

Survival rate
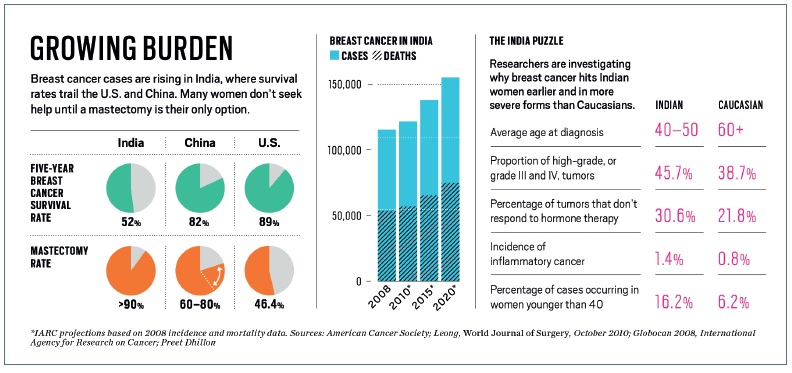
More than 115,000 new cases are diagnosed each year. The few treatment centers that track survival say 52% of breast cancer patients in India are alive after five years, a 2010 study published in The Lancet found. That pales in comparison with the 89% survival rate in the US and the 82% rate in China.
“The growing cancer burden threatens to overwhelm health systems and budgets in the developing world,” WHO Director General Margaret Chan told the organization’s International Agency for Research on Cancer in Lyon, France, on February 4 [2013].
Globally, cancer emerged as the no. 1 killer in 2010, when it passed ischemic heart disease. Today, it ends more lives than AIDS, malaria and tuberculosis combined. The economic toll: $1.16 trillion annually, or 1.6% of global gross domestic product.
Developing countries such as India face the brunt of the incursion. They report more than half of new cancer cases and two-thirds of deaths, compared with 15% of cases in 1970. At the same time, only 5% of global spending on cancer occurs in low- and middle-income countries, Harvard University researchers wrote in The Lancet in 2010.

‘Explosive change’
“It is an explosive change,” says Benjamin O. Anderson, a surgeon at Seattle’s Fred Hutchinson Cancer Research Center and chairman of the Breast Health Global Initiative, which provides guidelines for low- and middle-income countries. “The bomb already went off, and now the question is, how do we handle it?”
India can ill afford the rising number of cancer cases. Asia’s third-largest economy is contending with the slowest pace of growth in a decade – 5% in the year ended on March 31 [2013]. Foreign investors who have buoyed the nation are pulling money from Indian securities.
The country’s vaunted success in lifting 137 million people out of poverty may stall – a victim of spiraling costs and families who lose breadwinners as they battle cancer and other chronic diseases, says Srinath Reddy, president of the Public Health Foundation of India.
Spurning treatment
“Many people will not even be able to afford care and will forgo care,” says Vikram Rajan, a doctor and senior health specialist at the World Bank in New Delhi. “We cannot wait another 10 years to look at this problem. We have to look at this problem now.”
Even before the cancer scourge, India’s $65 billion health-care system was struggling to keep up: more than 300,000 babies each year fail to live beyond their first day, and one in 170 women die in childbirth or from pregnancy complications, according to Save the Children, which works to protect young people. India accounted for three of every five new leprosy cases in 2012 and a quarter of tuberculosis sufferers.
Now, cancer is exploding as more Indians live into their mid-60s, up from an average life expectancy of 50 before 1970. At the same time, the country is still battling such traditional killers as malaria and cholera.
Fresh threat
“We haven’t gotten over the infectious diseases yet, but the non-communicable ones are already on us,” says Harmala Gupta, who founded New Delhi-based CanSupport, a charity that has provided free medical services and support to more than 50,000 cancer patients.
Gupta, who herself beat a blood cancer called Hodgkin’s lymphoma more than 25 years ago, says breast cancer patients face special challenges.
Cultural taboos make many Indian women embarrassed to talk about their bodies. Held back by modesty, poverty or ignorance, they delay doctor visits when they find something wrong with their breasts.
When they finally get a checkup, their prognosis is often dire: in a third of cases, the tumor has spread to the skin or chest wall, making treatment less successful.
The lack of privacy at Indian hospitals exacerbates the problem. Gupta, 60, recalls the scene at a breast cancer clinic in a New Delhi public hospital in the mid-1990s.
Women humiliated
“They were asking women to disrobe, and they were palpating their breasts,” she says. “It was supposed to be cordoned off by curtains, but the curtains had frayed. Everyone was sitting there and watching these women. You could tell on their faces the humiliation.”
Indians with cancer are stigmatized, Gupta says.
“No one wants to talk about it,” she says. “They’re worried their children won’t get married because of arranged marriages in this country. People think it’s in the family. Children are taught to lie to their prospective marriage partners.”
Mumbai homemaker Deepti Shinde says she ignored swelling in her right breast, hoping the pain would go away. In October 2011, when she finally mustered the courage at age 47 to get the first breast exam of her life, the tumor that had formed in a milk duct was the size of a lime and had invaded nearby lymph nodes. Her only option for survival was a mastectomy, which she underwent in January 2012.
“I got really scared,” says Shinde, who quit school in 10th grade to work as a nanny and today shares a 10-foot-by-10-foot room and loft with her husband, 17-year-old son and five other relatives. “I didn’t know a whole lot about cancer at the time. I wondered if I would live.”
Shinde also worried about paying for surgery. Her doctor first referred her to a private hospital, where she was told the operation would cost 120,000 rupees ($1,950). The bill would have equated to almost a year’s income for her husband, a polio survivor who can work only part time as an electrician, and her brother-in-law, a laborer. She turned to Tata Memorial, where her mastectomy and two-night stay cost 5,000 rupees.
After the surgery, Shinde traveled to Tata from central Mumbai at least once a week for almost nine months. She arrived at 8 a.m. for 10 minutes of treatment. She never made it home until late afternoon.
“I used to just sit there, repeating God’s name,” she says of her six- to seven-hour waits. “It would feel like the day was never going to end.”
Shinde’s brother-in-law footed the bills for surgery and follow-up visits. A friend gave her money to help pay for chemotherapy, which she says cost 2,500 rupees per dose.
“Everybody in my family took care of me when I was sick,” Shinde says. “But it was hard on my family in terms of money.”
Cheaper drugs
India’s government is helping patients manage costs by allowing companies to make cheaper, generic cancer-fighting drugs. The Ministry of Health and Family Welfare has sought so-called compulsory licenses for versions of Bristol-Myers Squibb Co.’s Sprycel for chronic myeloid leukemia and Ixempra for breast cancer as well as Roche Holding AG’s breast cancer therapy Herceptin.
Roche introduced a lower-cost Herceptin packaged by a local pharmaceutical firm for the Indian market in August 2012. Natco Pharma Ltd. got government permission to make a cheaper copy of Nexavar, Bayer AG and Onyx Pharmaceuticals Inc.’s patented treatment for advanced kidney and liver cancer.
World Trade Organization rules allow such licenses to improve access to important medicines. The US, European Union and most of those regions’ drugmakers don’t like them. They lose money because they can’t sell the higher-priced versions of the drugs, which are protected by patents.
Unique features
Researchers are trying to unravel why breast cancer is rising in India – and why certain features there differ from elsewhere. Half of the cases can’t be explained by known risks, India’s Council of Medical Research found in a 2005 report.
The WHO links breast cancer to such choices as having no children, having children late in life, not breast-feeding, excessive weight gain and frequent alcohol consumption – practices often found in westernized lifestyles. In India, these potential triggers aren’t as common, and in many instances don’t exist at all.
“All the risk factors that have been identified in the West don’t seem to be operating here,” Gupta says. “These are women who have breast-fed their child. They marry early. Despite that, we are seeing this, and in younger women.”
 Younger women
Younger women
In India, breast cancer typically strikes women at age 45 to 50 – more than a decade earlier than in the West. Fewer cases in India involve protein molecules targeted by estrogen, the female hormone that stimulates breast cell division.
In about 45% of Indian cases, breast cancer cells possess receptors for estrogen. That compares with about 60 to 65% of cases in Western countries, says Rengaswamy Sankaranarayanan, the IARC’s head of early prevention and detection.
Doctors are interested in the estrogen receptor because it identifies women with a typically slower-growing disease who will benefit from hormone-based treatment, Sankarana- rayanan says. The absence of estrogen receptors in a greater percentage of Indian cases means proportionally fewer women will respond to hormone therapy.
“These are tumors that are likely to grow faster,” Sankaranarayanan says. Some doctors say rising obesity may be stoking the breast cancer increase. Obesity may boost levels of insulin and another hormone called insulin-like growth factor 1, which causes insulin resistance and may promote cancer development, according to the National Cancer Institute in Bethesda, Maryland. Yet colorectal and kidney cancers, which obesity also spurs, aren’t increasing significantly in India.
Cases like that of Mumbai resident Geeta Ambre, who has been afflicted with both breast cancer and Type 2 diabetes, may provide clues to possible links between the diseases. She was diagnosed with diabetes in 2001, when she was 40, and discovered a breast lump in 2011 as she was turning 50. Ambre had the lump checked out at Tata, where, she says, doctors put her mind at ease.
“I was scared and also too embarrassed to show it to anybody,” recalls Ambre, 53, who had never had a routine annual checkup or gynecological exam, even though she’s diabetic. Doctors found a fast-growing, grape-sized tumor that had spread to her lymph nodes. She had surgery to remove the lump in March 2011.

More aggressive
Sirohi, the Tata oncologist, helped supervise Ambre’s chemotherapy and sees her in the support group. She says Ambre’s tumor tested positive for a protein called human epidermal growth factor receptor 2, or HER2.
Cancers with this mutation tend to be more aggressive, and doctors speculate it may be more common in breast cancer patients in their 20s and 30s.
Preet Dhillon says researchers can learn a lot from Ambre and others with diabetes lurking in the background. An epidemiologist at the Public Health Foundation of India in New Delhi, Dhillon has been studying cancer patterns for six years.
She says if scientists can disentangle the mechanisms and disease-causing pathways that stem from body fat, insulin resistance and inflammation, they may find both diseases share the same cause in some cases.
Like breast cancer, diabetes typically turns up a decade earlier in Indians than in Caucasians. As many as 14% of urban Indian women have diabetes today, up from about 3% in 1972.
“It’s an avenue that needs to be explored, along with genetics and the environment, especially considering the burden of diabetes and associated syndromes,” says Dhillon, an American of Indian heritage who received her doctoral training at the University of Washington and Fred Hutchinson Cancer Research Center in Seattle and first came to India through an IARC fellowship in 2003.
Rajesh Dikshit, the chief epidemiologist at Tata Memorial, is trying to crack India’s breast cancer mysteries in a sixth-floor office that echoes with beeping horns from the street outside. He says many Indians die from cancer without ever being diagnosed, let alone treated.
Dikshit came to Tata six years ago after a two-year stint at the IARC in France and studies at Finland’s University of Tampere, where he got a PhD. He is exploring why a small number of women develop breast cancer in their mid- to late 20s.
 ‘Fastest growing’
‘Fastest growing’
“In the Mumbai population, breast cancer is the no. 1 fastest growing,” Dikshit, 49, says. “There are many cases with women that are less than 35 years of age in India.”
On this day in April, Dikshit pores over the blood-test results of 1,500 breast cancer patients and compares them with 1,500 women without the disease.
He’s searching for 384 DNA patterns to identify the most-common variations to figure out the biological factors that increase susceptibility to breast cancer. He says the research will reveal how changes in a woman’s body mass affect breast cancer development and whether doctors can use abdominal fat to predict risk.
Diabetes, heart disease and certain cancers are all linked to inflammation and the damage it causes, suggesting possible unifying drivers, he says. His findings on common genetic variations in breast tumors should be ready for submission to a scientific journal in early 2014, he says.
Dikshit is also looking for differences in nutrition and body mass in about 2,500 patients from urban and rural areas. He wants to compare them with about 2,000 women who don’t have breast cancer.
This study will identify whether young, rural women are at a higher peril of so-called triple-negative breast cancer, an aggressive form that doesn’t respond to three main drug therapies.
“It’s quite possible that the first 20 years of life are more important than their recent residential status,” he says.
Outside Dikshit’s office, 10 women enter patient records into a database. The electronic records enable the hospital to calculate the percentage of patients alive five years after diagnosis and identify which treatments have been successful.
Such efforts show how Tata is working to get a handle on the flood of cancer cases. Last year, 59,184 patients filed through the 700-bed hospital; 23,019 were admitted for treatment. India’s Department of Atomic Energy, which manages the hospital, deemed 60% of those treated too poor to pay for basic care – a cutoff usually set at a monthly income of 3,000 rupees [$40] or less.
Little privacy
The hospital’s annual expenditure is $40 million, equal to $1,738 per hospitalized patient. People who can afford to pay are treated individually in a private wing.
The MD Anderson Cancer Center in Houston, by comparison, had net patient revenue of $2.96 billion from 26,726 admissions in the year ended on August 31, 2012. That’s about $110,000 per hospitalized patient. For international clientele, Anderson provides a service that helps them decide what to pack.
Tata has no such luxuries. Government-subsidized patients usually share their first visit with two or more other people. At least three doctors discuss each new case – with everybody in the same room.
“The whole thing with patient confidentiality goes out the window,” says Sirohi, who, in addition to seeing 50 to 60 patients a day, also indirectly oversees the care of 40 to 50 more. “The alternative is, they don’t get the care at all.”

Cobalt, vinegar
Anderson, the Seattle breast surgeon, sees a silver lining in India’s handling of the overwhelming numbers: Tata has learned to make the most of what it has. For one thing, it relies on less-expensive technologies. Doctors use cobalt-powered units for radiotherapy, alongside more-expensive linear accelerators, and vinegar for cervical cancer screening instead of Pap tests.
“You look at this and think this is chaos, yet they’re doing it,” he says. “They really manage high volumes of patients with high-quality care.”
Ambre, the patient with Type 2 diabetes, returns to Tata every six months for a checkup.
“My friends – I’ve told them to do breast self-exams, and they are all doing them,” she says. “They were all scared by what happened to me, so now they keep checking themselves.” None has found a lump, she says.
Shinde is cancer-free and in good health after her mastectomy in 2012. She attends Sirohi’s meetings every month and in June began working an hour a day for a neighborhood moneylender.
“We are learning what to eat, what not to eat, how much to exercise,” she says. “I feel good after coming here. It’s possible to recover from this. What’s there to be afraid of?”
Shinde and Ambre can count themselves among India’s fortunate ones. Sirohi says she’s frustrated every day by the cancer she sees and can only chip away at.
“My hands are, in a way, tied because I want to do so much,” she says over breakfast at a Mumbai hotel. “You can’t. I don’t have the resources. People are so poor.”
“You feel for every patient,” she continues. “I want to fight for them because you are their best advocate – the only advocate.”






Leave a Reply