Future generations of trials must abandon [the traditional] method of patient selection and define eligibility by tumor biology… The era of breast cancer as a homogenous disease is no more. (Ode to a past Emperor, editorial by Angelo Di Leo and Catherine Oakman, JCO 2010)
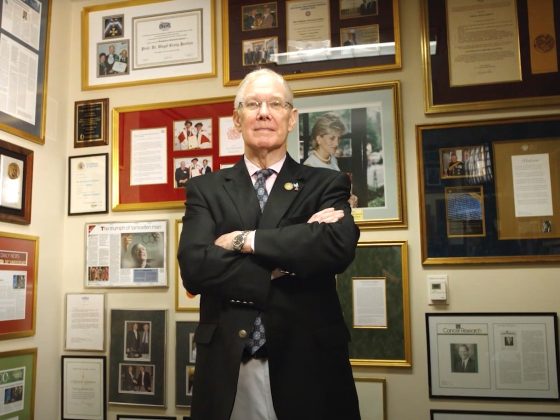
Angelo Di Leo, who died on 13 June, at only 58 years old, will be remembered as a great oncologist, breast cancer specialist, researcher and mentor – but above all as a leader in a period of great change.
If the point he made so clearly in that JCO editorial quoted above is now widely appreciated, it is thanks to people like Di Leo who understood the scale of the revolution that was happening in his field, recognised the huge challenge of getting the cancer community to change the way it did research and clinical decision making, and took a lead in arguing for and making that change.
Di Leo did his oncology training at Milan’s National Cancer Institute, where he worked between 1989 and 1996. This was a world leading centre for breast cancer, which over the previous two decades had pioneered breast conserving surgery techniques and launched the first adjuvant chemotherapy trials, which in turn heralded the start of truly multidisciplinary approaches to cancer treatment.
But it was a different challenge that awaited his generation. Advances in molecular biology techniques were transforming the understanding of cancer and cancer control, with the first targeted treatments coming over the horizon ‒ trastuzumab a monoclonal antibody used to treat breast cancers overexpressing HER2 and imatinib a tyrosine kinase inhibitor that targets the expression of the BCR-ABL protein use to treat chronic myeloid leukaemia.
In 1996 Di Leo chose to make a move to the Jules Bordet in Brussels, where he worked at the chemotherapy unit, and where, a year later, he was appointed Medical Director of the Breast European Adjuvant Studies team. It was a great strategic move. At the time, the Bordet Institute was not at all the international player it is now, but Martine Piccart had recently come on board, and was driving forward the targeted medicine agenda that would soon see breast lead the way in defining biological differences and exploring the implications for personalising treatments.
This is where Di Leo learnt about what can be achieved through close international collaboration among specialist centres. The year he arrived saw Piccart and the Bordet take a lead in setting up the Breast International Group, to bring together a highly fragmented research picture into a structure designed to pursue the new type of translational research programmes that would be need to rapidly translate scientific discoveries into the clinic.
Di Leo, himself, focused his research principally on trying to find ways to identify which breast cancer patients respond to which chemotherapies, to reduce the number of patients who derive little or no benefit from these toxic treatments.
It was an extraordinarily exciting time both in breast cancer and for the Bordet, which would eventually go on to lead the milestone MINDACT trial, the first prospective clinical validation of a genomic tool to identify which patients would need adjuvant chemotherapy and which could be spared.
But by 2003, Di Leo was ready to move back to Italy. With his track record and experience he could no doubt have had his pick of leading oncology centres to sign up with. He chose instead to set up a new oncology department, from scratch, in Prato, where he established a laboratory, built up translational research programmes, participated in international research groups including BIG and the Early Breast Cancer Trialists Cooperative group, and mentored a new generation of clinical researchers.
Like all good leaders, while the first breakthrough for targeted cancer treatments happened early in his career, Di Leo was quick to see beyond the hype. While so many opinion leaders were starting their sentences with “Take imatinib for example…” Di Leo understood quite quickly that the targeted anti-cancer drugs that followed on would not be the game changers everyone had been hoping for.
He was at the forefront of research that took a closer look at individual tumours, revealing that the biology of solid tumours can vary in important ways from one part of the tumour to another, between the primary and the secondaries, and also over time.
But he was also quick to recognise and warn against the dangers of oncologists obsessing over the precise biology of every tumour and forgetting about the patient. In an interview with Cancer World in 2010, he said “People come up to me in conferences and ask, ‘What is the first-line treatment for metastatic breast cancer?’ I say, ‘I don’t know – it depends on the patient in front of you.’ You can’t possibly map out an algorithm for late-stage disease as there are so many variables, such as the patient’s preferences for the level of aggressiveness of treatment, how and when drugs are taken, whether they can tolerate hair loss and other side-effects, and so on.”
In terms of the practice at his department, he said, that meant giving every patient 45 minutes for their first appointment, and setting aside one day a week exclusively for patients and families to come and talk through their situations and concerns.
Like all good leaders, Di Leo took great pains to develop the next generation, and invested heavily in mentoring younger members of his team. He was one of the few Europeans to serve on the ASCO committee that oversees grant selection for young investigators, and took every opportunity to send his more junior staff to international conferences and give them the all-important first authorship on research papers.
Di Leo’s great contribution was recognised by the European Society for Medical Oncology in 2019 with a Lifetime Achievement Award “in tribute to his outstanding career dedicated to cancer research and education.”
On receiving the award, Di Leo, who knew at the time he had an incurable condition that would limit his life, said “I believe I have had two big achievements in my career: one has been to create this place in Prato, starting from nothing, where people now come to be cured of such a critical disease as cancer, with a lot of confidence in our programme. The other is that I have had the opportunity to work with and develop a team of young, extremely skilled oncologists and researchers – I am proud to say that the programme will successfully continue without me one day.”
It’s a great legacy, and the programme will undoubtedly continue successfully thanks to the strong foundation he laid and the attention he paid to developing the next generation of leaders. But filling the shoes of such a great scientist, clinician and leaders will be a big ask.
He leaves a daughter, Federica, and wife, Laura Biganzoli, who is a leader in geriatric oncology, and worked alongside Di Leo at the Prato Hospital, where she continues to work as Coordinator of the Breast Unit, and to research new biomarkers to predict the risk of breast cancer recurrence.
Further reading: Angelo Di Leo: mapping the geography of breast cancer