The use of artificial intelligence might increase the speed and the consistency of cancer diagnosis, but could also exacerbate the problem of overdiagnosis, according to a perspective article recently published in the New England Journal of Medicine by Adewole Adamson and Gilbert Welch, who suggest that this risk may be mitigated by overcoming the dichotomous classification between “cancer” and “not cancer”.
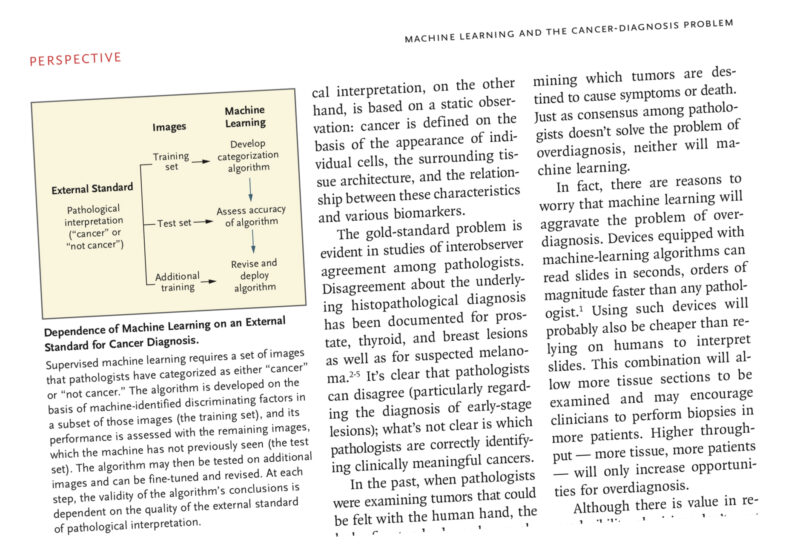
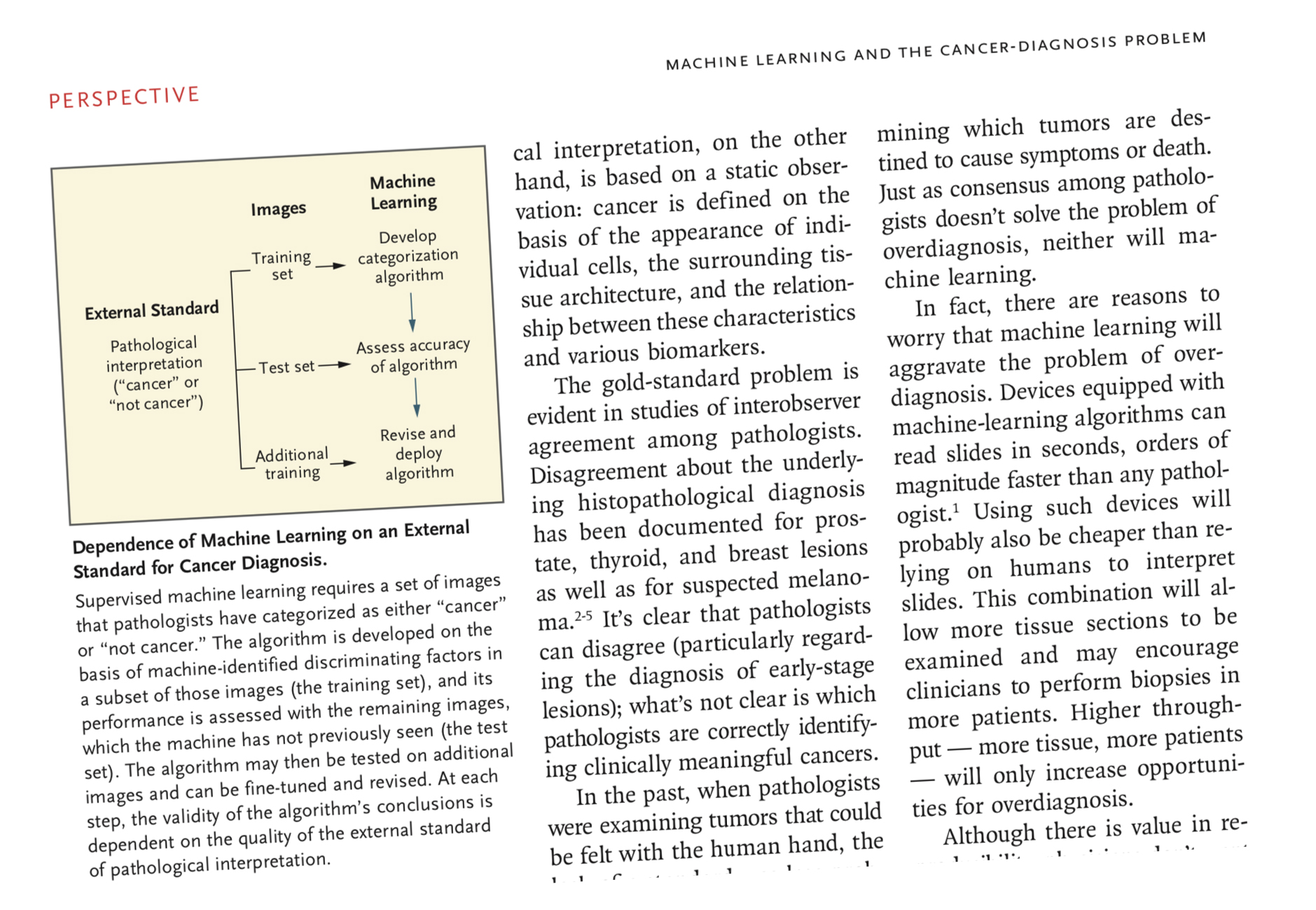
 Supervised machine learning consists in the generation of decision-making algorithms starting from sets of images that pathologists have categorized as either “cancer” or “not cancer.” “The computer system learns by judging its diagnosis against the external standard of pathological interpretation” Adewole Adamson, assistant professor of Internal Medicine at Dell Medical School at the University of Texas, explains. “Reliance on this external standard is problematic, however, since machine learning doesn’t solve the central problem associated with cancer diagnosis: the lack of a histopathological gold standard.”
Supervised machine learning consists in the generation of decision-making algorithms starting from sets of images that pathologists have categorized as either “cancer” or “not cancer.” “The computer system learns by judging its diagnosis against the external standard of pathological interpretation” Adewole Adamson, assistant professor of Internal Medicine at Dell Medical School at the University of Texas, explains. “Reliance on this external standard is problematic, however, since machine learning doesn’t solve the central problem associated with cancer diagnosis: the lack of a histopathological gold standard.”
There is no single right answer to the question: “What constitutes cancer?” In fact, some microscopic cellular abnormalities may meet the pathological definition of cancer but may not be destined to cause symptoms or death. Since AI allows to analyse images in a faster and cheaper way, clinicians may be encouraged to request more exams, boosting opportunities for overdiagnosis.
“One approach to mitigating this problem would be to make use of the information manifested by disagreements regarding pathology” Gilbert Welch, senior investigator at Brigham’s Centre for Surgery and Public Health, Brigham Women’s Hospital in Boston, suggests. “In other words, using an external
standard based on judgments from a diverse panel of pathologists, algorithms could be trained to discriminate among three categories: total agreement regarding the presence of cancer, total agreement regarding the absence of cancer, and disagreement regarding whether cancer is present.” Lesions that are of uncertain significance should deserve further attention by the pathologist and, possibly, a conservative approach from the oncologist.
“Ultimately, what matters to patients and clinicians is whether the diagnosis of cancer has relevance to the length or quality of life” the authors conclude. “We believe that the possibility of training machine-learning algorithms to recognize an intermediate category between “cancer” and “not cancer” should be given serious consideration before this technology is widely adopted.”