Patients with metastatic non-squamous non-small-cell lung cancer (NSCLC), prostate cancers, ovarian cancers and cholangiocarcinoma should be offered next-generation sequencing (NGS) for profiling tumour samples, concludes an expert panel from the European Society for Medical Oncology (ESMO) in their review (Mosele F et al. Ann Oncol 2020) published in Annals of Oncology (August 24).
“These are the first recommendations from a scientific society about the use of NGS,” said Dr Fernanda Mosele, the first author of the paper, from Gustave Roussy, Villejuif, France. “Our intent is that they will unify decision-making about how NGS should be used in patients with metastatic cancer.”
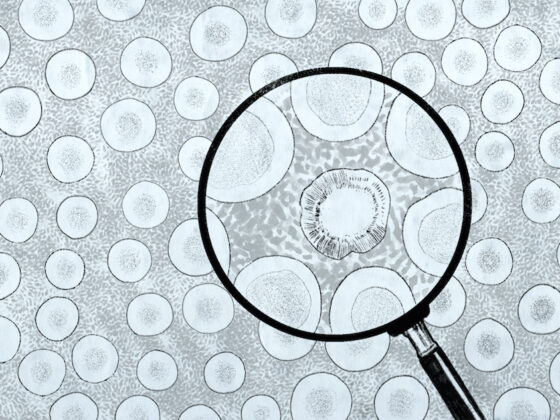
NGS is a sequencing technology that assesses high numbers of nucleotides in a short time frame with the aim of selecting targeted treatments according to mutations detected. While it has been widely implemented, until now, no recommendations have been issued regarding use in daily practice.
The ESMO Translational Research and Precision Medicine Working Group (Mateo J et al. Ann Oncol 2018) developed the new recommendations using the ESMO Scale for Clinical Actionability of molecular Targets (ESCAT). This scale is a framework that ranks a match between drug and genomic alterations, according to actionability. For example, ESCAT level I means that the match of an alteration and drug has been validated in clinical trials; while ESCAT level III includes alterations validated in another cancer, but not in the disease-to-treat. For the current recommendations, all recurrent genomic alterations were identified in the eight cancers considered responsible for the most deaths worldwide. Then the ESCAT score was determined for each alteration. Finally, from the prevalence of alterations for each tumour type and the ESCAT ranking, the authors calculated the number of patients who would need to be tested with NGS to identify one patient who could be matched to an effective drug in daily practice.
In the paper, ESMO makes recommendations at three different levels.
- From the public health perspective, the authors recommend NGS should be used routinely in patients with metastatic lung adenocarcinoma, prostate cancer, ovarian cancer, and cholangiocarcinoma. In these tumours, large multigene panels could be used if they add acceptable extra cost compared with small panels. Additionally, based on the KN158 trial it is recommended to test tumour mutational burden (TMB) in well-and moderately-differentiated neuroendocrine tumours (NETs), cervical, salivary, thyroid and vulvar cancers, as TMB predicts response to the anti-PD-1 antibody pembrolizumab in these cancers.
- From the clinical research perspective, centres should perform NGS to generate more evidence about use of this method and accelerate drug development.
- From the patient-centric perspective, patients with other cancers can decide with their doctors to order NGS on a large panel of genes – providing there is no extra cost for the public healthcare system and the patient is informed about the relative likelihood of benefit.
The review found there to be no current indications for NGS in breast, squamous-cell lung, gastric, pancreatic, or hepatocellular carcinoma. However, the authors concluded that as new data emerge for novel therapies across tumour types the recommendations will need to be updated.
Commenting on the publication, Ruth Plummer, Professor of Experimental Cancer Medicine at Newcastle University, UK, said, “These ESMO guidelines are an excellent distillation of the current data and provide clear recommendations for the tumour types where there is the best evidence NGS might be of benefit. They also provide a very comprehensive summary of the trial data available.”
For routine clinical practice, she said, the guidelines will help physicians in discussions with patients about the benefits of having an NGS panel run on their tumour sample, and help guide NGS sequencing when resources are limited. In general, NGS sequencing for all patients with NSCLC, prostate cancers, ovarian cancers and cholangiocarcinoma, she added, was not currently available in all cancer centres across Europe. “Having clear European guidelines from ESMO will help inform discussions as health services move towards establishing routine NGS for cancer patients,” said Professor Plummer, who is deputy chair of the Cancer Drug Development Forum.