Adding a drug currently used against idiopathic pulmonary fibrosis to chemotherapy in the neoadjuvant setting increased event-free survival in patients with early HER2-negative breast cancer. The study, published in Clinical Cancer Research, 16 September, found that high levels of fibrosis in the microenvironment predicted poor outcomes, and that those poorer outcomes could be corrected by the anti-fibrotic drug nintedanib.
“This strategy defines a pathway toward more personalised and lower-cost treatment paradigms for breast cancer and represents the first successful clinical application targeting tumor fibrosis in oncology,” write the authors, led by Ghassan Mouneimne, from the University of Arizona Cancer Center, in Tucson, Arizona.
Tumour stiffening is a feature of the progression of breast cancer, producing a varied microenvironment ‘landscape’, which ranges from normal elasticity to fibrotic-like tissue stiffness. The stiffness is caused by the extracellular matrix (the network of proteins and other molecules surrounding cells) having increased collagen deposition, which increases the tissue rigidity/stiffness. “Whether a tissue is fibrotic or not is largely determined by the amount of collagen fibres secreted by fibroblasts and whether bundled and cross-linked together,” Mouneimne tells Cancerworld.
When cancer cells are surrounded by stiff matrix, the physical resistance triggers ‘mechanotransduction’, defined as a rapid conversion of mechanical stimuli into biochemical signals. Mechanotransduction has been shown to promote the first steps of metastasis by increasing cytoskeletal dynamics, cell migration, and invasion in situ. A study published in Nature Nanotechnology in 2012 showed that extracellular matrix stiffening was implicated in tumour progression.
A fundamental aspect of the current study is the mechanical conditioning (MeCo) score that Mouneimne and Adam Watson devised to provide a quantitative measure of how cancer cells become influenced by stiffness in their extracellular matrix. In a study published in Cell Reports in 2021, they developed tissue culture in vitro models exposing breast cancer cell lines to hydrogels with both high and low levels of stiffness. Next, they performed RNA sequencing gene expression analysis to see which genes were ’dialed up and down’ in the cancer cells in the soft and stiff matrices. Differential expression analysis revealed that 930 genes were upregulated and 1,795 downregulated by >2 fold increases in stiffness. The gene sets were then further refined to develop the MeCo score, which was then validated using long-term survival data from four studies involving more than 2500 patients. “The MeCo score is not a biomarker of fibrosis, but rather a biomarker of the response to fibrosis, a measure of the problematic potential of the actual cancer cells that will exert a devastating effect when they migrate to a different setting during metastasis,” explains Mouneimne.
For the current analysis, Mouneimne calculated MeCo scores for patients who had previously taken part in an earlier Phase 2 trial exploring whether the drug nintedanib had anti-angiogenic properties in HER2 negative breast cancer.
For the study, originally undertaken by Miguel Quintela Fandino from the Spanish National Cancer Research Centre (first published in British Journal of Cancer in 2014), 130 patients with early HER2-negative breast cancer were randomised 1:1 to the experimental arm, receiving nintedanib plus paclitaxel in the neoadjuvant setting prior to surgery, or the control arm, receiving just paclitaxel.
Nintedanib was of interest in the treatment of fibrosis, because it is an agent known to exert a powerful anti-fibrotic activity through blockade of the fibroblast growth factor receptor (FGFR) family. Notably, it was the first disease-modifying therapy approved for idiopathic lung fibrosis.
For the current analysis, the team generated RNA sequence data from patients in the earlier 2014 study, which enabled them to calculate baseline MeCo scores. These scores could then be compared with data on survival outcomes after the team collected long-term follow-up data from all the study sites. Patients were divided into high MeCo scores (prespecified as above the median) and low MeCo scores (below the median). For the new analysis, this gave rise to four separate patient groups: those with high MeCo scores treated with nintedanib, those with high scores who were not treated with nintedanib, those with low scores who were treated with nintedanib, and those with low scores who were not treated with nintedanib.
Results at a median follow-up of 9.67 years showed median event-free survival was not statistically different overall between the experimental arm who received nintedanib and the control arm who did not receive nintedanib (P=0.37).
However, when patients were split according to their MeCo score, the results suggest a positive therapeutic effect for nintedanib, specific to patients with fibrotic high MeCo tumours. In the control arm (who did not receive nintedanib), patients with high MeCo scores had statistically higher relapse rates than those with low scores (HR=0.21; P=0.0075). In the experimental arm, however, that higher risk was corrected by nintedanib, resulting in no statistical difference between patients with high versus low MeCo scores (HR=0.37; P=0.16).
Furthermore, nintedanib demonstrated pharmacodynamic engagement, reducing the MeCo score by 25% during the run-in phase of the trial (P<0.01).
“When patients are split by their MeCo score, the results suggest a positive therapeutic effect of nintedanib that is specific for fibrotic High MeCo tumors. In the absence of anti-fibrotic treatment, patients with elevated scores suffer from a very aggressive disease course,” conclude the authors.
Introducing nintedanib into the neoadjuvant setting, they believe, has the potential to increase overall survival in some patients with high levels of fibrosis. “By offering a specific therapy targeting the biological feature identified by the MeCo score, nintedanib could provide a rational therapeutic option for high-risk groups,” write the authors. Importantly, the approach would be cost-effective, adds Mouneimne, since nintedanib is now off-patent.
The team are currently looking to develop cancer-specific MeCo scores for prostate and colorectal cancers, and are in the early stages of planning a prospective multicentre trial using the MeCo score test to inform nintedanib use in patients with luminal ER-positive breast cancer. Pavani Chalasani, from the George Washington Cancer Center, Washington DC, will be the principal investigator. “Ultimately, we hope that patients will be able to get access to their MeCo scores to decide whether they would benefit from anti-fibrotic therapy in the neoadjuvant setting before surgery,” says Mouneimne.
Reducing fibrosis in the microenvironment, he adds, is likely to deliver additional benefits, including allowing drugs to more easily access the cancer cells and influencing the immune system.
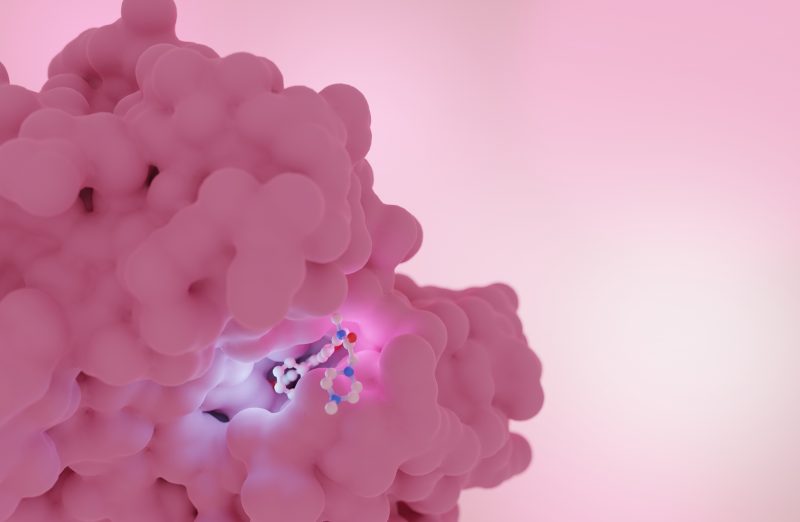
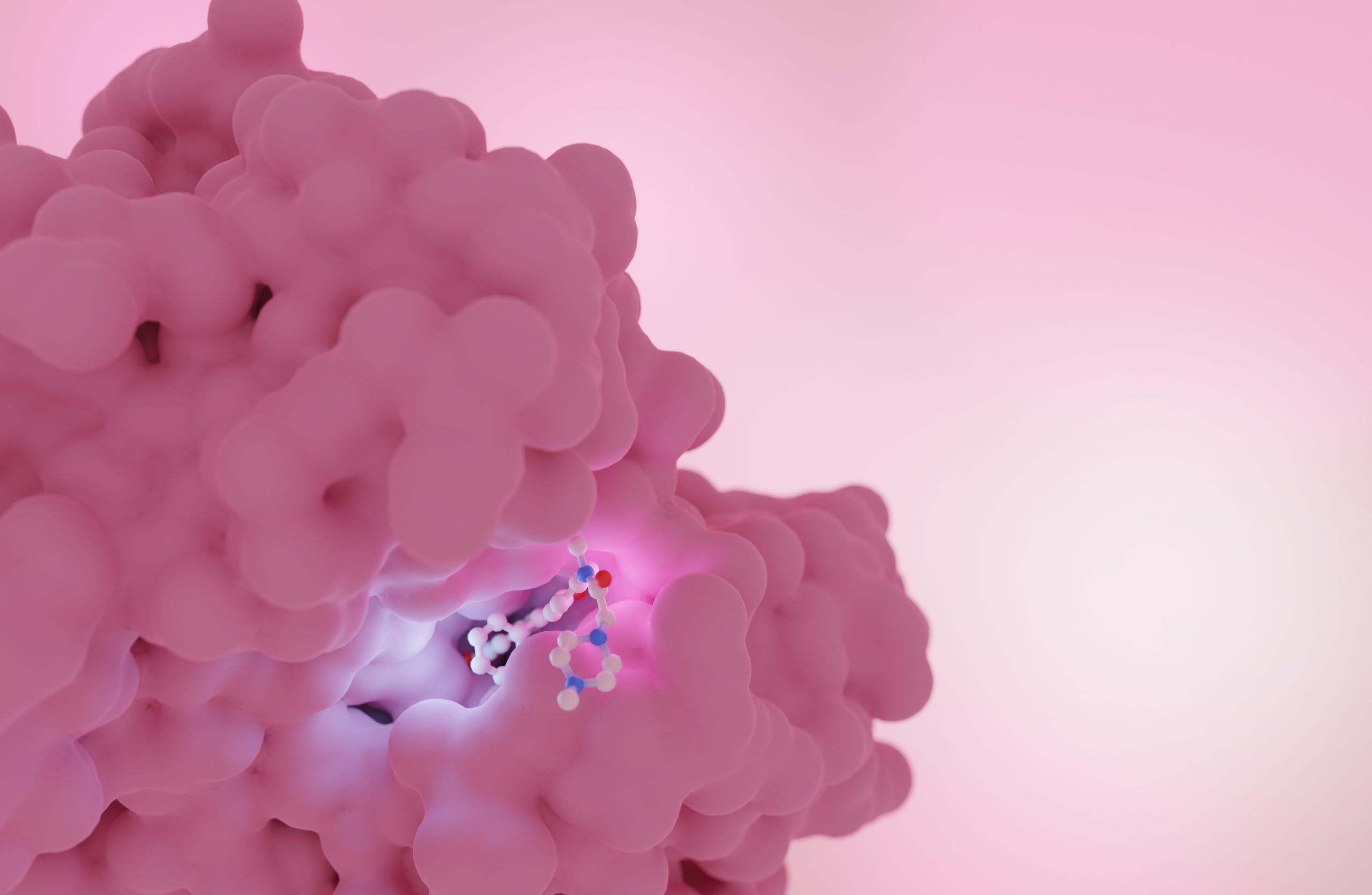
The opening illustration shows a rendering of nintedanib bound to its target in the RET protein tyrosine kinase domain (PDB ID: 6NEC). Artistic rendering made by Behnoush Hajian.