At a cancer forum not long ago, after I introduced myself as an orthopaedic surgery resident, someone asked — with genuine curiosity — “But why are you here?” The question stayed with me, because it revealed a paradox: musculoskeletal health professionals are often seen as peripheral to oncology, yet bones, muscles, and movement lie at the heart of living with and beyond cancer. Patients sustain pathological fractures, lose mobility, struggle with sarcopenia. Their independence and dignity, their ability to stand on their own feet, often depend on musculoskeletal health. This brings us to the real question for the cancer community: is it pragmatic, is it plausible — and above all, is it needed — to expand the mandate of musculoskeletal health professionals in cancer prevention, control, and care?
Current Status
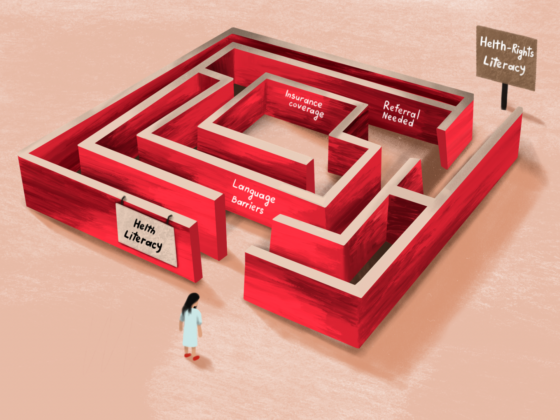
Musculoskeletal professionals are already involved in cancer care — but in disease-specific ways that may be fragmented from the continuum of cancer care. Orthopaedic oncologists provide highly specialised surgery for bone and soft-tissue sarcomas, a rare field centralised in a few expert centres. Orthopaedic and spine surgeons treat metastatic bone disease, often faced with controversies, such as whether biopsies should be routine during vertebroplasty to detect occult cancers. Physiotherapists and rehabilitation physicians play an important supportive role throughout treatment, yet their services may remain unevenly integrated and underfunded.
There is however, space and need for more action from musculoskeletal health professionals. Bone metastases affect approximately 54 and 89% of patients with advanced breast or prostate cancer, respectively, while skeletal-related events such as fractures or spinal cord compression drive morbidity and cost.1 Sarcopenia and frailty, affecting 30–50% of cancer survivors, predict poorer outcomes and limit treatment options.2 Despite this, cancer rarely features in the core curricula of orthopaedics, rehabilitation, or physiotherapy training — apart from focused modules in subspecialties such as musculoskeletal oncology or paediatric orthopaedics. The result is a professional community that has the potential to accompany the cancer journey, but without systematic preparation, recognition, or policy mandate to do so.
A Play in Three Acts – Clinic, Research and Policy
Contemporary cancer care emphasizes both survival and quality of life, rendering the services of musculoskeletal health professionals essential. Standardising musculoskeletal follow-ups could prevent debilitating complications. These include early detection of bone metastases that precede fractures, routine frailty and fall-risk assessments, and proactive physiotherapy or surgical stabilisation where indicated. Simple tools such as DXA scans, FRAX adapted for oncology, and functional assessments like the Timed Up and Go test could be embedded into survivorship clinics as readily as blood counts are checked in oncology visits. Beyond complication management, the musculoskeletal health community could drive prevention — aligning with Europe’s “Cancer Code” recommendation on physical activity. Active social prescribing of exercise, safe-sport counselling, and community programmes led by rehabilitation specialists would strengthen both primary prevention and survivorship care.
“Be physically active in everyday life. Limit the time you spend sitting.”
European Code Against Cancer (2014, EC/WHO/IARC)
A stronger evidence base is essential. Musculoskeletal outcomes could be systematically captured in cancer registries, tracking fractures, mobility, falls, and quality of life using validated instruments such as the MSTS score, PROMIS mobility, or the EORTC QLQ modules. Translational research could link the effect of chemotherapy, radiotherapy, and hormonal therapy on bone and muscle biology to indications for physiotherapy, assistive devices, or even prophylactic surgery. In exercise oncology, musculoskeletal expertise is crucial to refining which regimens improve not only cancer-specific outcomes but also independence and function.3 With musculoskeletal data integrated into cancer registries, the evidence gap that sidelines musculoskeletal health professionals could be bridged.
Finally, musculoskeletal health needs to be recognised in cancer strategies at the policy level. Formal involvement in national cancer control plans, WHO rehabilitation frameworks, and survivorship guidelines would legitimise and fund these roles. Representation in conferences, consultations, and research consortia can strengthen cross-sector links — from orthopaedics and rehabilitation to sports medicine and industry. Athletic events could serve as platforms promoting exercise as prevention. Harnessing partnerships with implant and surgical planning ventures could create momentum mobility interventions focused on cancer patients and survivors. Policy presence often serves as a lever transforming isolated good practice into system-wide change.
“Rehabilitation is relevant to the needs of people with many health conditions and those experiencing disability across the lifespan and across all levels of health care.”
WHO Rehabilitation 2030 initiative, 2017

Recommendations – The Way Forward
The way forward requires both structure and experimentation. A top-down approach would mean developing frameworks, curricula, and guidelines: oncology modules in orthopaedic and physiotherapy training, multidisciplinary working groups within cancer societies, and inclusion of musculoskeletal indicators in national cancer registries. International working groups and dedicated sessions at major oncological and orthopaedic conferences could set shared agendas and track progress through yearly reports.
At the same time, a bottom-up approach is equally necessary. Pilot programmes in hospitals and communities could test practical models: joint survivorship clinics that integrate physiotherapy and orthopaedics, structured exercise prescription embedded in routine oncology visits, or twinning programmes increasing mutual understanding of healthcare professionals in oncology and musculoskeletal health and care. Patients themselves should be invited to shape these initiatives, ensuring that services reflect real needs and lived experiences.
The most pragmatic path is a combination of both: a framework that provides legitimacy and resources, and grassroots use-cases that prove feasibility and generate evidence. A concrete start could be an inaugural “Call to Action” published jointly by cancer and musculoskeletal societies, followed by structured exchanges of knowledge, annual progress reports, and international twinning opportunities for the next generation of professionals.
Conclusion
Expanding the role of musculoskeletal professionals in cancer care is not about rivalry or reshaping hierarchies — it is about collaboration. By joining forces across disciplines, we can prevent avoidable fractures, preserve independence, and embed exercise and rehabilitation into every stage of the cancer journey. The goal is simple but powerful: better care, together, for every patient living with and beyond cancer and for every individual who can diminish their cancer risk.
References
- Huang JF, Shen J, Li X, et al. Incidence of patients with bone metastases at diagnosis of solid tumors in adults: a large population-based study. Ann Transl Med. 2020;8(7):482. doi:10.21037/atm.2020.03.55
- Surov A, Wienke A. Prevalence of sarcopenia in patients with solid tumors: A meta-analysis based on 81,814 patients. JPEN J Parenter Enteral Nutr. 2022;46(8):1761-1768. doi:10.1002/jpen.2415
- Watson G, Coyne Z, Houlihan E, Leonard G. Exercise oncology: an emerging discipline in the cancer care continuum. Postgrad Med. 2022;134(1):26-36. doi:10.1080/00325481.2021.2009683