Project sites in seven low-income countries have reached the 90% targets set by the World Health Organization (WHO) for treating women identified with pre-cancerous lesions.
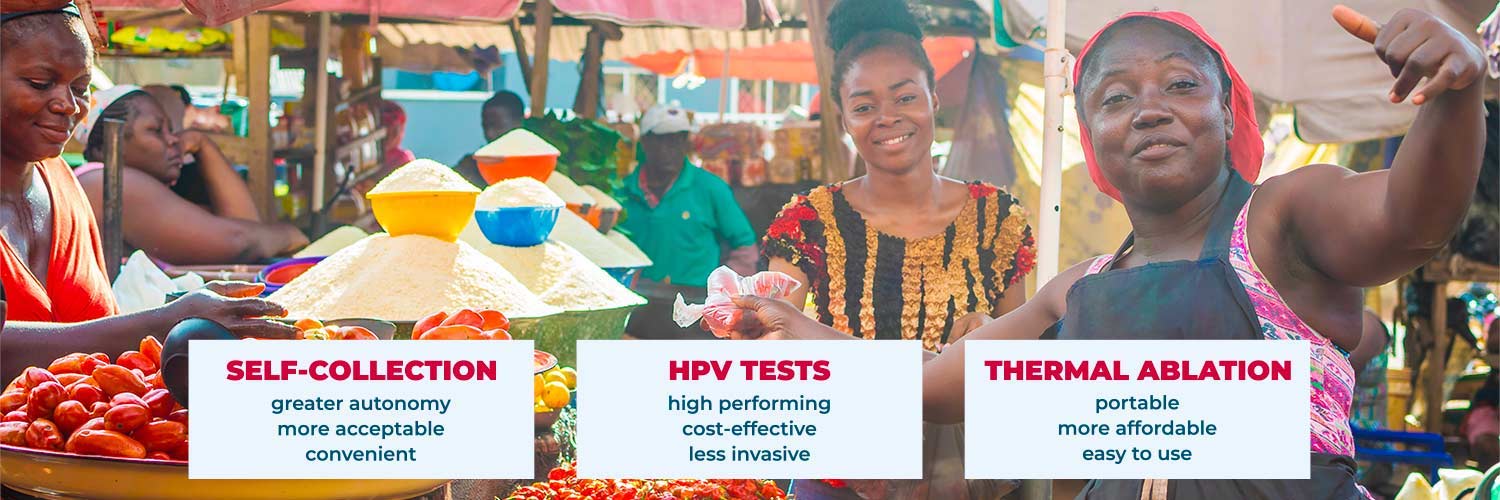
This success was achieved using a model of cervical cancer elimination developed for use in low-income and community settings that integrates HPV screening with the use of hand-held, battery- powered thermal ablation for treating pre-cancerous lesions.
The projects, running in Burkina Faso, Côte d’Ivoire, Malawi, Nigeria, Philippines, Rwanda and Senegal, are part of global efforts to achieve the WHO goals for a sustained reduction in the incidence of cervical cancer in every country to no more than four cases per 100,000 women by 2030.
The target of delivering treatment to 90% of women identified with cervical disease (pre-cancerous and cancerous) is one of three targets set by the WHO – the other two being delivering screening with a ‘high-performance test’ to 70% of women between ages 35 and 45, and fully vaccinating 90% of girls by age 15.
Screening programmes in the seven countries have reached more than 50% of women with HPV tests, showing strong progress towards achieving the 70% screening target as well.
Thermal ablation for pre-cancerous lesions
The use of thermal ablation to treat pre-cancerous cervical lesions is seen as an important contribution to reaching the 90% treatment target, particularly in low-income countries. It has a number of advantages over cryotherapy, the standard non-invasive treatment option, which uses extreme cold to kill the pre-cancerous cells, takes about 15 minutes to administer, and requires compressed gas – nitrous oxide or high-quality carbon dioxide – which can be hard for poor countries to procure.
Thermal ablation, by contrast, is a quick outpatient procedure: treatment takes about one minute, and can be performed by a range of health workers, including physicians, nurses, and midwives, working in a variety of settings, including primary health care facilities and out-reach settings.
The projects in the seven countries are among 14 such projects funded by Unitaid and implemented in partnership with the Clinton Health Access Initiative (CHAI) and the SUCCESS consortium (Expertise France, Jhpeigo and the Union for International Cancer Control).
Thermal ablation takes about one minute, and can be performed by a range of health workers, working in a variety of settings
To facilitate uptake, pricing agreements secured by Unitaid and CHAI have reduced the cost of thermal ablation devices by nearly 45% and HPV tests by nearly 40%. Field data from countries show that the overall cost of thermal ablation is nearly ten times less than cryotherapy per woman treated. HPV tests cost $5–15 (depending on the manufacturer) at the prices negotiated through the Unitaid-supported project.
Nine out of ten cervical cancer deaths worldwide occur in low- and middle-income countries. Lack of progress against this highly preventable disease is widely attributed to a combination of lack of awareness and financing, as well as high costs, ineffective screening methods, and poorly adapted treatment devices. The hope is that the model that has shown early success in projects in the seven low-income countries can be scaled up and adopted/adapted much more widely.
“We hope our success so far will inspire more countries and partners to implement programs to help protect the health of women and provide better access to crucial treatments,” said Joshua Chu, Executive Vice President, Vaccines and Non-Communicable Diseases, at CHAI.
Rolling out the model
Uganda is one of the 14 countries running cervical cancer screening and elimination projects funded by Unitaid. It has started to use thermal ablation devices to treat pre-cancerous cervical lesions identified at screening, but has not yet been reported as hitting the target of treating 90% of these lesions.
In November 2022, a study on the experiences and acceptability of thermal ablation to treat pre-cancerous cervical lesions, carried out in the Mayuge district in the east of the country, reported that 98% of women treated that way said they would recommend the treatment to others.
For Andrew Musoke, Country Director at Clinton Health Access Initiative in Uganda, the priority has to be rolling out high-quality screening, particularly to women living with HIV, who are six times more likely to develop cervical cancer than women without HIV, he says.
“Right now, in Uganda the screening rate is only 30% among women living with HIV, and less than 10% for the general population”
As Musoke points out, while reaching the target of 90% treatment of identified pre-cancers is important, the impact is limited if only a small proportion of those at risk are being screened. Right now, in Uganda the screening rate is only 30% among women living with HIV, and less than 10% for the general population.
“Delivering an effective HPV testing service requires investment into the sample transport, lab capacity, and patient navigation systems to ensure that women receive timely and accurate results,” he says.
Where it has been possible to build on existing healthcare services for HIV populations, he adds, that screening rate goes beyond the WHO target of 70%. “For women attending ART [antiretroviral therapy] clinics at priority HPV sites, the rate is much higher – about 75%… It is recognised that there is an urgent need to scale up access to screening services to reach the full target population.”
Implementing high-performance screening among a large proportion of the target population, and at the recommended frequency (which in Uganda is every five years, or every three years for women living with HIV), will catch most pre-cancers before they become cancers, says Musoke – just as routine screening implemented at scale substantially reduced cervical cancer incidence in high-income countries even before the HPV vaccine was introduced.
Across the project’s partner countries, the screening programmes are picking up around 30 times more cases identified as pre-cancer than suspected invasive cancer, he adds, which means the thermal ablation treatment model could have a major preventive impact.
Women identified with invasive cervical cancer will still need to be referred for surgical excision at a centre of excellence, which in Uganda would be at the Uganda Cancer Institute in Kampala.
Building momentum
The recent progress towards preventing cervical cancer in the project countries and elsewhere comes on the back of the call issued by the WHO in May 2018 for the global elimination of cervical cancer, commented Tracey Shissler, Implementation Director at the international non-profit health organisation Jhpiego, which is part of the SUCCESS coalition alongside Expertise France and the Union for International Cancer Control.
“We are seeing incredible progress on introduction and adoption of new secondary prevention approaches… This innovations journey underscores that healthcare system thinking is critical to see increased gains and see cervical cancer prevention integrated and financed into routine women’s health and HIV services,” she said.
“Now it comes down to access for all women,” said Philippe Duneton, Executive Director of Unitaid, the global health organisation that is funding the projects through an investment of US$60 million aimed at making improvements in the screening and treatment of women with cervical cancer in poorer countries. “We must see concerted urgent action from governments and partners to scale up these models and bring an end to cervical cancer for generations to come.”