Substantial increases in the number of avoidable cancer deaths in England are predicted as a result of diagnostic delays due to the COVID-19 pandemic, report two modeling studies published in the August issue of Lancet Oncology. Both studies underline the urgent need in the time of COVID-19 for public education programmes to be introduced across Europe to encourage people to seek medical advice for cancer symptoms.
The national lockdown, introduced across the UK on March 23rd, 2020, has been associated with a decrease in, or cessation of most non-COVID-19 National Health Service (NHS) activities. Of great concern has been the effect on cancer patients, where the only routes to diagnosis have been by urgent ‘two-week referral pathways’ for suspected cancer, initiated by the GP (primary care physician), or through direct presentation to emergency departments. Cancer screening services and routine non-urgent diagnostic work initiated by primary and secondary care teams were both suspended. “Whilst currently attention is being focused on diagnostic pathways where cancer is suspected, the issue is that a significant number of cancers are diagnosed in patients awaiting investigation for symptoms not considered related to cancer,” explains Ajay Aggarwal, one of the authors, in a press release from the London School of Hygiene & Tropical Medicine (LSHTM).
In the first study, Aggarwal and colleagues used a retrospective population cohort, extracting NHS cancer administrative data for more than 93,000 cancer patients (aged 15-84) diagnosed with breast, lung, colorectal and oesophageal cancer between 2010 and 2012. Of the patients identified, 32,583 had breast cancer, 29,305 lung cancer, 24,975 colorectal cancer and 6,744 oesophageal cancer.
Assuming incidence remains relatively stable year on year, the authors estimated the subsequent impact on survival by reallocating patients from screening and non-urgent routine referral pathways (from GPs and secondary care) to urgent two-week wait referral routes and emergency department presentations. The analysis was undertaken according to three reallocation scenarios, providing best- and worst-case survival estimates.
The results showed:
- Across the three scenarios, up to five years after diagnosis of breast, colorectal, lung and oesophageal cancers there are estimated to be an additional 3,291‒3,621 deaths, and an additional 59,204‒63,229 total years of life lost (YLLs).
- For breast cancer, across the three scenarios over five years, there was estimated to be 7.9‒9.6% increase in the number of deaths, corresponding to between 281 and 344 additional deaths.
- For colorectal cancer, there was estimated to be a 15.3‒16.6% increase in number of deaths, corresponding to between 1,445 and 1,563 additional deaths. For lung cancer there was estimated to be a 4.8‒5.3 % increase in number of deaths, corresponding to between 1,235 and 1,372 additional deaths.
- For oesphageal cancer there was estimated to be a 5.8‒6.0% increase in the number of deaths, corresponding to between 330 and 342 additional deaths.
“These data are essential for policy makers to drive changes in national lockdown and stay-at-home messaging, and to urgently reduce diagnostic delays, particularly for routine investigations, through outreach and accessibility programmes,” write the authors. There is a need, they add, for public health messaging that “accurately conveys the risk of severe illness from COVID-19 versus the risks of not seeking health-care advice.”
In the second study, Amit Sud and colleagues, from the Institute of Cancer Research, London, looked across 20 common tumour types diagnosed by the two-week referral pathway, which ended up being delayed due to COVID-19, and estimated the effects of lockdown 10 years on. The authors modeled only patients who would have had a two-week wait referral, omitting those diagnosed via other routes. Data on tumour types were derived from Public Health England and data on cancer diagnoses that resulted from referrals to the two-week referral pathways from the NHS Digital’s Cancer Waiting Times system.
The results show:
- A backlog of referrals of 25% (with an average presentational delay of two months per patient) would result in 181 additional lives lost and 3,316 total years of life lost.
- A backlog of referrals of 50% would result in 361 additional lives lost and 6,632 total years of life lost.
- A back log of referrals of 75% would result in 542 additional lives lost and 9,948 total years of life lost.
“Our estimates suggest that, for many cancers, delays to treatment of 2‒6 months will lead to a substantial proportion of patients with early-stage tumours progressing from having curable to incurable disease,” write the authors, who stress that they believe their estimates to be broadly applicable across most economically developed countries.
“Furthermore, pre-emptive public education is required to discourage patients from deferring presentation of cancer symptoms along with modification of pathways to and through primary care,” they add.
In a comment published to accompany the two studies, William Hamilton, from the University of Exeter, highlights that two markedly different figures were calculated, reflecting the different methods, cancer sites and assumptions made in the two modeling studies. “Perhaps a precise figure is not needed – the loss of life is big, whatever the method used. What is most important is the recovery plan,” writes Hamilton. There have been encouraging reports, he adds, that the UK Nightingale hospitals (which were rapidly built to offer care for patients with COVID-19) will be reconfigured into cancer diagnostic hubs. Aggarwal agrees that organisational change is needed. “We need to rapidly increase diagnostic capacity. As well as changes in working patterns, this may necessitate centralisation of booking systems to ensure all available diagnostic capacity in the public and private sectors,” he says.
Speaking to Cancer World, Matti Aapro, President of the European Cancer Organisation ECCO, comments that there is no reason to suppose that the cancer diagnosis situation modeled in the English studies would be any different for other European countries. “My personal opinion is that countries across Europe made a terrible mistake in communication, which was received as a terrorising message to patients against seeking medical advice for symptoms.” Additionally, he adds, there was no rationale behind suspending screening services, since the radiologists who review cancer diagnostic images are often entirely different personnel from those who review chest X-rays for COVID-19. “In any second wave of COVID-19 we need to ensure that the lessons around cancer diagnosis highlighted by these articles are learnt, to prevent further loss of life from cancer and other diseases, like myocardial infarctions,” he says.
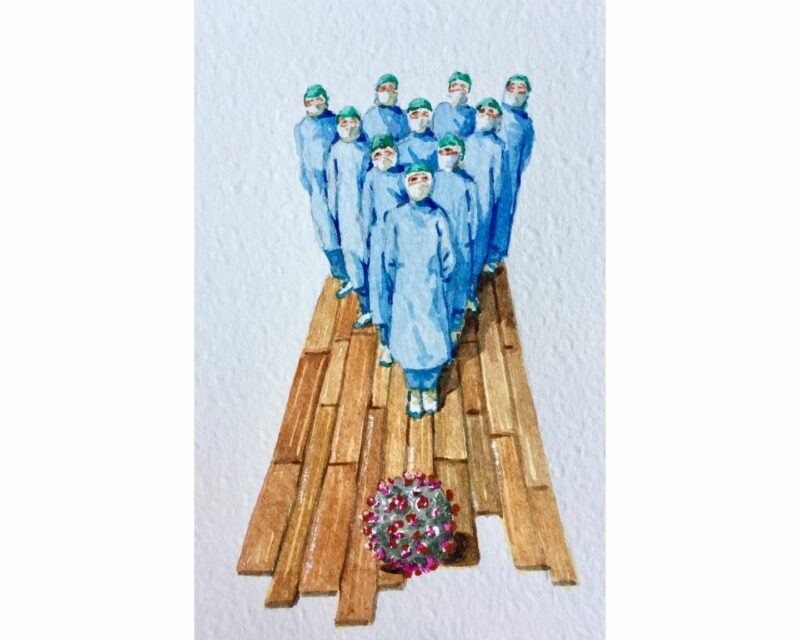
Image credits: Vanni Cuoghi, 2020, Senza titolo e in silenzio, cm 15×10 acquerelli su carta