The extraordinary career of Virgil Craig Jordan, Dallas/Fort Worth Living Legend Chair of Cancer Research, one of the ‘Four for the Millennium’ in women’s health, Order of the British Empire, Companion of the Most Distinguished Order of St. Michael and St. George, and so very much more, has come to an end.
He will be remembered above all for his discovery of Selective Oestrogen Receptor Modulators (SERMs), and especially his translational research on tamoxifen – a failed contraceptive that he repurposed into the first targeted precision cancer medicine. It was Jordan’s dogged and relentlessly thorough pharmacological exploration of the drug that revealed its potential to transform the prospects of women with breast cancer. That research laid the groundwork for him to discover similar compounds that could target more than one oestrogen-related condition, whether in a preventive or treatment setting, paving the way for generations of anti-oestrogen drugs in women’s health, and stimulating the discovery and application of Selective Nuclear Receptor Modulators.
Jordan himself always considered his tamoxifen success as only one part in a much wider and more complex story that revealed how a single compound can act differently on oestrogen receptors depending on the tissue type – acting as agonists in some and antagonists in others.
In 1977, Jordan discovered tamoxifen’s most potent metabolite with its strategic hydroxyl, which led to the development of the hydroxyl-containing SERMs, raloxifene and bazedoxifene, both approved for prevention of osteoporosis in postmenopausal women, with the latter also addressing vasomotor symptoms associated with menopause. Ten years later, Jordan showed that tamoxifen and keoxifene (later renamed raloxifene) maintained bone density in ovariectomised rats and prevented mammary cancer.
His research was rejected by osteoporosis journals on the grounds that “anti-estrogens cannot build bone, only estrogens can”. In 1990, he wrote that, “important clues have been garnered about the effects of tamoxifen on bones and lipids so it is possible that derivatives could find applications to retard osteoporosis or atherosclerosis”. This was Jordan’s clarion declaration of SERMs.
In 1992, Jordan’s data led to the clinical trial that confirmed tamoxifen prevents decreases in bone density. In 1999, raloxifene was proven to maintain bone density and reduce breast cancer incidence in postmenopausal women.
Today, there are five SERMs (tamoxifen, raloxifene, toremifene, basedoxifene, ospemiphene) approved by the US regulators, the FDA, to treat major diseases and conditions in women. From the treatment of all stages of breast cancer, to breast cancer risk reduction in high-risk women, osteoporosis, painful intercourse, and menopausal symptoms.
Today, there are five SERMs approved to treat major diseases and conditions in women
The later part of Jordan’s career was spent on discovering the molecular pathways underpinning oestrogen-induced apoptosis – that oestrogen can not only fuel breast cancer growth, but also kill vulnerable breast cancer cells under the right conditions, in women who failed multiple therapies and have no other options. This simultaneously solved a 70-year mystery, and birthed a new group of medicines called ‘oestrogen mimics’, which trigger rapid ERα[oestrogen receptor α]-induced unfolded protein response and apoptosis. He continued working on this until his final months.
He died at his home in Houston Texas, on the morning of Sunday June 9th, having survived for a remarkable seven years living with a stage 4 kidney cancer.He leaves behind as his legacy not just his huge contributions to our understanding of women’s health and cancer treatment, but also many generations of expert researchers who he mentored, encouraged, and helped on their way.
Revolutionising women’s health
It is hard to overstate the massive impact of the introduction of tamoxifen into strategies for treating early breast cancer. In terms of survival benefit – always the key outcome for Jordan – a 1998 overview analysis of 55 trials covering more than 37,000 women, with around 10 years follow-up, showed that adjuvant tamoxifen given for five years resulted in a 47% reduction in recurrence and 26% reduction in death rates.
That sort of impact is rarely seen. To achieve it, Jordan had had to believe in what his research was telling him, which frequently meant challenging widely held assumptions.
Tested first in metastatic disease, tamoxifen performed so poorly that its manufacturers, ICI, saw no point in trying to bring it to market. Jordan’s work on animal models was telling him, however, that this drug had potential. So he kept faith with the drug and looked for a setting and a strategy where it would perform better.
By the late 70s to mid-80s when much of this work was done, bitter experience had taught the medical oncology community to expect that sooner or later cancers develop resistance to every systemic therapy. Jordan’s research, however, was telling him that longer was better, and it was only when the duration of adjuvant therapy was extended to five years that the real benefits began to show (later shown to be even greater when taken for 10 years).
At that time, a dominant strategy adopted to overcome that resistance was to try cytotoxics in combination and at high doses, resulting in increasingly brutal levels of toxicity. Many in the cancer community felt that the very benign toxicity profile of tamoxifen called into question its efficacy at killing cancer cells.
Jordan’s approach to investigating the interaction between drug and disease – he called this ‘a conversation with nature’ – was meticulous and thorough. In contrast to the way drug development tends to happen today, where experimental compounds get trialled across a range of indications to find the most likely setting to gain approval, Jordan believed in doing deep immersion pharmacological exploration to understand ‘the good, the bad and the ugly’ of what the drug is doing (the ‘ugly’ in the case of tamoxifen, being an associated small rise in the risk of endometrial cancer in postmenopausal women, which Jordan flagged up before this showed up on any pharmacovigilance radars).
In someone else’s hands, the chances are that tamoxifen would never have been given the opportunity to show what it could do, and it would have ended up in the failed drug dustbin. In someone else’s hands, the risk of endometrial cancer would almost certainly not have been spotted so early, monitoring would not have been initiated, and lives might have been lost.
Jordan’s approach to investigating the interaction between drug and disease – ‘a conversation with nature’ – was meticulous
As it was, Jordan not only helped overturn many of the assumptions driving medical oncology at that time, but he also introduced the first targeted drug into cancer therapy, leading to the first use of biomarkers and precision approaches to cancer medicine, for which he doesn’t always get the credit he deserves.
With the crude and time-consuming tools available in the mid 1970s, Jordan was able to demonstrate that tamoxifen works by blocking oestradiol from binding to human oestrogen receptors. This enabled him to predict, and then demonstrate, that the drug would not work well in patients whose tumours showed low levels of oestrogen receptors. Testing breast tumours for their hormonal status became routine by the early 1990s. So by the time trastuzumab, the pioneering ‘designer drug’ came on the market in 1998, the concept of precision medicine had already been in use in breast cancer for many years.
While much of the pharmacology work investigating tamoxifen could clearly have been made easier had he had access to the techniques in use today, Jordan worried that access to these powerful tools might be dragging research into unproductive areas. In an interview with Cancerworld in 2020 on How to make precision drugs that work better, he said, “Everybody could just go into the lab and take tumours and sequence them and compare them with the normal human genome. All we’ve really done is developed a map of the world. All of these maps. But nobody has a got a clue about: What is going on in Africa? Why is Detroit different from Los Angeles? What’s going on in Europe, and what are the interactions that create a European Union? Nobody has any idea because the task is so vast. You’re not going to cure cancer by sequencing everything.”
Although targeted therapies go to a specific gene target, he said, there are no tests to put the gene target and response to the therapy together. “Nobody is doing that. It is ‘suck it and see’ with every one of them. We’ve gone back to the days before the oestrogen receptor and SERMs.”
A sense of duty and public service
Jordan once reflected that nothing in his early upbringing – in a town in northwest England, twenty minutes’ drive from the headquarters ICI’s pharmaceutical operations – could have predicted any path to progress in breast cancer research, describing his indifference to schoolwork, with his great interest being “Roman history, a passion for chemistry, training, organizing, leading and teaching other children in the neighbourhood”.
Those who knew him, worked alongside him, and particularly those who worked under him, can testify that, in reality, all of those attributes contributed to the success of his research career – except possibly the Roman history, though that will have fed into a parallel career he chose working within the British (and occasionally US) military. As for the indifference to schoolwork, as Jordan himself recognised, that too might not be such a bad predictor for a truly successful career in science, where the sort of intellectual agility and imaginative leaps that are not always fostered in a school environment, can be crucial for spotting clues to what your research data is showing you.
Jordan’s driving force was a strong sense of duty and service, which he attributes in part to a strong military history within his family, but equally to a sense of debt he has always felt to the people who took a chance on him. He talked, for instance, of a formative experience of his mother battling the school authorities to allow him to stay on past age 16 to take his ‘A’ levels, after he flunked out with only three ‘O’ levels to his name – a minimum of five were required to carry on. The resolve that paid off in his later pharmacology work was created, he believed, by his early failure, and his mother’s “unshakeable support”.
He talked too about his debt to his chemistry teacher, who not only supported his bid to continue his schooling, but convinced him to try for university, and wrote a personal letter of recommendation that backed Jordan as “a VERY interesting young man”. Jordan would never forget the opportunity his teacher offered him, which opened a door to everything he would later achieve. Throughout his career he developed a track record of going above and beyond to help open doors for others.
The story of how that initial pharmacology degree from Leeds University (1969) led on to a PhD on the oestrogenic and antioestrogenic activities of some substituted triphenylethylenes and triphenylethanes (1973) and to working with key players including Arthur Walpole, Mike Harper, Dora Richardson, Roy Cotton, and Lois Trench to explore the possibilities of tamoxifen as an anti-cancer agent is told by Jordan in his 2014 article Tamoxifen as the First Targeted Long-Term Adjuvant Therapy for Breast Cancer.
That research work took him to labs at Worcester Foundation for Experimental Biology, in Shrewsbury, Massachusetts – his first visit to the USA, which was to become his home for almost his entire career.
The story of Jordan’s subsequent search for “the ‘ideal’ SERM, which would have estrogenic effects on bone and serum lipids, neutral effects on the uterus, and antiestrogenic effects on breast tissue,” is told in a 2013 article he co-authored on The Discovery and Development of Selective Estrogen Receptor Modulators for Clinical Practice.
The research he was focused on near the end of his life, looking at the wider therapeutic implications of the apoptotic effect of giving a “whiff” of oestrogen to a breast cancer that had been treated with hormone deprivation for many years, remains unfished business. In 2019 he talked about the concept that there may be a general principle that “there is a program in all human cancer in which normal cells contain the ability to activate cancer-killing properties. Therefore we need to understand this activity which will open up a huge new area of research, finding ways to unlock the cancer-killing properties of any cell in the body.”
Particularly for people he felt were underestimated, he’d say, ‘I’ll give you opportunities to improve yourself and help you fly
Balkees Abderrahman, who did her PhD on this topic (2017–2020) as a Dallas/Fort Worth Living Legend Scholar, under Jordan, had been working with him on this ‘big project’ ever since, which included pulling everything together in the last year of his life to ensure that work can continue.
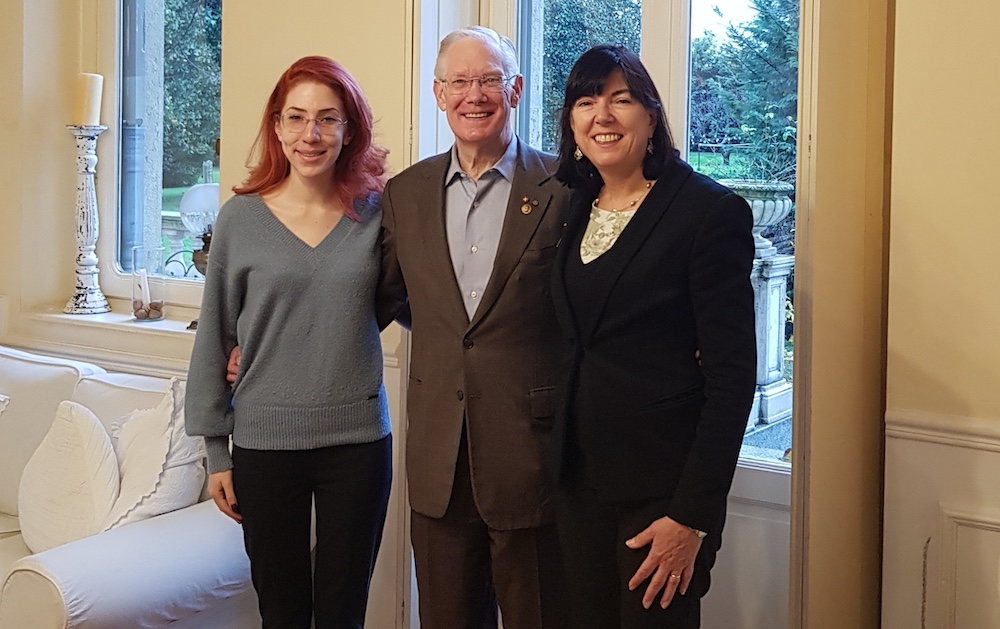
She speaks very warmly of the support Jordan gave her and all those that worked under him. She remembers him as a person whose generosity and kindness marked him out from other faculty members. “He was really interested in the lives of others, he always showed up and gave us opportunities. Particularly for people he felt were underestimated, he’d say ‘I’ll give you opportunities to improve yourself and help you fly.’”
They in turn carried out much of the work that drove forward Jordan’s research projects, which he made a point of frequently acknowledging, including for instance in his 2021 article Turning scientific serendipity into discoveries in breast cancer research and treatment: a tale of PhD students and a 50-year roaming tamoxifen team.
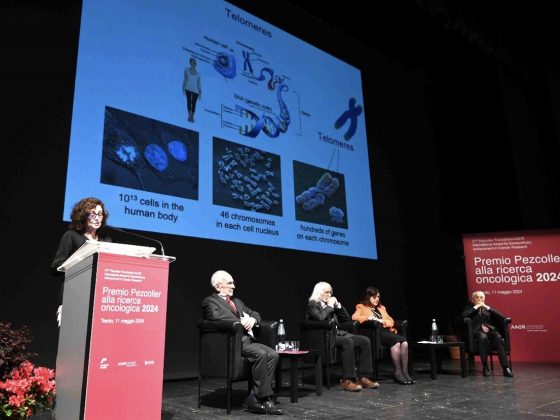
The philosophical approach that underpinned Jordan’s work, of understanding causes and intervening with minimally toxic ways to prevent disease is one that presented a desperately needed alternative to the direction that cancer treatment was going in the 1970s and ’80s. It spoke to the agenda of leaders in the breast cancer field such as Umberto Veronesi, a pioneer in breast conserving surgery, and was strongly reflected in the approach taken by the European School of Oncology (ESO), which Veronesi set up in 1983.
Alberto Costa, who was a surgeon under Veronesi, helped found ESO and remains its CEO, has valued Jordan as a friend and researcher for many decades, and found him his customary kind, gentle and quietly humourous self, when they met at Jordan’s Houston home shortly before his death.
“Craig Jordan has been my ‘older brother’ for more than 30 years in our common field of breast cancer research. We met the first time when he was in Madison, Wisconsin and since then we have always been in contact to coordinate our studies, particularly in the area of prevention, when we conducted the Milan trial with tamoxifen in women who had undergone hysterectomy.
“Craig was also a great lecturer at our European School of Oncology and his presence in our Venice courses was always a party. I was lucky enough to visit him less than a month ago, where we had a final big hug, and with his eternal British humour he told me: ‘I hope not to see you soon, my dear Alberto!’”
The sheer weight of contributions Jordan made to our understanding of breast cancer and its treatment is reflected in a CV that covers 86 pages and lists more than 800 books, peer reviewed papers, chapters and reviews. It also lists a glittering array of awards and recognitions, including Honorary Fellowship of the Royal Society of Medicine; American Society of Clinical Oncology David A. Karnofsky Award; the British Pharmacological Society’s Sir Henry Wellcome Gold Medal; Identified by the National Cancer Institute as one of the pioneers of cancer care and prevention to celebrate the 50th anniversary of the National Cancer Act in 1971; Identified by the German Society of Gynaecology and Obstetrics as one of the “Big 4 of the Millennium” for women’s health; Elected to the Giants of Cancer Care Oncolive…
This professional recognition was very important to Jordan. But the awards that he valued, perhaps, above all others, were the ones bestowed by the British monarchy, in the form of an OBE (Order of the British Empire) for services to international breast cancer research, and in 2019 a CMG (appointed Companion of the Most Distinguished Order of St. Michael and St. George) for services to women’s health.
It was that belief in service to others and the nation that his family had bestowed on him as a boy, which had remained the driving force throughout his successful career, even though that career was played out almost entirely in the US.
It is fair to say that he repaid the debt he owed those who showed faith in his potential as he made his shaky start. Few people in our time have served the cause of women’s health so well.
Craing Jordan documented his adventures in his autobiography and self-help book, Tamoxifen Tales: Suggestions For Scientific Survival.