“My partner had to be admitted to hospital with neutropenia earlier on in her treatment cycle, and she and I are constantly discussing what to do: whether we should ask about suspending treatment, how the risk/benefit equation adds up, whether we should call the consultant. But I think the fact is no one, not even COVID-19 experts, have the knowledge on which to base decisions. It’s an evolving virus and an evolving pandemic: no one knows what to do.”
These words were written in a chemotherapy clinic in England in early March 2020, around the time that new cases and deaths from the novel coronavirus were beginning to escalate in Italy, and the governments of Europe were sending out urgent public health warnings and preparing their citizens for lockdown (Cancer World, Voices, published online 18 March 2020).
Over the following months, cancer services, and health services in general, would drastically change the way they operated, in line with the ‘first do no harm’ principle. Standard pathways and protocols were reviewed to ensure the benefit patients could expect was not outweighed by the added risk of being exposed to the virus and/or making them more vulnerable to infection or more likely to die if they caught it.
There were many reasons for concern. Cytotoxic drugs, some supportive drugs (such as steroids), and having cancer in itself are all known to impact the immune system, making people more vulnerable to catching an infection and limiting their ability to fight it off once caught. By contrast, immunotherapies are designed to boost the immune response, which led to fears of inducing cytokine storms in people exposed to the COVID-19 virus. Surgery is also known to repress the immune system for weeks or even months following an operation. The prevalence of comorbidities and older age that are common in cancer patients compound these risks further, leading to serious, potentially life-threatening symptoms from COVID.
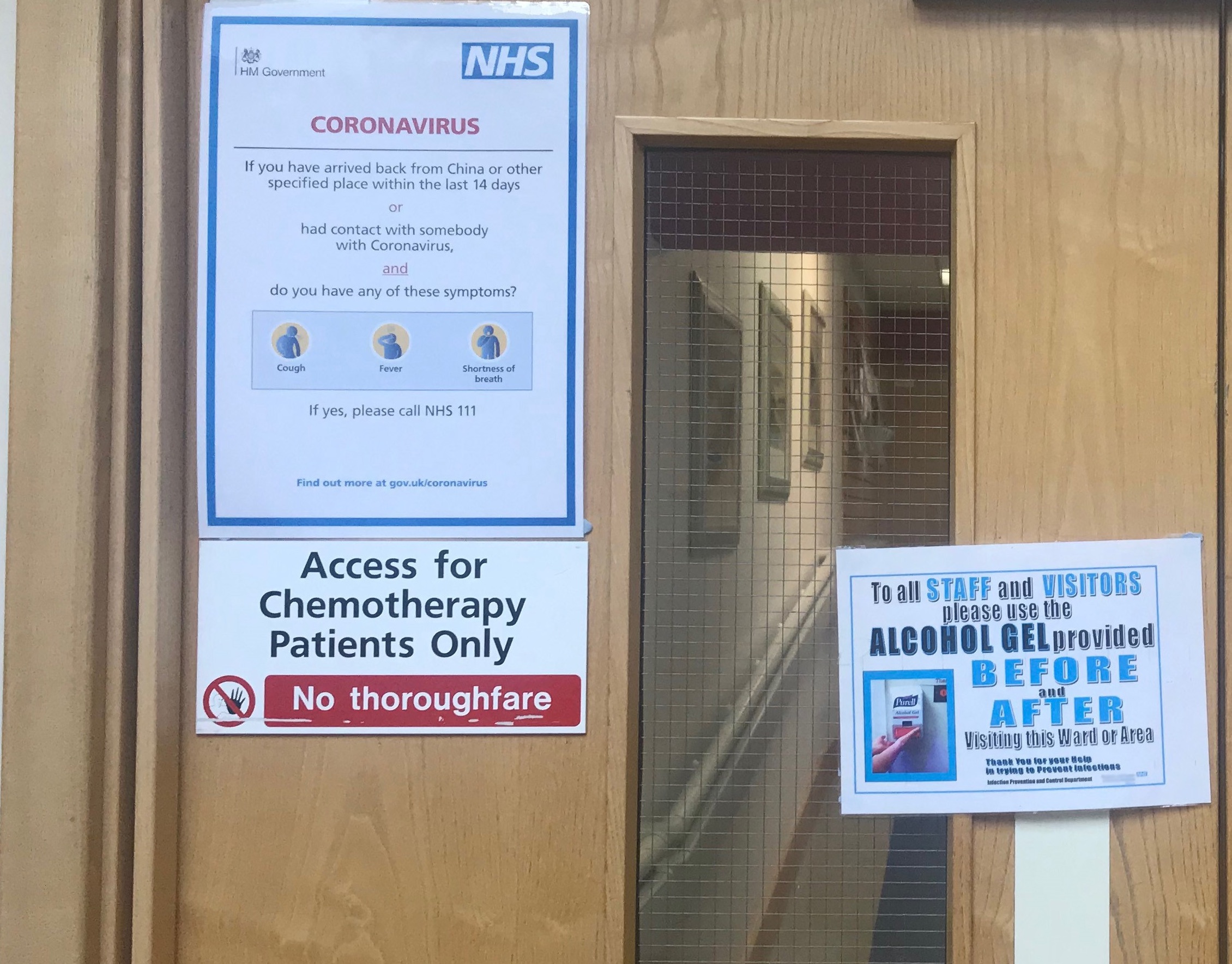
In these circumstances, taking a very critical look at the risks versus benefits of inviting patients out of the safety of their homes to visit medical facilities, and administering treatments that could raise their risk from COVID, was clearly the right thing to do. All the more so, where those same medical facilities were also treating patients with COVID, and at a time when no reliable COVID testing was available and many hospitals were struggling to get basic protective supplies, such as hand sanitizer and personal protective equipment (PPE), needed to keep themselves and their patients safe.
Risks and benefits ‒ the clinicians’ perspective
The only published evidence available at that time came from China. A case series report from the Chinese Center for Disease Control and Prevention showed a case fatality rate from COVID of 5.6% among cancer patients compared with 2.3% for the general population. A prospective study from the Chinese National Clinical Research Center for Respiratory Disease reported on a cohort of 1,590 patients with COVID, which included 18 people who had cancer or had recently been treated for cancer, of various types, at various stages and with various treatment modalities. The data indicated that people with cancer were much more likely to die or need invasive ventilation than people without cancer, even after accounting for age, smoking history and other comorbidities. Among cancer patients, those who had received chemotherapy or surgery in the past month were more likely to experience clinically severe events than those who had not been treated in that timeframe.
It would be several months before data from much larger studies became available, which started to tease apart which cancer patients were most at risk from severe events or death (Kuderer NM et al. Lancet 2020), and importantly questioned the finding that cancer treatment per se ‒ using any modality ‒ increased the risk of severe events or death from COVID (Lee LYW et al. Lancet 2020). Meanwhile, oncologists had to act on the evidence available, which in hindsight may have led to undue caution, as was recognised in the consensus paper on ‘Managing cancer patients during the COVID-19 pandemic’, published by the European Society for Medical Oncology in July 2020.
The general policy widely advocated early on was to continue treating patients already in treatment, but to consider adjusting the standard treatment to protocols that were deemed safer in terms of the risk from COVID. This included moving to longer treatment intervals for chemotherapy, shifting from hospital-administered infusions to oral treatments that could be taken at home, avoiding immunotherapies, abbreviating radiotherapy courses, or giving fewer but higher doses, cancelling follow-up visits or conducting them remotely, and possibly delaying the start of adjuvant treatment.
When it came to new patients, the question was whether to wait until the ‘first wave’ of COVID was over before starting treatment. In a lot of cases, that is exactly what happened. Considerations of the best interests of the patient were not the only driver here, but they were important. While immediate treatment is imperative with certain cancers, there are others where a few weeks’ delay poses little additional risk, and given the evidence from China it made sense to weigh the relative risks carefully for each patient.
The lack of detail in that evidence, however, made the balancing exercise harder. Was chemotherapy the biggest threat? Should neoadjuvant treatment be omitted in favour of wider surgical excision? Or was surgery the biggest threat? Should patients be kept on neoadjuvant treatment for longer than normal to keep the cancer under control until the COVID spike had passed, when surgery could be performed more safely? How much does each week of delay impact on the effectiveness of surgery or of adjuvant therapies, and in whom?
Oncologists are used to working with unknowns, but this was truly unprecedented territory – a once-in-a-generation challenge – where every evidence-based guideline that could be trusted as the gold standard before COVID could no longer be assumed to apply.
The global cancer community was quick to collaborate on national and international registries to start developing the much-needed evidence as fast as possible. But it wasn’t until May 2020 that the first publications began to come out. In the meantime, oncologists had to look for guidance that started coming out of leading cancer services, cancer centres and professional organisations, based on the limited available evidence together with basic principles and common sense ‒ and usually accompanied by the caveat “these are not guidelines” (Ferrario C. CancerWorld 2020).
Risks and benefits – the patients’ perspective
In some cases the decision to interrupt treatment was initiated by patients. Powerful messaging from governments about the dangers of COVID aimed to maximise population-wide compliance with the lockdown, rather than to equip cancer patients with the information they needed to weigh up the risks of catching COVID against the risks of interrupting their care. Messaging from oncologists and patient advocacy groups stressed the higher risk COVID posed for cancer patients and the importance of ‘shielding’ ‒ staying away from all possible sources of infection. And they could not count on hospitals to be safe.
While cancer centres were generally safer than oncology units within general hospitals, reaching them often involved longer journeys, which was either risky or sometimes impossible by public transport. Stories about COVID outbreaks in hospital units treating non-COVID patients hit the headlines, and fuelled public fears that medical facilities were risky places.
One melanoma patient advocate in France described the feeling in the patient community: “When they hear that there is no PPE or triage, that healthcare professionals are overstretched, and they are more vulnerable, say, to cytokine storm, they then have to decide whether being constantly worried about progression not being picked up is really worse than risking COVID…Some go in looking like Buzz Aldrin, and others stay at home and cancel.”
Cancer patient advocacy groups reported receiving double the average number of calls compared to pre-COVID days, with more than four out of five of the queries relating to COVID concerns. Not surprisingly, almost nine out of ten respondents to a survey of affiliates conducted by five global cancer advocacy coalitions reported worrying levels of stress and anxiety among patient communities, with many reporting a significant impact on attending medical appointments.
Capacity and priority
Other pressures were at work, which arguably had as great an impact on the delivery of cancer care. Chief among them was health service capacity. Available data on the per capita number of beds and intensive care beds, for instance, indicate massive disparities across Europe. Germany has up to three and a half times as many hospital beds per capita as countries such as Portugal, Italy, Spain, the UK and Sweden. Its per capita intensive care bed capacity is between two and and three times that available in Italy and Spain, around four or five times that available in the UK and Sweden, and almost seven times that available in Portugal.
Many health services struggled too with their staffing levels, in some cases redeploying medical and non-medical staff from oncology and other units, which were already suffering from high levels of absence due to COVID infection or ‘self-isolation’. All over Europe, elective surgeries were delayed or cancelled, as all available capacity was prioritised for COVID patients.
Collateral damage: cancellations, delays and changed protocols
Cancer diagnosis
The disastrous drop in diagnosis and referrals of new cancer cases across Europe will no doubt prove to be where the pandemic wrought the greatest collateral damage. Interruptions in screening programmes, delays in diagnostic referrals, and public reluctance to contact medical services about worrying symptoms were all contributing factors. One modelling study estimated that, in the UK alone, around 3,500 people in the UK will die from breast, colorectal, lung and oesophageal cancers who could have been cured if diagnostic routes had been working as normal, amounting to around 60,000 years of life lost. Such reports have led to calls for a change in policy to ensure all diagnostic referrals ‒ not just those where cancer is strongly suspected ‒ continue as a priority during this and any future pandemics, and for clear public messaging about the importance of moving quickly to get checked out if they have symptoms that they are concerned about.
Cancer care
The impact on patterns of treatment and care has been harder to quantify. To try to get a snapshot of what was happening at hospitals and cancer centres across Europe, Cancer World conducted a survey of oncologists in early June 2020, on Cancer Care During the Pandemic: Problems and Solutions. The survey asked questions regarding concerns about delays in diagnostics and treatment, changes to standard practice, approaches to clinical decision making, communication with patients and colleagues, and safety issues. Some respondents were contacted again in mid-August 2020 to get more detail, or updates, on their comments to the original survey.
Responses to the survey indicate that, in most European countries, changes to normal pathways and protocols happened in around four out of ten patients. The reported proportions increased to around six in ten in some countries, including Belgium and the UK, but were lower in others, including Switzerland and Germany. Changes to the normal course were reported to be slightly more frequent in general hospitals than cancer centres. This finding concords with a comment made in response to the survey by a practitioner at a leading southern European cancer centre, indicating that the realities at that cancer centre were very different to those at the majority of hospitals treating cancer patients elsewhere in the country. In France, a melanoma patient advocate reported that, while the Institut Gustave Roussy cancer centre seemed to be operating “relatively normally”, in other places significant changes to care were happening, with patients being switched from immunotherapy to targeted treatments and transfers to clinical trial centres being put on hold.
The Cancer World survey was circulated just around the time that some of the stronger evidence was emerging that suggested sticking to standard protocols for medical treatments was safe in many patients, and the survey would not have reflected that new information. However ‒ with some notable exceptions ‒ responses did indicate confidence (7 on a scale of 1‒10) that, in the changed pandemic environment, most oncology teams were making an effort to tailor treatment and care plans to each patient’s individual risks, benefits and preferences, and that the implications of any changes or delays to standard treatments were generally discussed with patients (7 on a scale of 1‒10). Confidence levels about whether treatment recommendations were made following multidisciplinary team (MDT) discussions were lower (just over 5.5 on a scale of 1‒10).
Guidelines
Of the 30 European countries represented by respondents to the Cancer World survey, the great majority said they had some form of national guidelines as well as hospital guidelines. Countries with strong professional oncology organisations were able to rapidly translate emerging evidence into recommendations and best-practice guidance. Where that lead was lacking, however, the guidelines seemed to be driven more by protecting against the risk of COVID than ensuring cancer patients got the treatment they need. An oncologist in Bulgaria commented that, in the early stages, “There were many national recommendations [that were] contradictory and changing from day to day… The instructions were to minimise the risk of a COVID patient entering any hospital system.” In practice this meant that any patients with fever were immediately referred to COVID units, “regardless of their other diseases or need of treatment.”
“During the COVID era, the first problem to be excluded is a viral infection. This introduces a delay, a need for a second consultation, stress and at least two visits to the hospital of patients who are frequently in a poor condition.”
With time, and as more evidence and guidance emerged at an international level, the oncologist adds, “we learned how to manage these patients and to minimise the stress both for them and for us.” But given the weakness of the national oncology lead, many oncologists in Bulgaria are reportedly still reluctant to treat patients for fear of the COVID risk. “This has led to a transfer of many patients to colleagues who ‘take the risk’ to treat the cancer disease from other colleagues who ‘prefer to stay on the safe side’.”
Even in countries with strong professional oncology guidelines, differences in implementation by region or from hospital to hospital have been reported. In the UK, for instance, where the NHS and the National Institute for Health and Care Excellence (NICE) were quick to develop and publish national guidelines during the pandemic, such as on the delivery of systemic anti-cancer treatments, variations in practice have been reported. In their response to the survey of affiliates conducted by five global cancer advocacy coalitions a UK group commented that, in “some parts of the UK”, women with ovarian cancer had had “significant non-evidence based changes to the treatment pathways, e.g. no chemotherapy for women with platinum-resistant disease, lack of access to counselling services and palliative care.” Such reported variations may reflect local differences in COVID prevalence and/or health service capacity, or simply the difficulties of responding at speed to a rapidly changing evidence base.
Cancer surgery
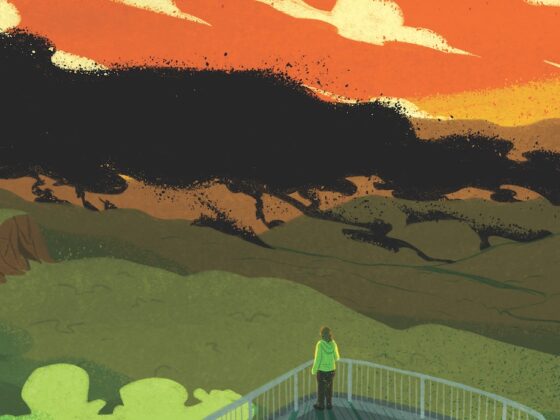
A predictive modelling study conducted by the COVIDsurg collaborative, and based on expert assessments, estimated the cancellation rate for cancer surgery during the 12-weeks of peak disruption would range from almost one in four to more than three in four across the globe, with most of Europe being at the lower end of the range. The authors called on governments to “mitigate against this major burden on patients by developing recovery plans and implementing strategies to restore surgical activity safely.”
Expert assessment of surgeries cancelled or postponed during the 12-week peak disruption
Based on the Bayesian β-regression model, best estimates for country-level cancellation/postponement rates for cancer surgery, during the 12-week peak disruption ranged from 71.2% to 87.4% across 71 countries. Figures for European countries were at the lower end of the range.
Source: COVIDSurg Collective (2020) Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg 107:1440-1449 © 2020 BJS Society Ltd Published by John Wiley & Sons Ltd. Republished with permission
Responses to theCancer World survey indicated that concerns over delays and cancellations were higher with respect to surgery than any other elements in the cancer pathway, except for diagnostics. Many respondents highlighted their concerns over potentially curable cancers moving to higher stages and becoming inoperable. They also queried the evidence basis for the delays, “There is not clear evidence that delays may protect patients from COVID but it is likely that they may affect the outcome.”
Among survey respondents, German oncologists were the only ones to report no disruption to cancer surgery. (By contrast, “practically no scheduled follow-up of cancer patients after completion of their treatment was performed,” commented one surgeon from Berlin, who voiced fears of “significant delays in the diagnosis of metastasis/recurrence”.)
A UK study published in mid-May, based on age-specific and stage-specific cancer survival for England between 2013 and 2017, calculated that delaying cancer surgery by three or six months would result in the attributable deaths of, respectively, 4,755 or 10,760 people who would otherwise have achieved long-term survival. The message from the authors was, “to avoid a downstream public health crisis of avoidable cancer deaths, cancer diagnostic and surgical pathways must be maintained at normal throughout, with rapid attention to any back log already accrued.”
Medical treatments
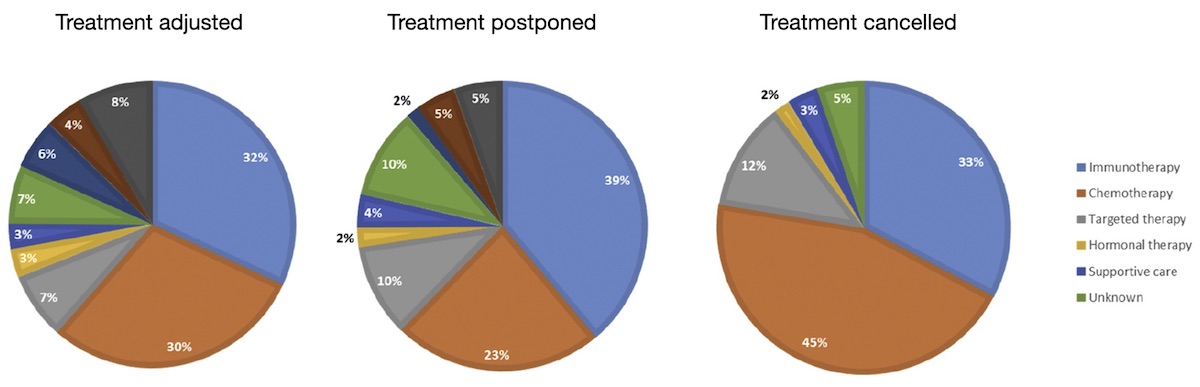
Some indication of the extent and nature of changes to medical oncology treatments is offered by a survey of patients in the Netherlands, conducted by the Dutch Federation of Cancer Patients Organisations, over three weeks beginning 28 March 2020. Among the 2,664 respondents who had had contact with the hospital, one in five indicated their treatment had been changed (i.e. adjusted, delayed or discontinued). In patients with adjusted treatment, chemotherapy (30%) and immunotherapy (32%) were most frequently adjusted. Delay and discontinuation of treatment also mainly included chemotherapy and immunotherapy (see Figure).
Changes to standard treatments during the pandemic, by modality
In an online survey conducted in the Netherlands in April 2020, one in five patients indicated their treatment had been adjusted, postponed or cancelled. The pie charts show how the changes to standard treatments break down by modality.
Source: K. de Joode et al. (2020) Impact of the coronavirus disease 2019 pandemic on cancer treatment: the patients’ perspective. Eur J Cancer 136: 132‒139 © Elsevier 2020. Reprinted under a Creative Commons Licence
Radiotherapy
Of all the treatment modalities, radiotherapy was associated with the least concerns about the risks of exacerbating the course of COVID ‒ except where irradiation of the lungs was concerned. Nonetheless, the impact on the risk‒benefit balance of going ahead with treatment as normal had to be revised to take into account the risk of exposing patients to the virus by requiring them to travel to the treatment centre, and to be treated by staff and equipment potentially exposed to the virus. Restrictions in capacity were also a problem due to the time taken to clean the facilities between patients, the time taken for additional protective measures, and the need to minimise the number of staff in the unit at any one time.
Reassuringly, a fair level of evidence was already available on the impact of treatment interruptions and how best to manage them, as well as the relative effectiveness of delivering lower doses more frequently compared with higher doses spread across fewer treatment sessions ‒ ‘hypofractionation’ ‒ which seems to have been used widely across Europe during the pandemic.
Consultations and follow-up
Postponing or cancelling visits to hospitals that did not involve delivering treatments was one of the first and most widely implemented measures taken by European health systems. Many of these planned visits were replaced by remote consultations over the phone or internet. What was lost, in many cases, were opportunities for follow-up tests and imaging that could have given early signals of a recurrence or metastatic spread, or for monitoring toxicities that could avoid problems building up to a point where patients have to be taken off therapies they wished to continue.
The impact that will have in lost lives and lost life-years could ‒ and arguably should ‒ be modelled in the same way that has been done with delayed diagnosis of primaries.
Yet the shift towards greater use of telephone and internet consultations was not always a bad thing in the eyes of both practitioners and patients. Discussions about the pros and cons of greater use of digital communications between doctors and patients have been going on for more than a decade. The pandemic has acted as a catalyst that propelled a major shift towards remote forms of communication almost overnight.
Responses to the Cancer World survey indicate that more than four in ten practitioners are conducting ‘a few more’ patient consultations over the internet or by phone, with a slightly larger number reporting ‘a lot more’. Only just over one in ten said their mode of communications with patients had not changed. Surgical oncologists and oncology nurses were slightly less likely to report increased communication by phone or internet, but the trend was clear for all oncology professionals and almost all countries.
This communication change is likely to be one of the lasting legacies of the impact of the pandemic on oncology practice. While remote conversations work better for some patients than others, and are entirely inappropriate and unhelpful for some communications and discussions, they do seem to have worked well for both patients and medical professionals in many instances.
What worked well? What can we do better?
The spring and summer of 2020 put immense demands on oncology professionals, requiring them to be creative, collaborative and use all their medical knowledge and skills to do their best for their patients, with limited evidence, stretched capacity and in a climate of fear. The cancer community can be proud of the speed at which it responded to the challenge of generating evidence, through registries and research collaborations such as the COVID-19 Cancer Consortium Registry, the Thoracic Cancers International COVID-19 Collaboration (TERAVOLT), the UK Coronavirus Monitoring Project, COVIDSurg and many others. The evidence provided has been key in giving confidence to practitioners and patients alike to minimise the huge disruption to cancer care that was seen in the early period of the pandemic. It also provides vital ammunition for giving much greater priority to ensure timely diagnosis, care and follow-up of cancer patients and rapidly clearing the backlog.
But the pandemic is far from over; health services remain highly stretched, cancer patients remain in need of ‘shielding’ ‒ some more than others; as of the end of September 2020, the pandemic seems to be resurgent across most of Europe; the possibility of a vaccine or improved treatment and care of COVID patients becoming available anytime soon remains uncertain at best. Oncologists and oncology services need to take stock of what has worked and what needs urgently to change.
Safety
Safety has to remain a big priority to protect patients from exposure to COVID and, importantly, to give patients confidence to engage with their diagnostic and care pathways. At the time of the Cancer World survey (early June 2020), more than one in four respondents said they had a COVID infection rate of between 1% and 5% in their departments, with a further one in ten reporting infection rates of between 5% and 10%.
On a rating scale of 1‒10, respondents rated their confidence in the effectiveness of COVID screening for patients and staff at around 5. Confidence in access to adequate PPE, and in the measures taken to ensure visiting cancer patients were kept away from risks of COVID exposure was marginally higher, at a little over 6. More than three in four respondents were aware of protocols about how and where to treat cancer patients who were diagnosed with COVID.
Comments from respondents indicated that, even where good policies were in place, it was not always possible to carry them out. One Italian surgeon commented. “Please apply better the strategy!” A surgeon in the UK commented, “Here in Wales COVID 19 testing for staff seems very difficult and I have been refused testing three times. Patients for surgery tested after 14 days isolation ‒ surgical teams NOT tested at all.”
The difficulties accessing PPE made headlines across Europe during the early months, with the high worldwide demands pricing poorer health systems ‒ such as in Albania ‒ out of the market. While the situation has stabilised somewhat, problems clearly remain. An update on the situation in Germany provided in late August by one of the survey respondents indicated that, “It is better now, but the quality of the protective masks for example is often very poor. In some cases, protective equipment and disinfectants have been and are being stolen, or are only available to personnel in the infection areas. Sometimes everything is sold out or simply cannot be ordered. Smaller clinics and the outpatient sector have bigger problems, also because the prices for protective equipment have skyrocketed.”
Going forward, the respondent would like to see more government support for provision of PPE, more testing of medical and nursing staff, and crucially better education of both staff and patients. “Precise information about risk management and necessary protective measures have a lasting effect on the behaviour of staff and patients. They can better understand processes and assess their own risk and implement the necessary self-protection and protection of others. Unnecessary fears and uncertainties can be avoided to ensure high-quality patient-oriented treatment.”
Delays
Ending delays that are not supported by evidence, and addressing backlogs, will need to be an urgent priority moving forward. Responses to the Cancer World survey indicated serious concerns about delays to all elements of the pathway, but most particularly about cancer surgeries and above all diagnostic and follow-up tests.
Focusing advocacy around addressing the multiple issues that led to the disastrous drop in new diagnoses and referrals, and delayed prompt access to curative treatment, makes sense in terms of the potential savings in life-years and health service expenditure.
There are concerns, however, that efforts to address the delays and backlogs in the preventive and curative setting could come at the expense of survivors, including those living with incurable cancers. Even those cancer services that made every effort to avoid delaying or interrupting cancer treatments were quick to cancel the great majority of hospital visits for follow-up checks. Concerns about delays in picking up recurrences and metastases were a frequent theme among respondents to the survey. Strong advocacy will be needed for this group of patients as well, to ensure that the delays and backlogs in follow-up visits do not continue ‒ or even worsen ‒ as systems try to redress the delays in the curative setting.
Protocols and pathways
Thanks to the prompt collaborative action in setting up cancer and COVID registries, new evidence will continue to emerge on risks and benefits of adapting standard pathways and protocols to the changing pandemic environment. Ensuring maximum participation in registries will be important. Rapidly spreading the evidence and emerging recommendations will also be essential.
Responses to the Cancer World survey indicate that one of the positive changes during the pandemic has been greater (internet-based) interactions and collaboration between cancer professionals, beyond discussions of individual cases at MDT meetings. “Webinars are very interesting to communicate with colleagues of other hospitals,” commented one respondent. Another talked about how greater communication had led to a better understanding of the different challenges faced by oncologists working in a general hospital environment compared with cancer centres. Many indicated that these sorts of interactions should continue. Making sure that happens will help ensure patients across Europe will benefit from emerging evidence as soon as possible.
As we have seen, however, evidence is not the only determinant of the care cancer patients can access. Asked to rate their confidence on whether changes to normal diagnostic treatment and care practices were being consistently implemented in the best interests of patients, the overall response was only 6 on a scale of 1‒10.
Some of the more negative comments included, “Protocols during the pandemic were focused to overcome problems, not to improve quality of care,” and “We are just ‘washing our hands’ with guidelines and making sure about ‘legal implications’, not aiming to provide the best for our patients.” Advocating against deprioritising the interests of cancer patients during the pandemic will therefore be important going forward.
That said, many respondents also highlighted changes to pathways and protocols initiated during the pandemic that they felt improved the quality and efficiency of care and should be maintained moving forward. Attitudes differed markedly between disciplines. Almost 80% of both radiation and clinical oncologists were enthusiastic about some changes. Medical oncologists, oncology nurses and palliative care specialists were more evenly split, with between 50% and 55% indicating in favour. By contrast, only 40% of surgical oncologists indicated that they would want to continue with any of the protocol and pathway changes made during the pandemic.
Hypofractionation
Notable among the responses on protocols and pathways was the enthusiasm voiced by many clinical and radiation oncologists for using hypofractionated treatment schedules, which reduce the number of visits to radiotherapy facilities while maintaining an effective overall dose. That is an issue we can expect to read more about in the coming months.
A more critical approach
Other changes for the better mentioned by respondents highlighted the benefits of being obliged to question assumptions about the value of certain standard treatments in different patients. Examples of such comments include: “A more realistic assessment of risks and benefits of adjuvant or palliative chemotherapy”; “critical thinking about diagnostic and therapeutic procedures” and “[better patient] awareness of what is really necessary for their pathways”.
Examples given of decisions that received more critical scrutiny included the following: For patients with advanced cancer undergoing palliative treatments, are imaging exams really needed or are clinical assessments sufficient to continue or change therapies? Are complete blood counts really needed in all patients undergoing chemotherapy or is it sufficient for certain patients to call in case of new health problems? Are post-therapy follow-up exams really necessary, or is a phone call or a video conference sufficient? Is it reasonable to use therapies with fewer visits ‒ e.g. once every 3‒4 weeks ‒ instead of more frequent treatment visits?
Communication with colleagues
Responses to the Cancer World survey indicate that greater use of videoconferencing and telemedicine was very widely welcomed, and we can expect to see a big change in the way communication is handled between members of MDTs and between professionals working in different parts of the system. Reported advantages include convenience, and also better discipline at preparing material in advance of discussions ‒ something also mentioned in relation to communication with patients.
Other comments highlighted faster decision making: “We need to think about keeping the pace of decision making post COVID-19,” and more-efficient record keeping, “Electronic therapeutic plans are now standard of care for most of our patients.” Enthusiasm was also expressed for greater use of virtual communications for more general educational purposes, “All these new webinars should keep going, for more subjects.”
Communication with patients
Attitudes towards greater use of remote communications were more mixed. Among those who said they had increased their use of remote communication with patients, the satisfaction rate “in terms of communications with you and your patients e.g. breaking bad news and discussing treatment options” was rated at just over 6 on a scale of 1−10. Among respondents overall, just over half indicated there were some changes to communications with patients during the pandemic that they would like to continue, going forward, with the remainder indicating they want a return to pre-pandemic ways of communicating.
Plus points were: fewer hospital visits were less disruptive for patients, ease of communication led to “more confidence between patients and doctors”, oncologists could spend less time on routine conversations giving them longer to spend on patients who needed more time. Negative points included limitations in familiarity, skills and access to the right communications equipment (for doctors and patients), and the loss of important non-verbal communication ‒ somewhat mitigated when using video links.
Almost all comments were qualified by stressing the importance of continuing with face-to-face consultations for specific conversations and specific patients.
The strongest comments, however, were about how pandemic restrictions are isolating patients in a way that is cruel and hampers effective communication.
The rule about no friends or family being allowed to accompany patients to hospital visits seems to have been implemented ‒ for understandable reasons ‒ across Europe. “This disturbs me highly on ethical grounds. Nobody should hear bad news about their health on their own,” was one comment from Belgium. Another comment, from a Danish practitioner, argued that conversations aimed at helping patients reach the right decision for them, often require the presence of family members or close friends, particularly when the news is not good. “Alone, most patients are quite vulnerable to these informations, and might not be able to catch all important details. Even more so when there are no treatments left to try, and the goal of the meeting is to plan for the few last weeks of life.”
The respondent reported that her team tried using the phone on speaker, to enable family members to be present in conversations with patients, “but all non-verbal communication is lost and one cannot really know their reaction to some of the information. Plus, when there are conflicts, either between patients and us or internally in the family, it is not possible to ease this using body language. So in all, the ‘interpretation’ of the patient; how they feel, think, behave, the challenges they face and the support they have has been very much limited by the visitor’s ban from outpatient clinics during COVID.”
Protecting the caring aspect of cancer care
In some ways the pandemic seems to be forcing oncology services, in some areas, to become more efficient, quicker, more digital, more critical, and better at allocating time where it is most needed ‒ all of which are to be welcomed. The big question posed by the Danish practitioner, however, is whether the human touch that is required to do the best for patients faced with difficult and distressing decisions can survive the current culture of social distancing.
“In my experience, the ethical standard of how we perform our work has been lowered, and my biggest fear is that this will become the new standard, as the pandemic will continue for many months and possibly years to come, and people already seem to have forgot how we did things before.
“I saw a nurse give a patient a hug yesterday. I haven’t seen that in months, but it really shocked me that I even paid attention to it, as if it was some big issue. Six months ago I myself hugged patients without blinking, if that was what they needed. Now I hardly touch them. It affects the trust and loyalty that we have in our patient‒doctor relationship. And though we try to compensate, the social distancing is as much psychological as it is physical, and I strongly believe it will lead to more conflicts and less understanding and trust in the years to come.”
Maybe the biggest challenge for oncologists, as we move into the next stage of the pandemic, is to be aware of this danger. Just as webinars and online discussions about emerging evidence and best practice regarding protocols and pathways will be essential, so will sharing best practice around ways to combat ‘psychological distancing’ during, and after, the pandemic.
The cartoon that illustrates this article is by Milo Manara, one of the most renowned Italian cartoonists. It is one of a series of cartoons he published on his social networks that paid homage to the people who kept working, and performed vital services, during the health emergency linked to Coronavirus. Manara’s designs are dedicated to healthcare personnel, transport workers, couriers, law enforcement personnel and supermarket clerks. In addition, the designer has made a short animated video dedicated to hospital staff, at the forefront of the pandemic.