The length of time it takes for each new cancer drug to reach the market – and more importantly, the patient – remains a cause of deep frustration particularly among those whose lives depend on accessing new options. Concrete data is hard to come by, but estimates of the time taken to complete clinical trials range from 10 to 15 years – and that does not include time spent identifying new drug targets or formulating them in a safe-for-human way. For rare cancers, the wait time is even longer.
Regulators have been trying to speed up the evaluation stage by ‘adjusting the screws’. Within the European Union, for example, the European Medicines Agency (EMA) can grant conditional marketing authorisation or accelerated assessment where an experimental product is deemed to address unmet medical need or to be of major interest for public health and therapeutic innovation.
Another possibility that could knock years off the drug development timeline would be to trial the use of drugs that have already been approved for one disease for treating a different disease or indication where there is a strong scientific rationale indicating potential benefit. Termed ‘drug repurposing’, this is a strategy that advocacy groups have long been campaigning for.
Potential time savings derive not only from the knowledge already developed around a drug’s mechanism of action, but crucially about its safety. Repurposed drugs will already have gone through – and if approved, passed – safety and toxicity testing. Clinical experience with the drug in the original indication may also provide some data for the repurposed indication. If the dose in the new indication is equal to or lower than the dose used in the original indication, much of the preclinical testing, safety assessment, and in some cases even Phase 1 clinical trials, can be used for the new indication. The big hope and expectation placed on repurposing is that such re-use – of knowledge, resources, testing time – would be more cost-effective and quicker than developing new cancer drugs from scratch, potentially making new cancer treatments available much faster and hopefully cheaper.
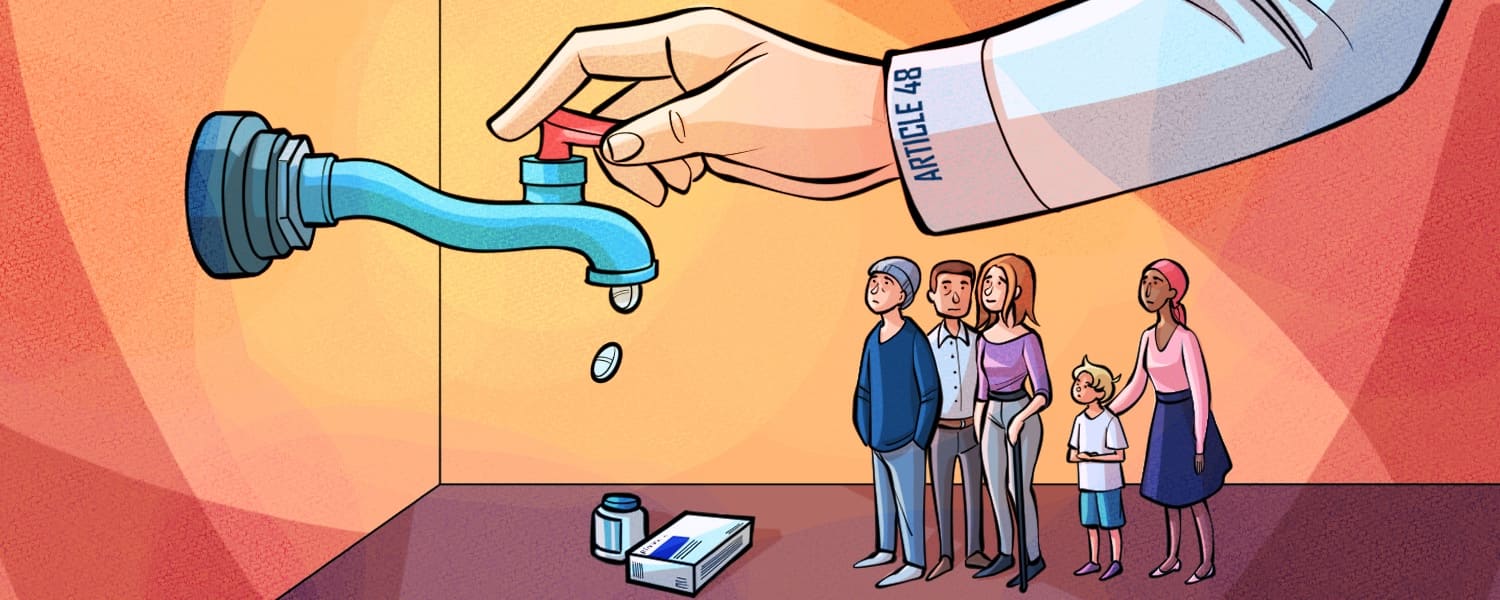
Yet, while common sense would seem to dictate it as a ‘no-brainer’, trialling an approved drug for a new indication is often not seen as a priority – or even a sensible business proposition – for the company that developed the drug. This matters, because as things currently stand, a proposal to seek regulatory approval from the EMA for using a drug in a new indication can only come from a company with active authorisation to market the drug – i.e. the pharmaceutical company that developed the drug or company manufacturing a generic version if there is one. That restriction could be removed, however, under a proposed change included in revisions to the EU Pharmaceuticals legislation, which has already been approved by the European Parliament. A lot now hangs on whether that change can pass the final hurdle of approval by the European Council.
Concept and history
Drug repurposing is defined as taking a drug that has been approved for one disease or condition and using the drug to treat a different disease or condition. The term covers the more common practice of extending the use of a drug to a related indication, e.g. using an oncology drug to treat a different type of cancer, which is termed ‘soft repurposing’, as well as the repurposing a drug for use in an entirely different condition – ‘hard repurposing’– e.g. using a non-oncology drug to treat cancer, rather than just to treat symptoms or side effects of cancer. “Hard repurposing is the much harder nut to crack, but in practice, repurposing is a spectrum,” says Pan Pantziarka, Programme Director for Drug Repurposing at the Anticancer Fund. As he points out, some cancers may share greater similarities than others: moving from leukaemia to solid cancer types, for instance, poses some major challenges.
Historically, there have been examples of successful repurposing, both soft and hard. The BCG vaccine was originally developed in the 1920s to treat tuberculosis and is still used for tuberculosis prevention. Then in 1976, the first use of intracavitary BCG against bladder cancer was published, and in 1997 the FDA approved the use of BCG in patients with superficial bladder cancer, where it remains the recommended standard treatment of high-grade non-invasive bladder cancer. Thalidomide, notorious for causing severe developmental defects when given to pregnant women, was first repurposed for treating leprosy and later for treating multiple myeloma. Propranolol, an early beta-blocker used for treating coronary heart disease and high blood pressure, has been repurposed for infantile haemangioma, with EMA approval in 2014. These cases underline the potential of drug repurposing: an already discovered mode of action of one drug is repurposed and reused for a different disease, where the same levers have to be pulled.
Thalidomide, notorious for causing severe developmental defects was repurposed for treating multiple myeloma
Successful repurposing cases such as these demonstrate that drugs approved for non-cancer indications can sometimes be repurposed to provide new treatment options for cancer patients – especially those with rare and ultra-rare cancers, where few therapies are available, and even fewer are in development.
In the past, the focus was mainly on re-using older drugs, which are often available as generics. More recently, however, attention has turned to repurposing recently approved drugs, which are still under patent protection, to treat cancers for which the drugs in question have not (yet) been approved.
From off-label to on-label
Knowing a drug works in one disease, and having a rationale indicating it might be effective in treating another, doesn’t mean the process of repurposing is plain sailing. Even after a potential candidate has been identified and validated preclinically, repurposed drugs typically need to undergo additional clinical trials, to assess safety and efficacy in the new patient population. The new indication may require a change in dosing or formulation, as well as manufacturing. A key question, which partly explains the low uptake of repurposing, remains: who should – or would want to – take on this process of redeveloping and retesting?
One deterrent from investing in going through the approvals process for a new indication is that, in serious diseases such as cancer, many drugs are already being used ‘off-label’ – i.e. without regulatory approval for that indication – particularly in rare cancers that have very few approved options. Is there a business case for companies to take their drug through the additional testing and approval process when they can be used off-label instead? An analysis by the Anticancer Fund and Swiss not-for-profit Rising Tide Foundation of data on active drug repurposing trials would seem to indicate that there is not. Their study showed that, out of 1,096 active or recently active clinical trials investigating the use of non-cancer drugs as treatment in cancer, only 73 trials were sponsored by a company; the vast majority of trials were sponsored by academic or clinical institutions (data as of Sept 2023).
Many companies don’t feel a push to move from off-label use to seeking approval for the indication, says Pantziarka. “If a drug is already being widely used off-label for a certain indication, the company may not feel compelled to pursue formal repurposing. They can benefit from the off-label use without having to take on the regulatory work.”
For patients, by contrast, there is a strong case for repurposing to be done through an official approval process, he adds. “Off-label use is not ideal, because first of all, patients are dependent on the willingness of physicians to prescribe, which might be limited because of the higher liability risk… There are also questions of reimbursement: In some cases, you may find a physician is willing to prescribe off-label, however, the drug may not be reimbursed.”
Access problems with off-label use can create inequalities, as Silvia Stacchiotti, a sarcoma specialist at the Istituto Nazionale Tumori in Milan, points out. “[In Italy], Access to an off-label drug is a regional, and even an institutional decision. There is no national approach, so there may be a region or an institution that will cover the cost, and others will not. With official EMA approval, access would be the same, at least across the country.”
“In some cases, you may find a physician is willing to prescribe off-label, however, the drug may not be reimbursed.”
Stacchiotti is a strong advocate for repurposing, and has herself led a study as part of a repurposing pilot with the EMA looking at the use of sirolimus (rapamycin) – developed and approved for kidney transplant patients, to prevent the body from rejecting the new kidney – to treat an ultrarare sarcoma called epithelioid haemangioendothelioma. “There is a big need for new treatments in sarcomas, a large group of different and completely heterogenous tumour types,” says Stacchiotti. “Only a very short list of drugs are formally approved in this indication, while several other drugs are known for being potentially active in at least selected sarcoma types. However, there is not interest from pharmaceutical companies to invest in these indications.”
An additional problem, explains Stacchiotti, is that the activity of a drug against sarcoma is often discovered later than in other cancer types, when a drug is already off-patent or almost off-patent. “Again, the reason is that sarcoma is not an interesting disease for pharmaceutical companies. With this background, repurposing is for me the most potentially relevant way to get active drugs available for patients affected by sarcoma – both paediatric patients and older patients.”
Unfortunately, so far, opportunities for realising the potential of repurposed drugs to meet the urgent needs particularly of patients with rare cancers have been few and far between. And “if we have had this conversation a few years ago, this is where it would have ended,” says Pantziarka. “But recently, we find that policy surrounding drug repurposing is suddenly an area with a huge amount of activity.”
Drug repurposing: the current system
One reason for the renewed interest, at least in Europe, is the proposed revision of the EU pharmaceutical legislation. For a drug to be repurposed and officially approved for use in another indication, the drug has to get EMA approval. Because this approval can currently only be applied for by a company with authority to market the drug, if they do not wish to do this, there is no way to get a drug approved for use in a new indication, even when academic trials or trials backed by independent consortia provided evidence that a drug could be of benefit to patients with unmet needs. In several cases, companies have been unwilling to apply for label extension, despite such third-party evidence.
Three examples of such blocked repurposing were described in the recent Anticancer Fund White Paper. One related to the treatment of alveolar soft-part sarcoma (ASPS), which is an ultra-rare soft tissue sarcoma for which no medicines in Europe have been specifically approved. Two classes of drugs have shown some activity in ASPS. Evidence from two small clinical trials shows that the antiangiogenic multikinase inhibitor cediranib was active in ASPS and associated with improved response and disease control rates. However, AstraZeneca, the manufacturer, has not sought approval for cediranib in ASPS, despite not having succeeded in getting approval for cediranib in Europe for any other indication. Immune checkpoint [PD-(L)1] inhibitors have also shown activity in ASPS in seven clinical trials, on the back of which the US regulators, the FDA, approved the PD-L1 inhibitor atezolizumab for the treatment of adult and paediatric patients (two years of age and older) with unresectable or metastatic ASPS. However, in Europe there is still no approved treatment.
According to the Anticancer Fund White Paper, “European investigators have approached MSD, owner of pembrolizumab – a PD-1 inhibitor – with a view to getting support for a registration trial but have been turned down, in part due to ‘strategic and business factors which are confidential and therefore would not be discussed outside the company’ (personal communication).”
In several cases, companies have been unwilling to apply for label extension, despite such third-party evidence
In angiosarcoma, another rare soft tissue sarcoma, a retrospective study provided an indication that pembrolizumab may improve survival rates. A proposal for a clinical study was declined, and the drug not supplied.
Then there is the example of sirolimus, which appears to slow the progression of epithelioid haemangioendothelioma. The use of sirolimus is supported by a consensus paper organised by ESMO, co-authored by Stacchiotti. Pfizer developed sirolimus, and the drug is now available in the US as a generic. However, no company has so far shown any interest in obtaining marketing approval for using sirolimus in epithelioid haemangioendothelioma. Effectively, for this group of patients, sirolimus can only be prescribed off-label, which for many of them may not be possible.
Pharmaceutical companies may refrain from seeking a label extension for several reasons, says Pantziarka. First, the business plan for rolling out a drug across several indications may not foresee a drug’s use in a specific indication – especially a rare disease – in the period of market exclusivity. In addition, a company may not see the value in investing the time and money needed to pursue additional testing for a further indication. And even when a third party, such as a not-for-profit or academic organisation, provides the evidence needed, additional time and money are still needed to pursue the label extension process.
Repurposing is increasingly becoming an economic and financial problem, rather than a medical one, says Pantziarka. “In our database of repurposing trials, we have registered almost 1000 active trials with several hundred drug candidates… The pipeline isn’t a problem and it’s an incredibly healthy ecosystem. If we were a drug company, we’d be laughing all the way to the bank because there are so many good prospects.”
Drug repurposing: proposed changes
The proposed new EU pharmaceutical package includes a provision to overcome this obstacle. Article 48 would allow not-for-profit entities to submit clinical evidence for a new therapeutic indication that is expected to fulfil an unmet medical need, to the EMA or to member states’ competent authorities, for their consideration. Based on the available evidence, the EMA may evaluate the benefit and risk of using the drug in the new indication. The opinion would be made publicly available and, if the opinion is favourable, the marketing authority holder would be required to submit a variation to update the Product Information Leaflet. Effectively, this allows third parties to go forward with a label extension.
If the legislation passes without any amendments to Article 48, the tables are turned. Even when no marketing authorisation holder is interested in repurposing, the available data can be submitted to the EMA and evaluated for label extension – clearing the way, for instance, for a request for sirolimus to be approved for treating patients with epithelioid haemangioendothelioma. By enabling a more straightforward path to label changes, Article 48 could incentivise more clinical research into repurposing opportunities, as researchers would be more confident that their evidence would be translated into patient access. “When we currently look at repurposing trials, so many of them, even Phase III trials, lead to headlines, conference talks or papers in high-impact journals. But it doesn’t go any further”, says Pantziarka. “Having a paper as an endpoint is fine for your career, but it’s the worst outcome for patients. So, this [adaptation] opens up the prospect that the endpoint is the patients getting access to their medicine.”
“Personally, I expect that the clinical trials landscape will change enormously as a consequence”
If the European regulations change, this may also change how clinical trials are initiated, says Pantziarka. “The Anticancer Fund funds clinical trials. In the current situation, we sometimes reject trials, because we think that there’s absolutely no way that the results will progress to the clinic. The company has, for example, definitively said that they are not interested. Now, with Article 48, funders could look at projects and know that, if the data produced is positive, they could go to the EMA and patients eventually will get the treatment. Personally, I expect that the clinical trials landscape will change enormously as a consequence.”
Remaining challenges
While the proposed new legislation, especially Article 48, could be a game changer for repurposing, there are still obstacles to be overcome. The European Parliament adopted its position at first reading, but the EU Parliamentary and national elections delayed the legislative package’s further progress through the legislative process. The next step will be consideration by the European Council, which has not yet adopted its position.
There may also be efforts to water down or limit the scope of Article 48, such as restricting it to only off-patent drugs. “Some organisations are pushing back against Article 48,” Patrizia Vandamme, Policy Officer at the Anticancer Fund, hints. “We should also make clear that Article 48 makes no change to the evidentiary requirements. Whoever comes with a dossier still has to show that drug has efficacy and an acceptable benefit to risk ratio. So we haven’t changed the goalposts, but if the data is strong enough, the drug has to be made on-label.”
There will no doubt also be a learning curve in getting the proposed new procedures to work effectively. To test the repurposing framework, following the discussions at the EU Commission Expert Group on Safe and Timely Access to Medicines for Patients (STAMP), a Repurposing Observatory Group (RepOG) was established. Its purpose is to define and test the practical aspects of a pilot project, with the aim to provide support to not-for-profit organisations generating or gathering data for repurposing an already authorised medicine.
“Getting not-for-profits and regulators together is an interesting learning exercise”
The pilot programme aims to clarify where the hurdles and challenges lie in the current regulatory process of repurposing. Among the selected cases, the Anticancer Fund worked with two academic and clinical ‘champions’ to go through the whole process required for obtaining a license extension. The two applicants submitted data packages for repurposed off-patent drugs to the regulators and were given the opportunity to go through the full scientific advice and regulatory approval process with the EMA. “Regulators and not-for-profit champions of a new drug come from different universes, and don’t speak the same language,” says Vandamme, who worked with clinicians on projects in the pilot programme, which included Stacchiotti’s study on repurposing sirolimus for epithelioid haemangioendothelioma. “Getting not-for-profits and regulators together is an interesting learning exercise.”
Additional hurdles that need to be addressed, in the event that Article 48 passes, include securing drug supply and funding for clinical trials, especially in the case of rare indications with small patient populations. Ensuring affordable patient access and reimbursement for repurposed drugs would also still require coordination between regulators, payers and industry. Nonetheless, as Pantziarka points out, “Article 48 as it currently stands will be the biggest and most fundamental change in repurposing in Europe.”
Repurposing in the US and the UK
In the US, off-label use of drugs is more common and accepted than in Europe; insurers will often cover drugs for off-label use if the drugs are included in clinical guidelines, such as those from the National Comprehensive Cancer Network (NCCN), for which there is no European equivalent. This means there is even less motivation for drug companies to pursue formal label expansions. In the US, it is the regulators, the FDA, that tries to promote drug repurposing. ‘Project Renewal’ reviews the labels of old approved generic cancer drugs, with the goal of identifying additional indications. The review is done by external experts using publicly available data to update certain older oncology drug prescribing information, including potential new indications. Where new indications are justified by the evidence, the FDA then invites the company to update the label.
In the UK, which is no longer covered by the EMA, repurposing is being promoted by NHS England under its ‘Medicines Repurposing Programme’, which identifies opportunities to use existing generics in new ways, and then puts out a tender inviting all manufacturers of the drug to offer a price for a label extension. The company with the lowest bid receives that money from the NHS, and in return, the company has to commit to sharing the data with other generics manufacturers. Suggestions for repurposing candidates can come from patient-focused voluntary-sector organisations, NHS clinicians and pharmaceutical companies. In November 2023, the first such license variation application supported by the programme was approved. The aromatase inhibitor anastrozole, which has been used for decades to treat breast cancer, had its licence extended in the UK for use as a preventive treatment in a defined group of post-menopausal women at increased risk of developing breast cancer.
Illustration by: Alessandra Superina