Women who ovulate for longer over the course of their lifetimes may have a higher risk of developing ovarian cancer. The international epidemiological study, published in Journal of the National Cancer Institute, 23 January, found that each additional year of ovulation was associated with a 4% increase in the risk of epithelial ovarian cancer. However, the picture was not that clear cut, with two ovarian cancer subtypes (mucinous tumours and high-grade serous) showing distinctly different risk factor profiles.
“Our findings show that all ovarian cancers are not equal. We think of epithelial ovarian cancer as one disease, but it’s actually a group of different diseases. The results show that different subtypes have different origins and point to where basic science research needs to go next to better understand how to prevent these diseases,” Francesmary Modugno, the senior author, tells Cancerworld.
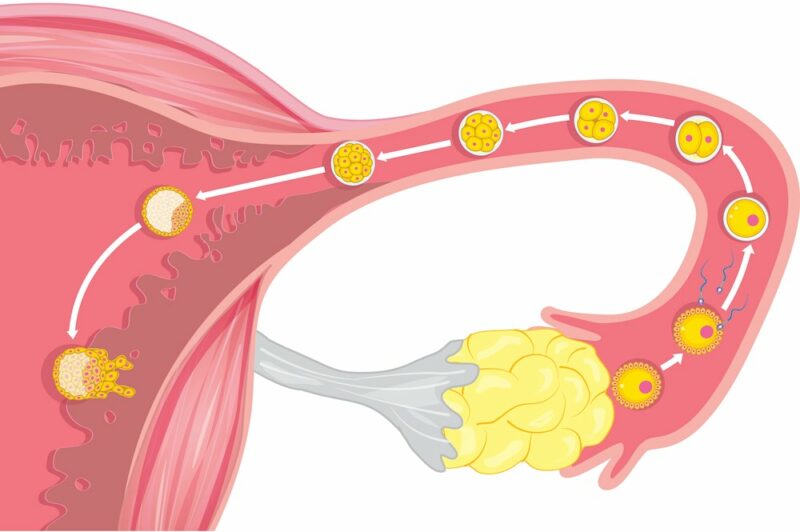
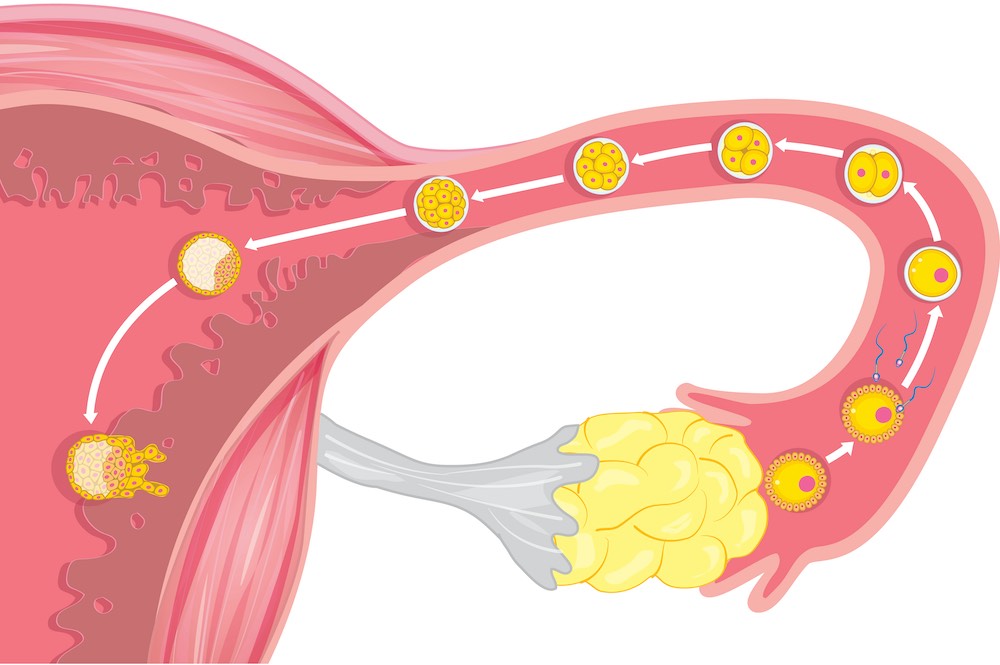
Oral contraceptives, having children, and breastfeeding have all shown consistent protective effects for ovarian cancer. However, while studies demonstrate that lifetime ovulatory years are associated with increased epithelial ovarian cancer risk, it has been unclear whether protective mechanisms arise through ovulation suppression alone or other factors. Furthermore, no individual study has been large enough to analyse individual epithelial ovarian cancer subtypes. Epithelial ovarian cancers account for over 95% of ovarian malignancies and are thought to arise from trauma and wound repair of the surface layer of ovarian cells as a result of ovulation. The main subtypes include high-grade serous ovarian carcinoma, endometrioid carcinoma, low-grade serous ovarian carcinoma, mucinous carcinoma, and ovarian clear cell carcinoma.
For the current study, the investigators pooled primary data from 21,267 women with ovarian cancer and 26,204 healthy controls who had been involved in 25 case-controlled studies. The studies, performed across four continents and nine countries, were undertaken by members of the Ovarian Cancer Association Consortium (OCAC), a forum of ovarian cancer investigators formed in April 2005. “By combining data from individual studies, we had enough power for the first time to carefully look at the individual subtypes. We wanted to get a handle on whether there were different risk factors that would imply that different subtypes arose from different origins,” explains Modugno, from the Magee-Womens Research Institute and UPMC Hillman Cancer Center at the University of Pittsburgh.
For ovarian cancer cases and controls (without ovarian cancer), investigators calculated lifetime ovulatory years as the time between the woman’s first and last menstrual period (her menstrual span), subtracting any time when she would not have been ovulating (pregnancy, oral contraceptives, breastfeeding). Multivariable logistic regression was used to estimate the odds ratio for the association between lifetime ovulatory years and epithelial ovarian cancer. The team utilised 12 different algorithms to assess the robustness of their results.
Overall, results showed that for all epithelial ovarian cancer subtypes, each additional year of ovulation was associated with a 4% increased risk of ovarian cancer.
When all subtypes were considered together, the estimated model coefficient protective effect for oral contraceptive use was 4.45 times greater than expected for the time period not ovulating; for pregnancy, the effect was 12 to 15 times greater, and for breastfeeding, it was 13 times greater. “The magnitude of these associations varied substantially from expectations according to the time period women were not ovulating. These data tell us that ovulation suppression alone is not the only mechanism underlying the protective effects of these factors. If that were the case, you’d expect similar results for similar time periods of oral contraceptive use and pregnancy (both preventing ovulation) to deliver the same benefits,” explains Modugno.
For the mucinous epithelial ovarian cancer subtype, total ovulation over a woman’s lifetime was not associated with cancer. However, the different factors contributing to total ovulations (oral contraceptive use, pregnancy, and breastfeeding) were. “This underscores that the mechanism of action for mucinous ovarian cancer was not through suppressing ovulation but by some other means,” explains Modugno.
High-grade serous ovarian cancer stood out as the only subtype where the mechanism of action appeared to be through ovulation suppression alone. “This is surprising because high-grade serous ovarian cancers are believed to arise in the fallopian tubes rather than the ovary. Thus, there must be something about ovulation beyond ovarian trauma impacting risk,” says Modugno. “Emerging data suggest that it may be the follicular fluid released at ovulation which reaches the fallopian tube that may lead to cancer initiation.”
The authors conclude that, taken together, the data imply that mechanisms beyond ovulation suppression, such as hormonal alterations or inflammation, are contributing to the association between lifetime ovulatory years and epithelial ovarian cancer. Going forward, Modugno says, the team hope to use the information to develop risk assessment models that clinicians can use to screen women to identify those at high risk who may benefit from specific prevention strategies.
The team also hope their epidemiological work will inspire basic scientists to undertake animal and in-vitro ovarian cancer studies to shed light on potential mechanisms. “Understanding these mechanisms can ultimately open new avenues for ovarian cancer prevention,” says Modugno.