Combining computed tomography (CT) scans, spatial radiomic maps, and ultrasound (US) images creates a visual guide that helps doctors perform fewer and more accurate tumour biopsies. The feasibility study, published in European Radiology (14 December), demonstrates how imaging can be used to non-invasively unravel the heterogeneity of ovarian cancer tumours and guide targeted biopsies. The University of Cambridge investigators believe that their integrated imaging approach could ultimately open the way for ‘virtual biopsies’ sparing patients invasive procedures.
Patients with ovarian cancer undergo a number of biopsies to obtain cancer tissue to confirm diagnosis for chemotherapy treatment. Biopsies are also needed for molecular profiling to test whether patients have BRCA1 or BRCA2 mutations in their cancer tissue, indicating that PARP inhibitors may be more effective. “The challenge is to get a good biopsy containing enough tissue for both cancer diagnosis and molecular profiling of the tumour. Tumours are heterogenous and it would be really helpful to be able to target the biopsy to the regions of the tumour that are most important,” explains James Brenton, Professor of Ovarian Cancer Medicine at the University of Cambridge and the medical oncologist on the team who undertook the study.
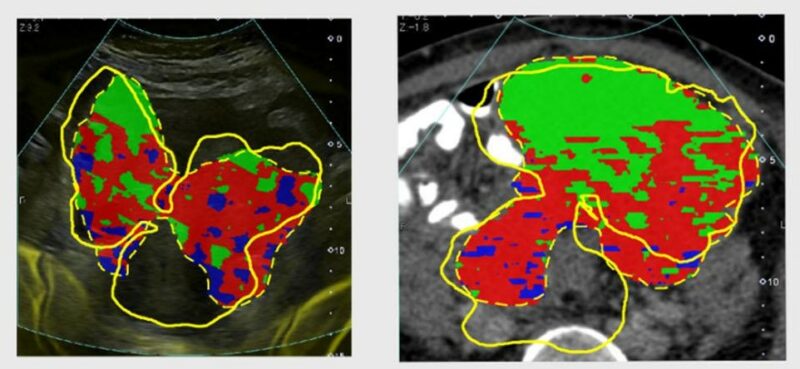
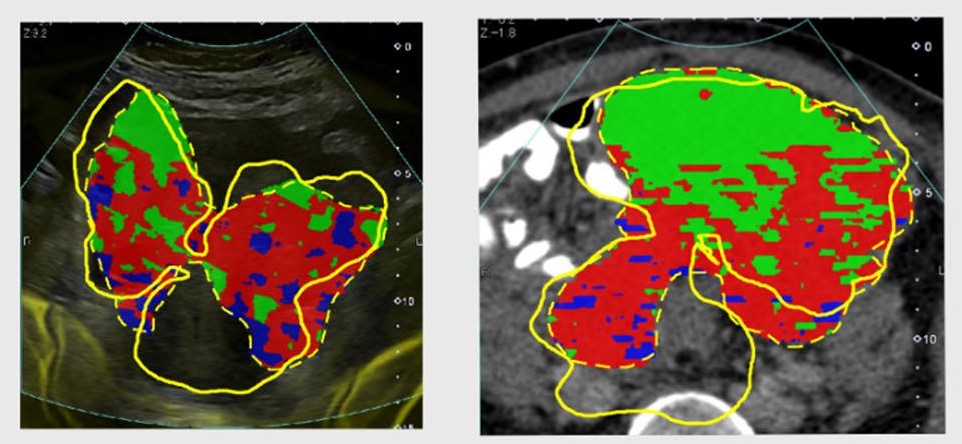
The integrated medicine approach, pioneered by the CRUK Cambridge Advanced Cancer Imaging Programme team, combines patient data from multiple sources to facilitate biopsy. For the study, CT scans of the tumours were subjected to radiomics, an approach that mathematically extracts the signal intensities and pixel interrelationships of the image to provide quantitative descriptions. “Radiomics tells us how texture and intensity changes across the tumour, allowing us to define different spatial regions with the same characteristics,” explains Mireia Crispin-Ortuzar, the physicist on the team.
Each different heterogenous region, known as a habitat, can be given a different colour code allowing investigators to visualise a number of distinct biological regions. The timeline involves undertaking the CT scan, then radiomics being performed and finally superimposing the CT radiomics habitats on to the real-time ultrasound to provide landmarks for biopsy. “In reality only a limited number of biopsies can be taken. This integrated approach allows the team to choose the lesions to biopsy that will provide the most meaningful information,” explains Evis Sala, Professor of Oncological Imaging at the University of Cambridge, who is leading the programme.
In the single-centre study, the team used the integrated approach for the first time on six women with advanced ovarian cancer, who were due to undergo US-guided biopsies before starting neoadjuvant chemotherapy. The investigators successfully demonstrated the different habitats of tumours, displayed them in real time, used the information to inform the location of biopsies, and obtained high quality tissue samples that were sufficient for routine workup and genomic analysis.
For reliable habitat-guided tissue targeting, accurate spatial registration between the CT and US images (known as fusion accuracy) is a prerequisite. When the team compared the contours of the US and CT scans, they found that the fusion accuracy was high for larger pelvic tumours but lower for the smaller omental metastases. This, the authors, suggest, may be explained by the larger tumour volume of the pelvic lesions and their relatively fixed position in the pelvis compared to the more flexible and smaller omental deposits.
The team now plan to discover and validate radiogenomic biomarkers in patients with ovarian and kidney cancers.
“One of the reasons the technique is so exciting is that it allows us to sample tumour habitats in vivo. It means that we may be able to track whether therapies are working,” explains Sala. “Ultimately, if we have biological validation to show the patterns of different tumour mutations we may be able to avoid biopsies altogether.”
Commenting on the significance of the study, Iain McNeish, Director of the Ovarian Cancer Action Research Centre, Imperial College London, says, “Obtaining a high quality biopsy is essential in women with ovarian cancer. Not only does this ensure that an accurate diagnosis is made, it also means that there will be enough material to perform detailed molecular analyses that are increasingly important for directing patient care. This study will ensure that radiologists know exactly which area to target for biopsy, thus ensuring that patients are diagnosed as quickly and reliably as possible. Importantly, this work can be readily applied in routine patient care immediately.”