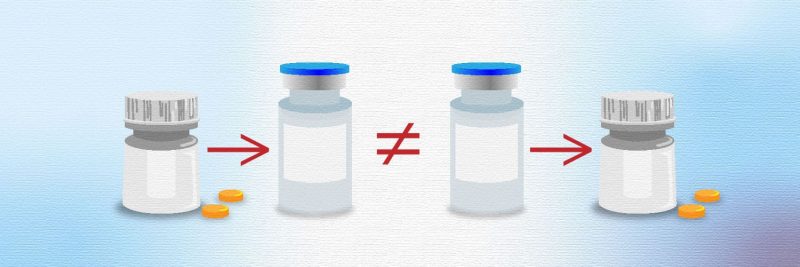
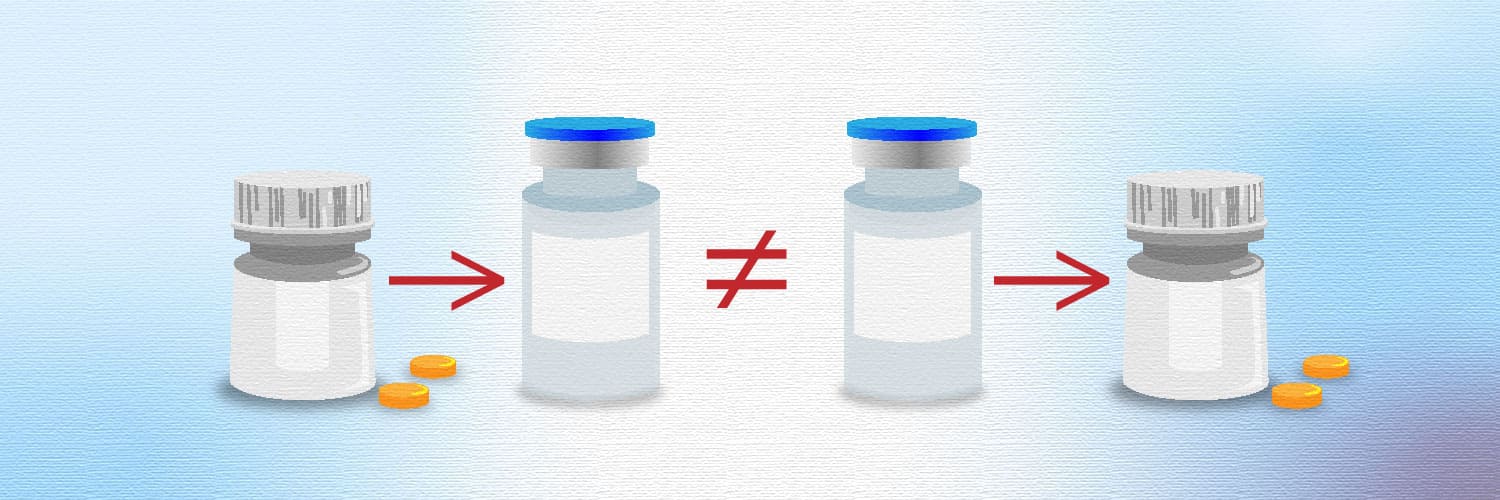
Patients with metastatic melanoma who received immunotherapy before targeted therapy showed a 20% overall survival advantage at two years versus those receiving targeted therapy first, with immunotherapy after. The final results of the DREAMseq trial, published in the Journal of Clinical Oncology (September 26), concluded that the combination of nivolumab/ ipilimumab followed by BRAF and MEK inhibitor therapy (if necessary) should be the preferred treatment sequence for patients with metastatic BRAFV600-mutant melanoma.
“I think the standard of care should immediately change because these are FDA-approved regimens,” says lead researcher, Michael Atkins, from Georgetown Lombardo Comprehensive Cancer Center, Washington DC.
“This data will guide physicians around the globe who care for patients with BRAF-mutated metastatic melanoma on the proper order of treatment so as to obtain the best survival,” says investigator Andrew Pecora, who led the trial at the John Theurer Cancer Center campus in Hackensaw, New Jersey.
Immune checkpoint inhibitors and targeted therapies are the preferred treatment options for patients with advanced BRAF-mutant melanoma. Approximately 50% of patients diagnosed with cutaneous melanoma have BRAF mutations, with substitution of glutamic acid for valine at position 600 (V600E) being the most common, accounting for ≈90% of all BRAF mutations. BRAF mutations can be targeted with a combination of dabrafenib (a BRAF inhibitor) and trametinib (a MEK inhibitor). While targeted medications and immunotherapy have become standard of care in advanced melanoma, the optimum sequence of treatment was unknown.
The Doublet, Randomized Evaluation in Advanced Melanoma Sequencing (DREAMseq) trial, which started in July 2015, was designed to explore whether nivolumab/ ipilimumab followed by dabrafenib/ trametinib offered the best therapeutic sequence, or vice versa. It was run on behalf of the ECOG-ACRIN Cancer Research Group and sponsored by the US National Cancer Institute.
In the phase III trial, 265 patients with treatment-naïve BRAFV600-mutant metastatic melanoma were randomised in Step 1 to receive either combination nivolumab/ ipilimumab (Arm A, n=133) or dabrafenib/ trametinib (Arm B, n=132). At disease progression they were enrolled in Step 2 to receive the alternate therapy, dabrafenib/ trametinib (Arm C, n=27) or nivolumab/ ipilimumab (Arm D, n=46). To be eligible patients had to have histologically-confirmed, RECISTv1.1 metastatic, unresectable stage III or IV melanoma containing a BRAFV600E/K mutation by a Clinical Laboratory Improvement Amendments (CLIA) approved assay. The trial was stopped early due to clear evidence of benefit for giving immunotherapy first.
Results showed two-year overall survival was 71.8% for those starting on Arm A (combination nivolumab/ ipilimumab) versus 51.5% for those starting on Arm B (dabrafenib/ trametinib)(log-rank P=0.010).
Step 1 progression-free survival favoured Arm A over Arm B (P=0.054). Objective response rates were 46.0% for Arm A, 43.0% for Arm B, 47.8% for Arm C and 29.6% for Arm D.
Crossover occurred in 52% of patients with documented disease progression.
The incidence of Grade ≥3 treatment-related adverse events occurred with similar frequency between arms: 50.5% in Arm A, 53.1% in Arm B, 53.8% in Arm C and 50.0% in Arm D.
“With further analysis of the data since our initial report, we not only know that patients with metastatic BRAF-mutant melanoma in general do better when combination immunotherapy is administered prior to combination targeted therapy, but we also have a better idea as to why. Specifically, combination immunotherapy, in contrast to targeted therapy, produces more long-lasting tumour shrinkage, reduces the risk of disease progression in the central nervous system and doesn’t interfere with the subsequent effectiveness of the alternative treatment approach,” says Atkins in a press release.
Remaining questions include whether the same benefits will hold for patients treated with single immunotherapy drugs (nivolumab or pembrolizumab) rather than the combined immunotherapy drugs (ipilimumab plus nivolumab) used in the study.
Another recent study revealing important information about the sequencing of melanoma therapy was SWOG S1801, presented in the Presidential Symposium at ESMO 2022 on September 11. SWOG S1801 showed that patients with high-risk melanoma who received the immunotherapy drug pembrolizumab both before and after surgery to remove the cancerous tissue had a significantly lower risk of cancer recurrence than patients receiving the drug only after surgery.In S1801, 345 participants with stage IIIB–IV melanoma that was deemed operable were randomised to 200 mg of pembrolizumab every three weeks administered after therapy (adjuvantly) or 200 mg of pembrolizumab every three weeks for three doses leading up to surgery (neoadjuvantly), with a further 15 doses following surgery.
Results showed that event-free survival was significantly higher for neoadjuvant therapy versus adjuvant therapy (HR 0.59, P=0.0015). Furthermore, more deaths occurred in the adjuvant group – 22 versus 14 in the neoadjuvant group (HR 0.63, P=0.091).
“It’s not just what you give, it’s when you give it! SWOG S1801 demonstrates that the same treatment for resectable melanoma given in a different sequence can generate lower rates of melanoma recurrence,” says Sapna Patel, the study leader from The University of Texas MD Anderson Cancer Center.
Commenting on the results, Marco Donia, from the National Center for Cancer Immune Therapy (CCIT-DK), Copenhagen University, says, “Neoadjuvant immunotherapy in resectable melanoma is particularly intriguing. Stimulating a patient’s immune response to intact tumours may benefit from a more natural immunological milieu and improved tumour-antigen presentation. This strategy is being evaluated in multiple clinical trials and settings where available treatments are used in a different sequence than the current standard.”