Targeting a specific enzyme in muscle could help cancer patients avoid the muscle wasting condition cachexia. The study, published in PNAS (October 17), found that a previously overlooked enzyme, known as UBR2, plays a critical role in cancer patients developing cachexia, by selectively degrading two myosin heavy chain subtypes.
“We believe that we have identified the pathway causing loss of myosin subtypes IIb and IIx, the proteins responsible for muscle contraction, in cachexia,” says Yi-Ping Li, the senior author from The University of Texas Health Science Center at Houston. “The findings will fill a key gap in understanding how cancer causes muscle mass and function loss.”
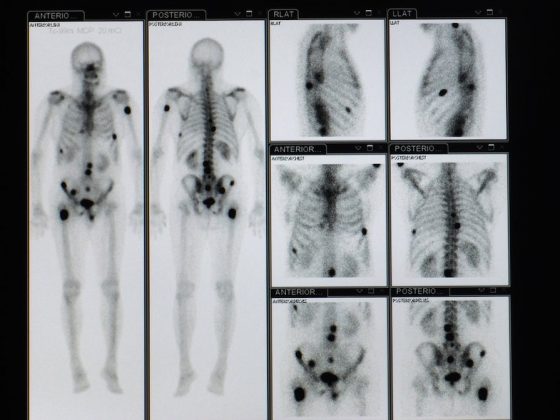
Cancer-induced cachexia is a wasting syndrome that features progressive loss of muscle mass largely due to excessive proteolysis. Cancer cachexia not only impairs the cancer patient’s body metabolism and physical capacity, but also decreases the efficacy of chemotherapy. Affecting ~60% of cancer patients, cachexia is the direct cause of around one-third of all cancer-related deaths. However, the detailed mechanisms through which cancer causes muscle wasting have not been defined, with poor understanding hindering the development of clinical interventions for cancer cachexia.
In the current study, Li and colleagues set out to identify the key molecules within muscle cells responsible for the excessive muscle protein degradation that occurs in cancer cachexia.
In a mouse model of cancer cachexia, they found that an inflammation signalling pathway involving p38β MAPK activation of transcription factor C/EBP is responsible for the bulk of muscle protein degradation. Furthermore, they found that C/EBP upregulates a previously overlooked E3 ubiquitin ligase, UBR2, in response to tumour burden. They found that induction of myosin heavy chain loss and atrophy of C2C12 myotubes in the mouse tibialis anterior by murine cancer cells required the UBR2 enzyme to be upregulated.
The investigators went on to demonstrate that genetic gain or loss of UBR2 function inversely altered myosin heavy chain (MHC) levels and muscle mass in the tibialis anterior muscle of tumour-free mice. Elevating levels of UBR2 in the muscle of mice both with and without tumours caused loss of MHC-IIb and MHC-IIx, but not MHC-I or MHC-IIa or other myofibrillar proteins.
Muscle-specific knockout of UBR2 spared tumour-bearing mice from losing MHC-IIb and MHC-IIx, fast twitching muscle mass, cross sectional area, and contractile forces.
To determine whether cancer patients with cachexia also suffer from UBR2-mediated selective loss of specific myosin heavy chain subtypes, the team examined rectus abdominis muscles that had been collected from male patients with gastrointestinal or genitourinary cancers who had either experienced weight loss or who were weight stable and compared them with muscle taken from non-cancer patients who were weight stable. They found that muscle taken from both weight loss and weight stable cancer patients possessed higher levels of UBR2 and lower levels of total myosin heavy chain (MHC) than weight stable non-cancer patients. Furthermore, UBR2 levels were found to be progressively higher in cancer patients who had experienced weight loss in correlation with a selective loss of MHC-IIx.
“Our data that deleting UBR2 protected fast muscle mass and function in tumour-bearing mice suggests that an effective intervention of cancer cachexia should have the capacity to protect MHC-IIb/IIx from UBR2-mediated degradation. Thus strategies for inhibiting UBR2 or its up-regulation by p38β MAPK and p300 could be developed for intervening in cancer cachexia,” write the authors
UBR2, explained Li, is upregulated by p38β MAPK, a protein kinase that can be inhibited by nilotinib, a drug already approved for treating chronic myelogenous leukaemia (CML). The team now plan to use nilotinib in clinical trials of patients with cachexia.
“Ultimately, if we were able to control cachexia this would help cancer patients to live longer and could potentially turn cancer into a chronic disease,” Li told Cancerworld.