The job of a radiation therapist may sound straightforward: deliver the right dose of radiation to the right location. But it’s not. These are complex tasks that involve working with data, high-tech equipment and patients. Moreover, by doing each task correctly, the risks to patients can be minimised so they derive the greatest benefit from treatment (Box). At every step of the way, an error may occur, with potentially disastrous consequences for the patient. Given this responsibility, it might seem reasonable to assume that radiation therapists receive extensive training. But across the world, including in Europe, the education and further training of radiation therapists (RTTs) are on shaky ground, says Mary Coffey, Adjunct Associate Professor in Radiation Therapy at Trinity College Dublin. “The public, and even people within the discipline itself, have no idea that the people who are actually giving the treatment in many instances have no or very little knowledge of what they do.”
The core problem lies in variations in the quality and extent of education covering specific radiotherapy content, says Coffey – coupled with a certain indifference towards the profession. “There is a feeling that the medics are very well qualified, so that treatment prescriptions are very well done. And medical physicists make sure the equipment is functioning really well. So nothing can go wrong! But they forget that it’s actually the RTT who has to put the patient on the bed, in the right position, and turn on the machine and deliver the radiation dose that’s prescribed.” Added to that, radiation therapists are involved in treatment preparation and patient care. “This is a key point in the treatment chain that people don’t appreciate.”
“They forget that it’s the radiation therapists who put the patient on the bed, in the right position, and deliver the prescribed radiation dose”
No title, no recognition
Currently, across Europe, no unified educational programme exists to prepare radiation therapy professionals. Indeed, the problem starts at an even more basic level: a lack of a unified title. “Radiation therapists, first of all, are not recognised as a profession,” says Michelle Leech, Associate Professor and Head of Radiation Therapy at Trinity College Dublin. “Even in Europe, we have 28 different titles for the profession, which makes it hard to compare curricula, training and competences across the continent. This lack of a unifying title is the first step. Radiation therapists not being a recognised profession is really the main stumbling block for any education.”
Europe’s radiology and oncology society (ESTRO) and the International Atomic Energy Agency (IAEA) are working on defining an internationally comparable, recognised title for the profession. The acronym RTT is recognised by both bodies, standing for Radiation TherapisTs. This title could then be used on the international stage, in addition to national titles for the profession.
The current problems may arise, in part, from the history of radiation therapy. Historically, radiation therapy was delivered through large radiology fields with less potential for missing the tumour, but greater risk to normal tissue. No specialist education was required, because radiation therapists were drawn from a range of backgrounds and minimal radiotherapy content was included in educational programmes, explains Coffey. In the past decades, however, radiation therapy has developed into a highly complex discipline. With current approaches, small precise areas conforming more to the tumour are targeted. This limits the dose delivered to normal tissue, improving outcome and quality of life for patients. In this setting, however, the need for accuracy is critical and the risk of errors can be greater if positioning is incorrect.
In 2011, ESTRO carried out a survey on how educational programmes prepare RTTs for this complex role. This, with responses from 28 European countries ‒ though possibly somewhat dated now ‒ showed that frequently RTT education is a component of a broader programme, in nursing, diagnostic imaging or a technical discipline. Although the education programme is, in some cases, at degree level, the academic content relating to radiotherapy is often limited, and relevant clinical education may be confined to just a few weeks of learning.
As Coffey points out, without recognition as a profession, it is difficult to insist on a standard of competences and a standard of education that achieves these competences. “Historically, radiation therapists have not been recognised as a profession within its own right. You find it lumped with something else, as part of radiography, for instance. But actually treating a patient on a linear accelerator is a very different process than taking an X-ray. Being competent to take X-rays doesn’t make you competent to treat a patient,” explains Coffey. “By the same token, if the background is nursing, which is a requirement in some countries, that is very positive from the patient care perspective. But a nurse has no education and technical understanding of what happens when you turn on a treatment unit and the potential for harm to your patient.”
“Being competent to take X-rays doesn’t make you competent to treat a patient”
Currently, the therapeutic relationship acknowledged in the term ‘radiation therapists’ is also rarely emphasised in educational programmes. Radiation therapists usually see a patient for the entire period of treatment, often over several weeks, during which they monitor side effects, discuss psychosocial conditions and provide support, explains Leech. “We very much see ourselves as therapists. We are here to support and educate the patients about their treatments, make sure they’re involved, listen to them, support them in managing their side effects. It’s a profession that, when the person is educated, contributes to the holistic way of providing cancer treatments.”
The therapeutic aspect also affects the education required to carry out the job, adds Coffey. “That’s why we want to move away from radiography. Radiation therapy is a therapy discipline, in the same way as a physiotherapist or an occupational therapist, because you treat a patient. This is key, because you need to incorporate psychology, communication and patient care in the teaching environment.”
How the limitations in education and training of radiation therapists affects patient care is known only anecdotally. A 2008 review of radiotherapy incidents by the WHO showed that, although a significant proportion of incidents could be traced to incorrect equipment use or setup, contributing factors included “incorrect treatment decisions, mistaken treatment delivery and inadequate verification of treatment, due to inexperience and insufficient knowledge of the staff involved.”
“There is currently no equality of care in radiation therapy across Europe, and it’s not just about access, it’s in the actual delivery of treatment, which is nowhere near equitable,” explains Leech. Velimir Karadža, Head of the Radiotherapy/Technology Unit at the Clinic of Oncology, University Hospital Center Zagreb, in Croatia, echoes this feeling. “I’m sure there have been more mistakes happening than we actually detect. But people need to have the awareness. If people are not educated well enough, they will not care, they will not see, and they will not detect the error.”
Unlike many other disparities in cancer care, this is not a divide between the ’old West’ and the ‘old East’. “It’s not specific to eastern Europe at all,” says Coffey. “Countries like Australia and New Zealand, the UK, and Ireland have strong, dedicated programmes. But for example in Portugal, an excellent course in radiotherapy was closed down and replaced with a joint radiography programme.” What is added in eastern Europe is that many countries are quickly catching up in their radiotherapy standards, says Siret Kivistik, radiation therapist at Tartu University Hospital and radiotherapy lecturer at Tartu Healthcare College, in Estonia. “The development in our country has been huge… in the 12 years that I have been actively working in this environment. So the need for trained people really grows day by day.”
Train the Trainers
Efforts have been made to improve RTT education across Europe. “Radiation therapists on the ground are dissatisfied,” says Leech. “They know that their standard of care could be better… and want to change it from the ground up.” Helping drive this change is ESTRO’s RTT Committee, which was established in 1993 to represent radiation therapists at the European level. ESTRO supported the development of a core curriculum for radiation therapists, which was first published in 1995 with the third and latest revision published in 2011. This core curriculum sets standards for education of radiation therapists and links these to core competencies. Courses designed to fit this core curriculum should equip graduates with the defined competencies.
Additionally, ESTRO and IAEA have collaborated in a Train the Trainers programme, which started in 2008. This seeks to empower radiation therapists to address educational needs within their own countries. After a week-long training, given to three participants from each participating country, the participants organise three courses on RTT-specific topics for other radiation therapists in their own countries. Five rounds of this ‘Train the Trainers’ programme have been completed so far.
One consequence of this project has been increased networking among RTTs. In the Balkans, this has led to the establishment of an international platform for cooperation to exchange knowledge, experiences and solutions. Four meetings have been held so far in the Balkan region, under the title South East Europe Technology in Radiation Oncology (SEETRO) congress. The project is also helping radiation therapists to push for increased recognition of their profession. “A lot of countries have actually set up their own RTT society, and in several countries they’re working in that direction,” says Coffey.
One aim of the Train the Trainers project was to influence national education, so that the radiotherapy component of programmes is increased. Karadža is one of the driving forces behind the SEETRO Congress and RTT training programmes in Croatia. “Our workshops and symposia raised awareness about the problems. But to make this something permanent, the only way is to change the official educational programme,” he says. That is not always easy to achieve, says Leech. “There must be an internal recognition in various countries that there’s actually a problem. And there must be a recognition by the educational institutes themselves that the programmes they are running are not fit for purpose, that they do not teach the fundamental science, that is necessary to understand your actions on a radiation therapy unit.”
“To make this permanent, the only way is to change the official educational programme”
New models for education in Croatia and Estonia
In trying to change education in Croatia, Karadža and colleagues started out by drawing up the competences that RTTs would need. “Even the educational bodies participated in that, but when we tried to make the actual changes to education itself, we encountered problems.” Nevertheless, in 2019, radiation therapists were, for the first time, appointed as lecturers at the University of Applied Health Sciences in Zagreb, Croatia. “We think this is absolutely mandatory, that people from the profession are teaching students about professional issues.” Now, Karadža seeks to change the curriculum further. “But it takes time to convince the Dean of the Faculty and everyone that they need to just cut off some subjects and bring in new learning.”
Coffey, set up a degree programme for radiation therapists at Trinity College Dublin, which has been further expanded by Michelle Leech. In countries with limited resources, Coffey argues that is important to use a ‘pick and mix’ approach to design a course containing the most relevant existing educational content, tailored to future radiation therapists, rather than trying to establish a more costly full degree programme. “If constrained by time and resources, education should be tailored and focus on teaching key areas of radiotherapy,” she says.
In Estonia, Siret Kivistik has been instrumental in setting up a two-year MSc course for radiation therapists, for which she is now the course coordinator. Estonia faces an additional problem: as the country is small, only two clinical departments in Estonia offer radiotherapy services, with a total of only six linear accelerators available in the country. “We’d need to have 15 students per year to set up a dedicated programme at BSc level. But with just two clinical departments, we do not have enough positions to offer to 15 graduates each year.” A joint programme by the Baltic States to provide radiotherapy education was envisaged and developed, but failed for political reasons. An international MSc programme focusing on radiotherapy is now in its second year at Tartu Healthcare College in Estonia. The course is intended both for already practising radiotherapists, as well as for graduates of related disciplines without prior experience. “This programme, however, teaches a lot of the skills and knowledge that graduates should know already, entering a Master’s level programme. But we get great backing from the clinical departments, and we are in a good situation, having such a programme established.” In a next step, Kivistik wants to safeguard proper education for everyone in the radiotherapy departments as part of Estonia’s next cancer strategy.
Lack of traction at a policy level is one hurdle radiation therapists are facing. “We did try to have events inviting the ministry of health and education from various countries to attend, but we had to abandon this because there was no interest in us. It’s very difficult, we never reach the top level of government,” says Leech. There are also challenges at the level of professional societies, because radiation therapists are frequently members of organisations where other professions, such as nursing or radiography, are in the majority. This can make it hard to ensure attention is paid to their specific interests and needs. “One head of a national radiography society told me that radiographers might get bored with diagnostics and want to do a bit of therapy. So therapy is still being seen as an add-on to diagnostics” says Coffey, who also encounters the fear of RTTs taking away the responsibilities from other professions. “We are not about educating people to take over someone else’s job, which is another big fear… it’s not about that, it’s about educating radiation therapists to do their own job.”
“They work really hard and care deeply for their patients, but it’s difficult without proper understanding of what happens when they treat a patient.”
Coffey insists that, currently, radiation therapists in all settings are doing as good a job as they can do, given the circumstances. “I’m not taking away from the people on the ground, they work really hard and care deeply for their patients, but it’s difficult without proper understanding of what happens when they treat a patient.” She points to her own graduate students participating in discussions in multidisciplinary teams on an equal footing. “It’s terrific to listen to the students actually discussing with the rest of the team from a point of absolute understanding, and it becomes an equal discussion. It just enables everybody to do a better job.”
Leech points out what is at stake. “Who would you like to be treating your child? The person who is specialised in this area or someone who maybe sees this case once or twice? I think citizens know the answer to that question.”
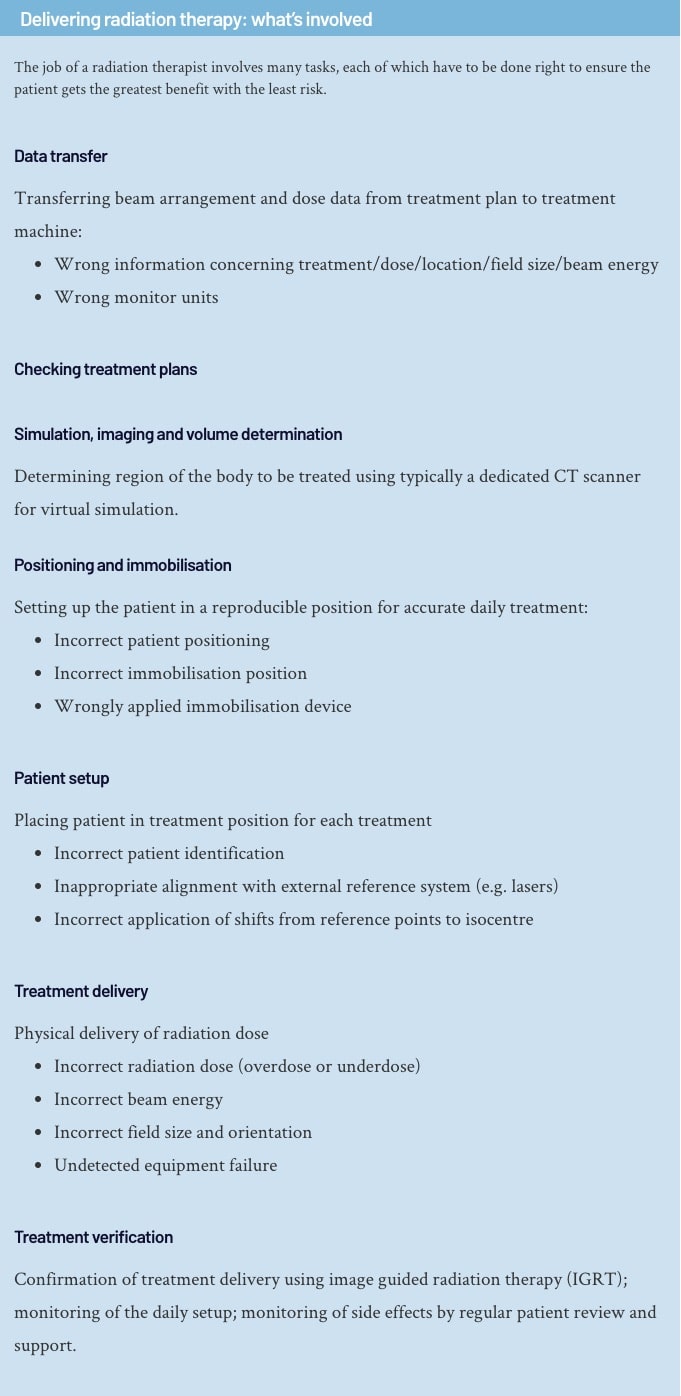
Delivering radiation therapy: what’s involved
The job of a radiation therapist involves many tasks, each of which have to be done right to ensure the patient gets the greatest benefit with the least risk.
Data transfer
Transferring beam arrangement and dose data from treatment plan to treatment machine:- Wrong information concerning treatment/dose/location/field size/beam energy
- Wrong monitor units
Checking treatment plans
Simulation, imaging and volume determination
Determining region of the body to be treated using typically a dedicated CT scanner for virtual simulation.Positioning and immobilisation
Setting up the patient in a reproducible position for accurate daily treatment:- Incorrect patient positioning
- Incorrect immobilisation position
- Wrongly applied immobilisation device
Patient setup
Placing patient in treatment position for each treatment- Incorrect patient identification
- Inappropriate alignment with external reference system (e.g. lasers)
- Incorrect application of shifts from reference points to isocentre
Treatment delivery
Physical delivery of radiation dose- Incorrect radiation dose (overdose or underdose)
- Incorrect beam energy
- Incorrect field size and orientation
- Undetected equipment failure
Treatment verification
Confirmation of treatment delivery using image guided radiation therapy (IGRT); monitoring of the daily setup; monitoring of side effects by regular patient review and support.Ilustration by Alessandra Superina










2 comments
The Strength of Chain is determined by the Weakest Link. Our RTT Colleagues deserve much better attention then what they are getting in terms of task recognition & professional development and growth planning.
Comments are closed.