Interview with Thomas Hofmarcher, health economist, IHE – The Swedish Institute for Health Economics, Lund, Sweden.
Q. Which is the origin of your idea of studying the cost of cancer in Europe? Does the Swedish Institute for Health Economics have a special interest in the topic?
A. Our interest in studying this topic goes back over 15 years in time. It all started with the drug approval of trastuzumab for the treatment of breast cancer by the European Medicines Agency in 2000. This drug was seen as a major breakthrough and in fact marked the starting point of personalized medicine in cancer care. At the same time, trastuzumab came with a significant price tag. A wave of new drugs followed trastuzumab and this sparked a lot of interest in two basic questions: how much are we spending on cancer care, and how much are we spending on cancer drugs?
Prof. Jönsson and Prof. Wilking have provided answers to these question in a report published in 2005. Since then they have teamed up with us at the Swedish Institute for Health Economics. Cancer care is evolving rapidly and thus there is a constant need to keep the numbers up to date. Cancer is also high on the political agenda but far too often a comprehensive view on the economic impact of cancer is neglected in political deliberations. We have therefore provided one update on the cost of cancer in 2016 and this year we have once again published the latest numbers.
Q. How difficult was to have data from the different national sources?
A. Data availability is really the dealbreaker in conducting this type of analysis. We cover 31 European countries in total. You can imagine that looking for data for each individual country takes a lot of time, especially since we are also looking at different types of costs. For direct costs of cancer, which are expenditure on cancer care made within the health care system, we tried to obtain data from national health accounts of countries. With the exception of Germany and the Netherlands, there are no countries where official sources (such as the Ministry of Health or the National Statistical Office) provide this kind of data on a regular basis. It is astonishing to realize that most countries have little clue on how much they are spending on specific diseases such as cancer. So instead we had to rely on country-specific data provided from research institutes, national cancer societies, articles in peer-reviewed journals and reports from the OECD and the WHO.
For indirect costs of cancer, which are composed of productivity loss attributable to premature mortality and to morbidity, the data availability situation is mixed. On the one hand, costs of premature mortality are relatively easy to estimate, since information on the age of death of people, which is the key input here, is readily available for all countries from Eurostat. On the other hand, costs of morbidity are difficult to assess as we lack data on sickness absence and early retirement caused by specific diseases such as cancer in many countries. We had to rely on studies conducted by other researchers to fill this data gap, which was also the case for our assessment of the informal care costs of cancer.
Q. The cost of cancer per capita in Switzerland is, according to your study, nearly 4 times higher than in Romania. Are survival rates also 4 times higher?
A. No, they are not. Switzerland is indeed always among the top countries if we look at survival rates of different cancer types. Romania is always close to the bottom of the ranking. When we look at the relationship of direct costs spent on cancer care and survival rates, we see a positive relationship.
Thus, countries that spend more also achieve better outcomes. But this relationship is not linear. That is, if you increase spending by 20 percent, survival rates will increase by less than 20 percent. If you spend your money on ineffective measures you might not see an increase at all. Spending more money to improve outcomes should be a priority, but this priority should be on an equal footing with trying to make the best out of the money that is already being spent. A review of the cost-effectiveness of current practices can reveal potentials for improvements in the allocation of resources. This will help bringing benefits to patients and, in some cases, even save money.
Q. Expenses for cancer drugs seem to represent exactly one third of the direct cost of cancer: did you expect more? Or less?
A. What we see is that the share of direct costs that is spent on cancer drugs has been increasing steadily throughout the years. In 2005, cancer drugs represented 12 percent of the direct costs, and this number increased to 31 percent in 2018. This is a large increase, but it is a bit overestimated as these numbers do not take into account confidential rebates that pharmaceutical companies grant to health care payers. There is some evidence that the size of these confidential rebates has been increasing over time as well.
The increasing size of expenditure on cancer drugs is not surprising. Between 2005 and 2018 we saw the regulatory approval of a whopping 99 new cancer drugs by the European Medicines Agency. Treatment with newer and effective drugs has become standard of care in many cancer types during this period. More cancer patients, who previously had no treatment option left, have now access to valuable drugs. New drugs are also increasingly being used in an adjuvant treatment setting instead of only in the metastatic setting. Thus, increases in the number of drugs available and the number of patients treated are developments to keep in mind when you look at the increasing expenditure on cancer drugs.
We also do not foresee an end to this development in the near future. There is a lot of money being spent on research of cancer drugs currently.
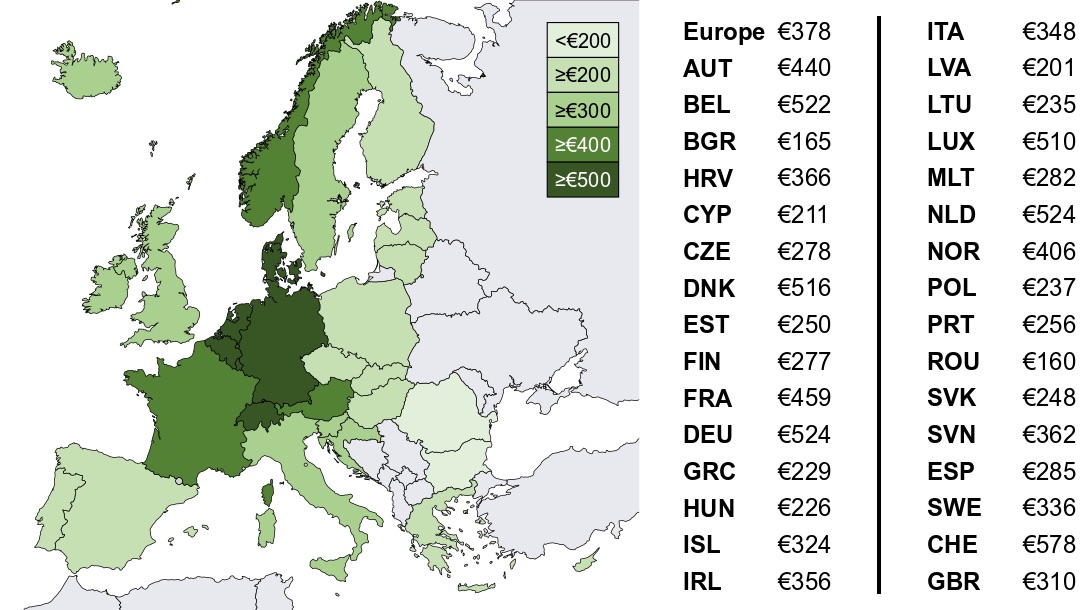
Q. Fig 3 in your paper seems very informative: would you like to comment it and define the take home message of your paper?
A. This figure summarizes the total cost of cancer, the sum of direct costs, indirect costs, and informal care costs, in every country. It really shows how much of a burden cancer is to society. In total we are talking about €199 billion in Europe in 2018. On the country level, the total costs ranged from €160 per capita in Romania to €578 per capita in Switzerland. Typically, costs are lower in Eastern and Southern Europe and highest in Central Europe. This reflects both more spending on cancer care and high productivity loss due to a higher labor market participation in the latter countries.
This study puts concrete numbers on the table that quantify the economic burden of cancer. Information on the total cost is essential for documenting value for money and potentials for improved patient outcomes through cost-effective spending. The massive differences in health care spending on cancer care between European countries are worrisome, because it indicates that patients do not have equal access to high-quality cancer care.
About the author
Thomas Hofmarcher is a health economist with a strong focus on policy-relevant analysis. He is an expert of cost-of-illness analysis, patient access studies, cost-effectiveness analysis, budget impact analysis, market forecast models to the application of advanced econometric methods in both Swedish and European contexts. Cancer is the disease area he has worked most with.