Brazilian surgeon Angelita Habr-Gama changed the way that lower rectal cancer is treated when she discovered that many patients treated with neoadjuvant chemoradiation for early rectal cancers showed no residual disease and yet were still undergoing abdominal perineal resections. She proposed a ‘watch and wait’ approach, and showed that it is safe to restrict surgery to those still showing evidence of disease following neoadjuvant treatment. Thousands of people have been spared unnecessary surgery-related sexual, urinary and bowel dysfunction thanks to this strategy.
Habr-Gama’s seminal 2004 study, comparing operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation, was the only Latin American work included in the 100 most cited works on surgery compiled by the World Journal of Surgery in 2018. Now her contribution to the development of medical science has been recognised by Stanford University, who has included her in the latest update of their prestigious rankings of the 2% most cited scientists in various disciplines.
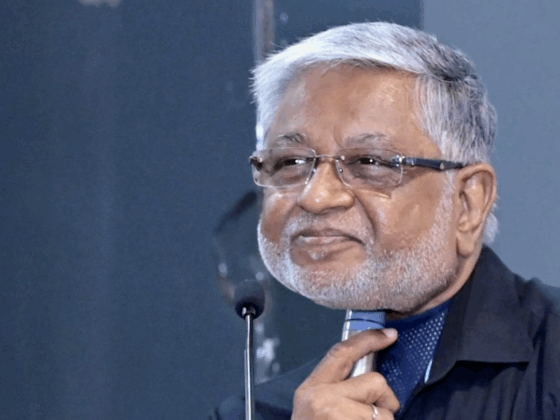
In an exclusive interview with Cancerworld, Angelita Habr-Gama, who was the first woman in her country to be admitted as a fellow at a school of surgery, discusses what her work has delivered for patients, how the gender balance in surgery has changed, and her hopes for cancer research in Brazil..
Cancerworld: The suggestion that some patients with early rectal cancers could be treated without surgery was quite a radical proposal. How did that idea come about?
Angelita Habr-Gama: Surgery for rectal cancer is a difficult intervention, and the lower the location of the tumour, the more complicated it becomes because it may involve removing the sphincter, permanent colostomy and other difficult decisions. In order to improve results and reduce recurrences, the chemoradiotherapy protocol started to be used soon after diagnosis and before surgical planning. With neoadjuvant chemoradiotherapy, the operation often became more feasible. We observed that, in some cases with this approach, the tumour mass disappeared. This evidence led us to no longer operate on patients immediately. Thus the idea of observing these patients meticulously, at first every two months, was born. This strategy was designated as watch and wait.
CW: How much of a challenge is this meticulous observation?
A H-G: The most important thing is to keep the patient under strict follow-up. It is necessary to establish a relationship between doctor and patient. The patient needs to be informed that the tumour may come back and, if this happens, surgery will be required. In the first year, the patient is re-examined every three months, and then, according to the evolution, it is spaced out. Doctor‒patient commitment is essential for the success of this strategy, but it makes it difficult to apply on a large scale because it requires frequent monitoring – otherwise a recurrence will not be detected quickly enough.
CW: How did the scientific community respond to the watch and wait strategy you proposed?
A H-G: The acceptance of non-surgical treatment, like any innovation, generates controversy. When a myth is broken, first you are discredited, then you are accepted. Of course, there are opponents. Today patients discuss with their doctors much more, seeking more information about their treatment. They wonder why, if their tumour disappears after chemoradiotherapy, they are undergoing surgery. This strategy should not be considered as a non-surgical treatment, but as an immediate non-surgical treatment.
CW: How has the protocol developed since the first study was published in 2004?
A H-G: In the first protocol, with two chemotherapy cycles (5FU and leucovorin), 29% of patients had a complete clinical response and were not operated on. We gradually understood that, in terms of chemoradiotherapy, the results should be evaluated later, and we started to wait at least 12 weeks. We switched to the expanded protocol in 2006, and the number of complete responses has increased greatly, with no further toxicity occurring. The radiotherapy dose was slightly increased. We started doing three cycles of chemotherapy during the radiotherapy period, and now we do chemotherapy continuously during radiotherapy and beyond, for almost two months. With the expanded radiochemotherapy protocol, we observed more than 50% clinical complete response. This results in a very large number of patients who are not operated on, and it is a great satisfaction to observe the acceptance of this protocol, which was much criticised at the beginning. The recognition is extremely important for patients. We are increasingly improving surgical techniques, but it is still major surgery, which can generate dysfunction. Sometimes the tumour greatly decreases in size, without actually disappearing. In these cases, instead of radical surgery, we perform a local resection, with the same possibility of cure.

CW: In the 1950s you were the first woman to be admitted as a fellow at a school of surgery in Brazil. You were also the first Latin American physician and the first woman to join the select group of Honorary Members of the European Surgical Association. How do you see the growth of female participation in the medical career, especially in surgery?
A H-G: Surgery has always been an essentially male area, as has medicine. But there is nothing in any profession that prevents women from participating. Women study hard, they apply themselves, and the consequence is that the proportion of women who enter medical schools today is higher, reaching 60%. I think the fact that more women are entering surgery is a reflection of the greater number of women who graduate each year, do residency and conquer their space. But motherhood is still an additional challenge, especially in the area of surgery, which, in addition to intellectual activity, requires physical presence. Therefore, pregnancy can be a little difficult. I made a choice not to have children. And with that I was able to work on equal terms.
CW: How do you respond to your most recent recognition, ranked among the 2% most cited scientists in your discipline worldwide?
A H-G: I was very surprised. I had already received a placement among the 100 researchers with the most cited works in the surgical scientific literature. Now, this position among the 2% most cited scientists in the world is very opportune, because it comes at a time when we have several problems in Brazil, with some young talents leaving the country. So I think this is an opportunity to show that, despite the difficulties we face doing research in Brazil, where there is not much, it is possible to publish important works and have new ideas respected by the international scientific community. It is a stimulus for youth, showing the strength of study and work.
Sergio Azman co-reported this interview.