“I was told that cancer was a temporary condition ‒ just get through treatment and things will go back to normal. I quickly realised that this is not true.”
Gregory Aune was treated for Hodgkin’s disease when he was 17. That treatment ‒ eight chemotherapy agents and a heavy dose of radiation ‒ saved his life and allowed him to pursue a successful career in medicine.
But the price he pays in long-term effects is quite sobering: hyperthyroidism; pulmonary fibrosis; infertility; aortic stenosis; 3-vessel coronary artery disease, all blocked by >95%; secondary skin cancers; stroke/transient ischaemic attack; diabetes; congestive heart failure; pulmonary hypertension/mitral valve disease.
Now in his mid-40s, and a professor of paediatric medicine at San Antonio, Aune says he is not looking for sympathy. He is looking for recognition. Recognition of the scale of problems that many cancer survivors live with as a consequence of their disease and treatment. Recognition of the gap in planned and coordinated care for this large and growing population, and of the gap in reliable information about their needs. Recognition of the gap in research dedicated to understanding long-term and late effects, what causes them, and how they can be predicted, prevented or managed. And ‒ a particular focus ‒ recognition of the ethical imperative to change the way new cancer therapies are developed, so that potential late-effects are investigated at a preclinical stage, rather than letting them enter clinical practice and just waiting to see what might happen to patients like him, 10, 20, 30 years down the line.
“We must incorporate off-target organ effects into early development of new cancer therapies,” he says.
Aune was speaking at a session on the Science of Survivorship, organised at the end of June by the American Association for Cancer Research, under the auspices of its Scientist↔Survivor Program.
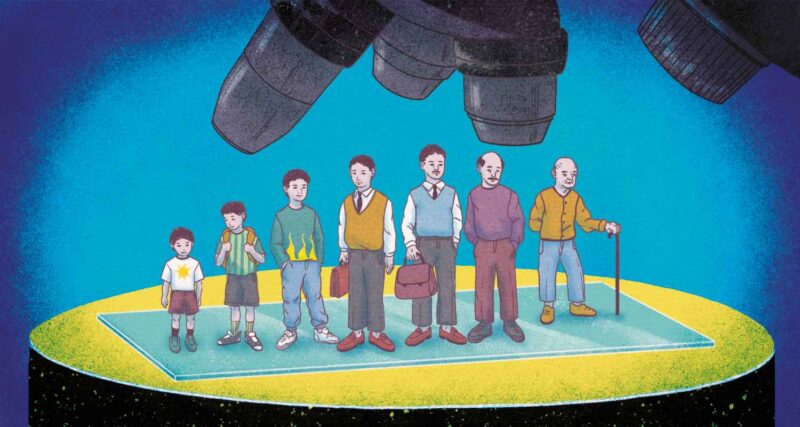
The headline statistics underpinning the session were ones that are familiar to many in the cancer community: In 1971, when President Nixon signed the US National Cancer Act, there were around three million cancer survivors. Today there are 18 million ‒ that’s more than the entire population of the Netherlands. Almost 50% of people diagnosed with cancer in the US now live for at least 10 years.
These statistics tend to be cited as evidence of the progress made in treating cancer, and to galvanise efforts to extend survival times still further.
But in this session, the focus was on the 18 million survivors, and on the gaping hole in knowledge about how their lives ‒ their health and psychological, social and economic wellbeing ‒ have been impacted over the longer term by their cancer diagnosis and treatment. It was on the urgent need to fund a coherent research programme to understand the scale and nature of long-term problems, in order to better prevent, monitor and manage them. Crucially, it was also about the role for survivors themselves, in generating ‘real world evidence’, by reporting the issues they face, and defining their unmet needs for support and care, and their priorities for research.
What it was not about was pitting the needs of people with better prognoses against those for whom survival remains the overriding issue, as Adam Hayden, an advocate with the AACR Scientist↔Survivor Program, made clear. Hayden was diagnosed almost seven years ago with an aggressive brain tumour that carries an average life expectancy of no more than two to three years. The need to develop durable therapies is hugely important, he says, “But sometimes there is so much focus on the newly diagnosed or newly recurred, that people like me, who have lived with this for seven years, are forgotten about.”
‘See you next scan’
A researcher at the department of philosophy at Purdue University, Indianapolis, Hayden has found his analytical skills helpful in making sense of what he is going through. His description was a great illustration of the ‘real world’ insights that will be so important to improving care and support for survivors.
First up, the emotional/psychological whack that goes with a brain tumour diagnosis makes the offer of psychosocial support essential right at the start. It’s not just about the prognosis, it’s about what happens to your confidence and your identity when the body you took for granted starts behaving in unpredictable ways. Then just as you have greatest need for friends and family, those relationships get disrupted, which can bring an added burden. “After illness, all experience becomes cast in the shadow of illness. People behave differently. The emotional distress is an existential weight on the shoulders of survivors. You are no longer the person family and friends thought. You are that plus cancer.”
“I had to go and find a mental health professional,” said Hayden. “That should be automatic because all of our relationships have changed. Many cancer centres offer access to mental health counselling, but we don’t access it early enough. It should be right at the start.” (Hayden also points out that a more constructive alternative to the question, “You do know you are going to die with this?” might have been used, at the point of diagnosis, if greater priority had been given to the quality of his survivorship, and to helping him find the best way navigate the years ahead.)
Another pressing need for people in his position, says Hayden, is information and guidance about what is happening with his disease and what he can do to help his own health and wellbeing. “See you next scan,” is how he refers to this set of issues. At a general level, he’d like better coordination between the actors involved in different aspects of his care, and to feel that there is joined-up oversight across all the health and wellbeing aspects that matter to him.
He would like evidence-based advice, for instance, on how to supplement his health, that goes beyond the standard “eat a healthy balanced diet”. He’d like more evidence on the long-term toxic effects of the gadolinium injected into him as a contrast enhancer for his regular MRI scans. Having survived seven years now, he’s had more than 30 doses – is it still the best option for someone in his position?
Above all, anything that can throw light on how his disease is likely to progress, about timelines, is a priority, and he finds it frustrating to get so little feedback after his scans. “Am I in remission? How do I plan? I would have planned differently if I knew I had six more years. What do I plan for now? We need an ongoing prognosis conversation to help with life planning.”
Turning experiences into evidence
For Patty Spears, a fellow patient advocate with the AACR Scientist↔Survivor Program, the testimony Hayden gave about the challenges he faces as a glioblastoma survivor, and of his priorities and unmet needs, provides essential building blocks in developing the science of survivorship.
Assembling those building blocks from across the full spectrum of patients and cancers, she believes, will require the integration of patient reported outcomes (PROMs) into routine clinical care. Not just during the treatment and follow-up period, but along the patient’s entire lifespan. And not restricted to a set of pre-selected symptoms, but capturing data on all health, psychological and socioeconomic issues. “We need to capture all long-term effects.”
More tailored and sophisticated apps are lightening the burden of such reporting, says Spears, who is herself a breast cancer survivor, and works as a Research Manager at the Patient Advocates for Research Council, at the University of North Carolina’s Lineberger Comprehensive Cancer Center. Conducted effectively, she argues, many patients see the benefits, quite independent of their research value. “Patients question everything that happens after treatment. They fear what will happen once treatment ends,” she says. “PROMs are really useful to tell doctors about experiences, and PROMs conversations can help better manage side-effects.”
Questions of how it might be possible to mine such data to get a full picture ‒ harmonisation, storage, security, access ‒ are of course currently the focus of intense discussion across the medical research world. But you can’t mine what you don’t gather.
Her hopes are that the evidence gathered in this way could be quickly put to use to improve the care of survivors. If you can predict the sorts of issues any given patient is likely to face, that enables clinicians and patients to monitor the progress of side effects that persist beyond treatment, to watch out for late effects that might arise, sometimes long after treatment ends, and to plan for coordinated delivery of the right support and care.
Spears finds it frustrating that even the evidence currently available is not reaching the people who need it most. This year, 23 years after being diagnosed and treated for locally advanced breast cancer, Spears found out she had a primary liver cancer.
Despite her long involvement as a patient advocate with a number of cancer research councils and networks, this new diagnosis took her completely by surprise. For many weeks she assumed the pain she was feeling was probably a gallstone complaint ‒ something that runs in the family. Only after an MRI scan revealed the liver cancer did she learn that liver primaries 20 years after breast cancer treatment are not so unusual.
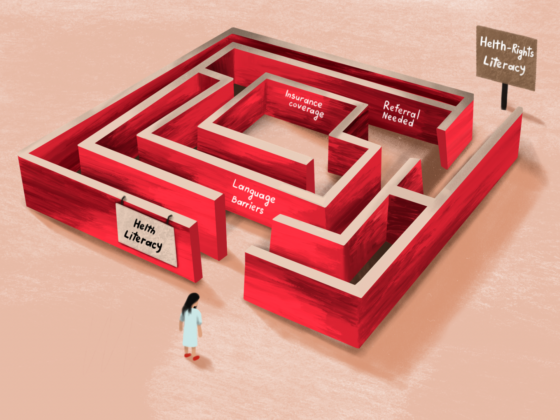
“Why did no one talk to me about long-term effects before, or even after treatment?”
“Why did no one talk to me about long-term effects before, or even after treatment?” she asks. “The focus was all on acute effects. You are not really told what [long-term effects] to look for. This information is not given to patients. We need to say that is important to talk about. Even the basics are not being done.”
She would also like to see much greater efforts to understand the causes, as a step towards preventing ‒ or at least predicting ‒ this late effect. “We should make an effort to ask the question: Where did this liver cancer come from? Is it my genes? If you can learn from patients like me, you can predict at an early stage and you know what to look for.”
Doing the science
Finding answers to questions like that one, regarding the biological mechanisms behind clinically observed potentially life-threatening late effects, is a priority for Gregory Aune. He can’t see it happening on the scale that is needed, without a strategic policy decision to direct more support into survivorship research.
Having himself undergone replacement of his aortic valve and triple bypass surgery at the age of 35 ‒ “like going through cancer all over again” ‒ he now focuses his own research work on exploring the mechanisms of cardiac toxicity associated with anthracycline treatment ‒ the drug class that he says causes the most problems. “Over half of paediatric patients treated with anthracycline get cardiotoxicity, often with a 20-year latent period. There is not much research into the mechanism. We need to go back and reinvestigate how these old drugs do this damage,” he says. “Chemotherapy will be needed for a long time to come.”
The damage from “old drugs” he accepts is a legacy from the days when “regimens were decided by trial and error with no understanding about how they affected other organs.” But as he points out, new tools are now available that make it possible to explore those effects during the early, preclinical stage of developing new therapies. He regards it as “almost unethical” not to use them.
“We need to go back and reinvestigate how these old drugs do this damage”
New classes of drugs such as immune checkpoint blockade and antibody-drug conjugates are known to impact ‘off-target organs, and yet they are being introduced, even in an adjuvant setting, without trying to understand the mechanisms involved.
He agrees with Spears on the vital importance of gathering long-term data, and has himself established a cohort of long-term survivors of paediatric cancer, for this very purpose.
The Scientist↔Survivors’ ask
The essence of AACR’s Scientist↔Survivor program is that, when survivors and scientists work together, they can help ensure a better life for millions of people living with and after cancer. But ‒ and this is the headline ask ‒ it will require those who shape the cancer research priorities, shape the infrastructure and allocate funding to put survivorship much higher up the agenda.
It will require a national effort to establish cohorts for all cancer types to gather long-term clinical and PROMs data along the lines of the one that Aune has set up for paediatric cancers ‒ and the political will to overcome all the legal, ethical and funding issues and barriers from vested interests that continue to hamper data sharing.
And it will require recognising how the challenge of cancer has changed since the National Cancer Act was signed more than 50 years ago. Finding ways to prevent and predict, and to monitor and manage, lasting and late effects of treatment must now become a research focus in its own right. A journal and an annual meeting dedicated to preclinical survivorship research, together with its own funding streams, and ideally its own institute ‒ the 38th US National Institute of Health ‒ is something Aune has been advocating for the past decade.
Then there are questions about what, if anything, can be asked of pharmaceutical companies. They won’t want anything that involves following up patients in the long term, was the feeling, but what about the preclinical work? Should regulators require data that might predict lasting or long-term impacts on off-target organs that might not become apparent during the course of the clinical trials? Should companies be obliged to share data that could be of concern for lasting or long-term effects?
And finally, the question of the bottom line – how do you convince the funders? Just do the sums, was the unanimous view of the panel. Preventing lasting and late effects in this huge and growing population, predicting them better, detecting them earlier, managing them more effectively makes economic sense. It saves healthcare costs, it enables survivors to stay economically active, and avoids carers having to leave work to care for dependents.
Factor in some of the more common lasting effects ‒ pain, fatigue, impaired immune function, anxiety and other mental health issues ‒ and the scale of the problem becomes clear. Then remember the size of the population ‒ larger than that of the Netherlands and rapidly growing, and that two in five are younger than 60, and that the risk of bankruptcy is 2.5 times higher among survivors than the general population.
Add that all together and the funding ask from the Scientist↔Survivors’ panel might begin to look quite reasonable. As might the demand that cancer research should integrate a long-term perspective into its investigations of new therapies.
Illustration by: Sara Corsi