In Africa, women’s infertility carries a heavy stigma; it becomes their label. Many end up feeling worthless, face harsh treatment from in-laws, abandonment by spouses, or relegation to polygamous marriages, as husbands take additional wives capable of bearing children.
For Linet Auma, a 27-year-old recently diagnosed with HER2-positive breast cancer, the fear of losing her ability to have children compounds the distress of her diagnosis. “The cancer diagnosis was shocking enough, but even more disheartening was the thought that I might never have children,” she says.
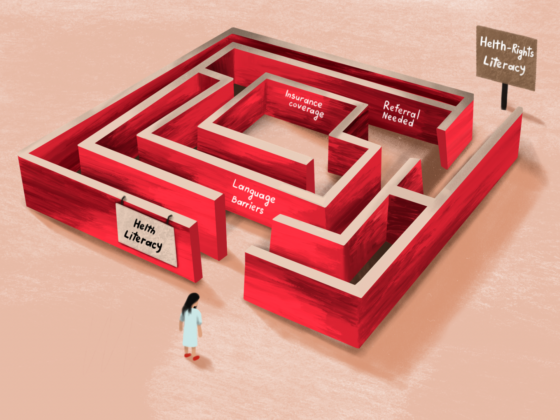
Auma says she only learnt about the damage caused by chemotherapy when the oncologist referred her to a fertility specialist. “He [the fertility expert] started by saying that I needed to freeze my eggs immediately to improve my chances of having a child in future. I didn’t even know what egg freezing entailed, let alone IVF [in vitro fertilisation],” Auma recounts tearfully.
“I went home and the first thing my mother asked was how much it would cost. I didn’t even bother to open the consent forms that the specialist sent me. I didn’t see the need to. We simply can’t afford it.
“My mum is struggling to get money for my cancer treatment, and she also worries about the possibility of lacking social status that comes with being a grandmother, she cannot afford to pay for my egg freezing,” says Auma, who is an unemployed graduate.
The 27-year-old is on a combination of paclitaxel, pertuzumab and trastuzumab, with a mastectomy and subsequent radiotherapy planned. “I don’t know if the chemo drugs have already destroyed my eggs. But I have seen women get children after chemo, so I’m optimistic,” she says.
Egg or ovary tissue freezing is very expensive – around three times the average per capita household income
The option of preserving fertility by having their eggs collected and frozen before chemotherapy is one that is not open to the great majority of African women, like Auma. In Kenya, for instance, there are fewer than 20 fertility clinics, most located in Nairobi, and egg or ovary tissue freezing is very expensive. The initial cost of egg freezing alone is around US$3,100, with an additional US$2,400 required upon completion of the process – that is around three times the average per capita household income of US$1,760.
However, a treatment already in use in the West to guard against chemo-induced early menopause is now being studied in a Kenyan patient population, with a hope that, by preserving ovarian function, it can increase the chances of successful pregnancies after cancer treatment. This treatment is goserelin, a gonadotropin releasing hormone (GnRH) agonist that blocks the hormones that trigger ovulation.
The goserelin study
Abeid Athman Omar, a clinical oncologist at Kenyatta University Teaching, Referral and Research Hospital, in Nairobi, says goserelin offers hope in addressing fertility preservation in low- and middle-income countries such as Kenya, where the egg freezing costs are too high and fertility clinics and specialists are few.
“Zoladex [goserelin] injection works by temporarily shutting down the ovaries, but only during the period of cancer treatment, akin to putting the ovaries in a state of hibernation. This pause protects the eggs, and after treatment, normal ovulation can resume, potentially allowing women to conceive,” he says.
Treatment-induced amenorrhea is common in breast cancer patients, but available data shows a majority of the women treated with goserelin before and during chemotherapy tend to resume normal menstrual cycles within six months, says Omar. “We have very few patients who can go up to two to three years because human beings are not the same, but we know that six months is ideal,” he adds.
“It’s an available option to… potentially improve future fertility in premenopausal patients with early breast cancer”
Evidence for the efficacy and safety of temporary ovarian suppression with GnRH agonists during chemotherapy, based on a systematic review and meta-analysis of individual patient–level data, was published in the JCO in 2018. The authors concluded that, “It’s an available option to reduce the likelihood of chemotherapy-induced POI [premature ovarian insufficiency], and potentially improve future fertility in premenopausal patients with early breast cancer.”
Although goserelin is used in other countries, its effectiveness for Kenyan breast cancer patients remains undocumented. Omar is conducting an observational study to assess goserelin’s efficacy in preserving fertility for Kenyan women, with guidance from Matteo Lambertini, an oncology consultant at IRCCS Policlinico San Martino Hospital, in Genova, Italy, who specialises in managing fertility and pregnancy-related issues in women with breast cancer, and was lead author on the JCO meta-analysis. The study aims to compare the outcomes with global findings, and may pave the way for broader use of goserelin if proven beneficial. “This is just an observational study,” says Omar. “We already know that this treatment has worked in patients in the West.”
Before the formal study, Omar had already been prescribing goserelin to some of his patients, in monthly injections of 3.6mg for six months. However, his patients said they preferred having fewer injections with higher doses, which they found more affordable and easier. The study protocol therefore uses two doses of 10.8mg administered three months apart. “We are targeting women under 40 because many of them have not yet completed their families,” he says, “We want to see if the two doses are sufficient.”
The study plans to recruit only 25–50 patients a year, due to budget constraints and the limited number of eligible participants. “We’re piloting it at our hospital. Then maybe we can extend it to a national study, if we have enough funds to support us,” says Omar.
Fertility preservation: a major unmet need
As Omar notes, the topic is particularly pertinent in the region due to the increasing prevalence of breast cancer in younger women in Africa compared to the West, with around one in four cases in Kenya diagnosed before age 40. Across Sub-Saharan Africa as a whole, the peak incidence of breast cancer diagnosis is around a decade earlier than in the United States. Unfortunately, many are not told of either the potential threat to their fertility or possible mitigation strategies, at the time they are started on treatment.
Omar believes that one reason so many oncologists are failing to provide this information comes down to time constraints. Despite international guidelines recommending fertility discussions for young cancer patients, such counselling is often overlooked due to the high patient load, he says.
“Fertility counselling can take a minimum of 30 to 40 minutes. If you have 50 patients waiting, it is very difficult for you to counsel”
“There was a survey, conducted by Dr Lambertini, which included many African countries. He was looking at the knowledge and awareness of these doctors in oncofertility. Most of the doctors said they are aware, but the main problem is, they don’t have time. We have very few oncologists serving patients, and fertility counselling can take a minimum of 30 to 40 minutes. If you have 50 patients waiting, it is very difficult for you to counsel,” he says.
“Like at my clinic, people sometimes complain that I spend a lot of time with patients. I do fertility counselling for all my breast cancer patients. I don’t assume just because a patient has two, three, or five children, she doesn’t want a bigger family,” he says. He wishes Africa could have the sort of dedicated oncofertility clinics that are increasingly common in Western countries, where he could send patients. “This can help me as a physician to see more patients.”
Impaired fertility from chemotherapy is also a problem for women over 40 and with other types of cancer.
Sharon Kemunto, a 40-year-old with hormone receptor-positive breast cancer, faces the same dilemma of fertility preservation. Despite already having two children, she desires more, but she was not informed about her options before starting treatment.
“I got remarried and then boom! I was diagnosed with Stage 3 breast cancer,” she says. “The doctor was in a rush to start me off on chemotherapy, radiotherapy and mastectomy.
“I know I’m lucky that the hurried treatment may have cleared the cancer, knowing that some patients take years, but you know how African culture is like. My in-laws have started asking when I will give my husband a child. I laugh off the conversation and say, ‘soon’. But I don’t even know if I will ever have a child. I’m very stressed,” she says.
Sharon and her husband have children from past relationships, but the mother of two teenage girls says, “I must give my husband a child. A boy mostly.”
“My in-laws have started asking when I will give my husband a child. I laugh off the conversation and say, ‘soon’. I’m very stressed”
Sharon says her husband, who left his first wife with children, has also started asking why she is not getting pregnant. “My husband asked when I would get pregnant. He doesn’t know that chemotherapy may have affected me… I cannot tell him,” she says. “Had I been asked to choose between treatment and starting a family with my new husband, I’d have picked the latter. I’d have conceived, gotten a baby, then resumed treatment to save my life.”
Sharon is now on her second year of taking tamoxifen, with three more to go. She is sticking to the medical advice not to try to get pregnant while on the hormonal drug, but she worries that waiting three more years will narrow the window of time in which she can try to get pregnant. She would welcome some reliable information on her options.
“If someone could tell me that I can safely temporarily stop this hormone therapy and conceive, I will do it without blinking,” she says.
Fertility pathbreaker
Khadija Warfa, an obstetrician-gynaecologist and a gynaecologic oncologist, underscores the critical need for early fertility discussions. “We have patients who have finished chemo and radiation, and they ask about fertility, and you are left wide-eyed wondering why it wasn’t discussed before the treatment started,” she said, during the second East Africa Oncology Summit held in Nairobi on June 22, 2024.
Omar is optimistic about the potential impact of goserelin as a fertility preservation pathbreaker for young breast cancer patients. “If it shows positive influence, oh yes, definitely. It will boost confidence in our women and give them hope. Even though it’s a small study, we believe the impact will be very high,” he says. “Some developed countries are using goserelin as a second option. But here in Kenya, it might become, like, the main option,” he adds.
If the study indicates Kenyan women could benefit, wouldn’t it require oncologists in Africa to be trained to offer that option? Even in Europe, where a range of fertility preservation options have been available for decades, some breast oncologists fail to have that discussion with their pre-menopausal patients.
Africa is making strides in oncofertility, says Omar, supported by organisations such as AORTIC, the African Organisation for Research and Training in Cancer. Omar’s own work represents a crucial step toward bridging the gap between the quality of care in Africa and the West, offering young women facing cancer a chance to maintain their ovarian function and fulfil their dreams of motherhood in the future.
Historically, in Africa, cancer has been seen as a death sentence, he adds. “So, most women, when they come with a diagnosis of cancer, they don’t think that they are going to survive that long to be able to have children. Unless you, the oncologist, start this discussion and take her through the treatment journey, make them optimistic.” It’s a conversation that matters immensely to the great majority of women who have not yet reached menopause, he stresses. “I have come to realise almost all women want to preserve their fertility.”