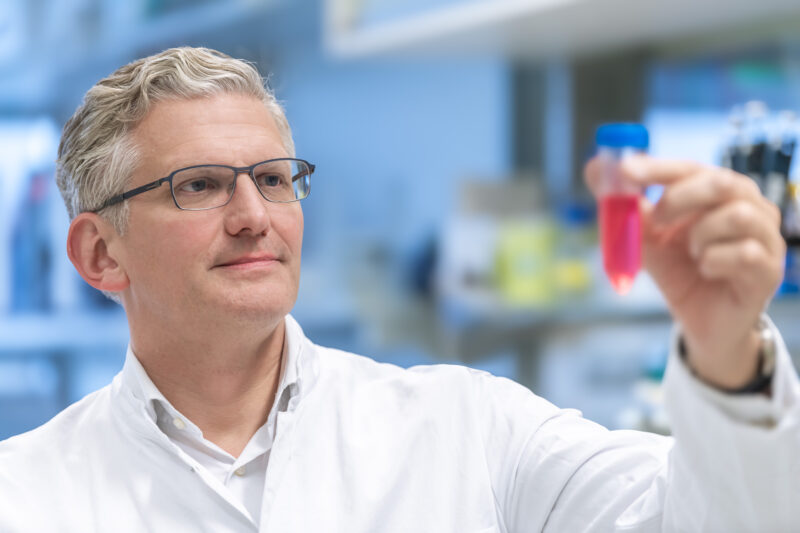
In May 2025, neuroscientist Frank Winkler, together with neurooncologist Michelle Monje, received the Brain Prize for pioneering Cancer Neuroscience, a discipline that explores how neurons actively contribute to tumor growth. How are nerve and tumor cells interacting, and how could this insight lead to new therapies?
Cancer neuroscience emerged not from a classic eureka moment, but – like so often in science – from an observation that made little sense. Looking at the image captured by electron microscopy together with his co-worker Varun Venkataramani and the neuroanatomist Thomas Kuner, Frank Winkler first thought he’d spotted a fluke. “We knew that tumor cells can form thin, long extensions similar to neuronal axons. That day, we saw synapses on these tumor microtubes”, Winkler says to CancerWorld. “Tumor cells sometimes behave weirdly. So, we thought, fine, this tumor cell is just being strange and forms a synapse with another tumor cell”. But then the German neuroscientist, now at the University of Heidelberg in Germany, decided to look more closely. “Synapses always formed in the same way, between neurons and tumor cells: Neurons presynaptically, where a signal is sent, and tumors postsynaptically, where the signal is received. Now that looked suspiciously like a biological function.”
Still, Winkler and his team were trying to make sense of their discovery – and to understand if their finding was an artifact or biological reality. The turning point happened in 2015, when Winkler met fellow neuroscientist Michelle Monje after a lecture. Not being able to hold back anymore, they went back and forth. “We found something crazy!” – “No, Frank, let me tell you, we found something crazy.” “After a few minutes of discussion, we realized that we both had found the same crazy things: Tumor cells instruct neurons to form synapses with them, and these synapses are not just structures. They are functional and indistinguishable from synapses formed between neurons”, Winkler recalls.
This year, Frank Winkler and Michelle Monje were recognized for pioneering the field of Cancer Neuroscience with a joint award of The Brain Prize, the most highly endowed award for neuroscience. Ten years ago, however, the neuroscientists found safety in numbers. “We quickly decided to collaborate closely, culminating in our articles being published back-to-back in Nature in 2019. For me, this collaboration underlines how science should work”, Winkler remembers. “In addition, sometimes scientific findings turn out to be incorrect and are retracted later. But if two independent research groups publish the same unusual finding, it adds credibility: The result is likely real and not merely an artifact of specific models.”

Indeed, their findings and follow-up research have changed our understanding of tumors. “Tumors used to be thought of as something foreign, something chaotic, that doesn’t belong and only disrupts an organ”, Winkler adds. “Instead, tumors are able to interact with the nervous system and can even, within their networks, autonomously perform nearly intelligent operations.”
But how did a neuroscientist come to co-drive a new field of cancer research? “I have always been fascinated by the big challenges and difficult questions. As a neuroscientist, I became quickly interested in brain cancer and during my time at Harvard, I focused on brain tumors”, Winkler recalls. “There, I learned intravital microscopy, a technique I brought back to Germany when I established my own lab in Munich and later Heidelberg. Backed by this technical angle, I brought a strongly neuroscientific view to cancer: I was trying to understand what a tumor is doing within the brain.”
Moving Beyond the Brain
Winkler and colleagues first identified neuron-tumor synapses in glioblastoma, a highly aggressive brain tumor, in which neuron-tumor synapses drive tumor growth and brain invasion. But further research showed that neurons and tumor cells form synapses not just in brain cancer, but also in brain metastases. Neuron-tumor synapses were found in brain metastases from breast cancer, lung cancer, and melanoma – indicating that very different types of tumor cells can become postsynaptic partners.
Whether such synaptic connections form only within the brain or also outside, in extra-cranial tumors, remains an open and intensively studied question. While studies by several groups are ongoing, no clear evidence is published yet. “Our own initial data points towards neuron-tumor synapses being a generalizable principle across tumor types”, Winkler notes. “Given that nerve endings are found throughout our body, I’d be surprised if synapses were restricted to the brain.”
Tumors are well known to be innervated, and many tumor types are more densely innervated than their tissue of origin. Already in 2001, co-cultures of mouse neurons with prostate cancer cells showed that neural processes extend towards cancer cells actively and stimulate cancer cells’ growth. Nerves are not simply bystanders, but instead are functionally affecting tumorigenesis – though the exact relationship may depend on both the tumor and the neuron type. “Innervation by the sympathetic nervous system often drives tumor growth, while innervation by the parasympathetic nervous system, when strongly activated, can slow growth”, Winkler summarizes. “But how does this work?”
New Therapies: A Long Road Ahead
Understanding the mechanism how neurons can fuel tumor expansion in some contexts could help develop targeted, specific therapies. As a clinician, Winkler is cautious not to overstate the potential impact of therapies based on cancer neuroscience. “Just because the concepts are exciting and the biology is tremendously fascinating, doesn’t automatically mean that patients will benefit from a neuroscience-instructed cancer therapy.”
Several therapeutic strategies are currently being explored, especially for glioblastoma. The key for developing an effective therapy is to alter the interaction between neurons and tumors, while not harming the normal, non-diseased nervous system. Winkler himself leads a Germany-wide clinical trial investigating the use of perampanel, an AMPA-receptor antagonist, against recurrent glioblastoma to investigate whether the repurposed drug – perampanel is normally used to treat seizures – can slow tumor growth. “Showing an effect in patients is the next major step for cancer neuroscience, and we – and others – are now testing this completely new therapeutic principle in both brain cancer and other tumor types.” As the nervous system, immune system and cancer cells all influence each other, additional benefit could arise from targeting this triangle.

Collaboration is again key. “Researchers across the field of cancer neuroscience are now coming together to lay out which conceptual hurdles we still need to take, which trials are needed, and which data we need to collect.” The goal is to develop the field quickly, with informative and well-designed trials. Winkler says he learned his lessons from observing the previous emerging field in cancer therapy. “For decades, researchers said that the immune system would fight cancer, but the studies continued to be negative, so much that proponents weren’t taken seriously anymore – until, of course, the amazing breakthrough of checkpoint inhibitors. With cancer neuroscience, we hope to avoid this fate and deliver benefits quickly.”