Small extracellular vesicles secreted by the hearts of mice with myocardial infarction accelerated the growth of lung cancer tumours already present in the same mice. The study, published online in Circulation, 15 March, found that the cardiovascular drug spironolactone reduced both the number of vesicles produced and resulting tumour growth.
“We showed for the first time that the diseased heart secretes small extracellular vesicles that contain thousands of different factors. These bubbles directly promote the growth of certain tumours and also modulate the immune system, making the body more vulnerable to tumour growth,” says Jonathan Leor, the lead author, from Tel Aviv University and Sheba Medical Center.
The association between heart failure and cancer has been attributed, at least in part, to shared risk factors (such as smoking, obesity, diabetes, and hypertension). However, recent mechanistic studies have suggested a more causal explanation, with circulating factors released from injured hearts accelerating tumour growth independently of risk factors.
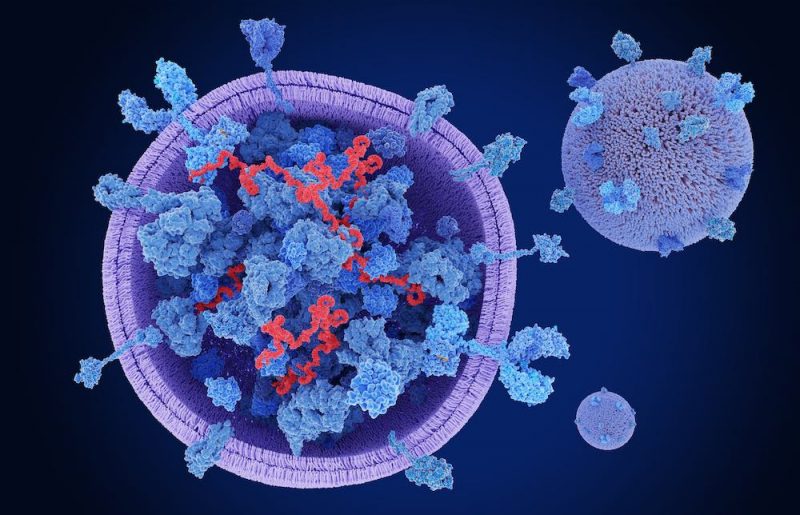
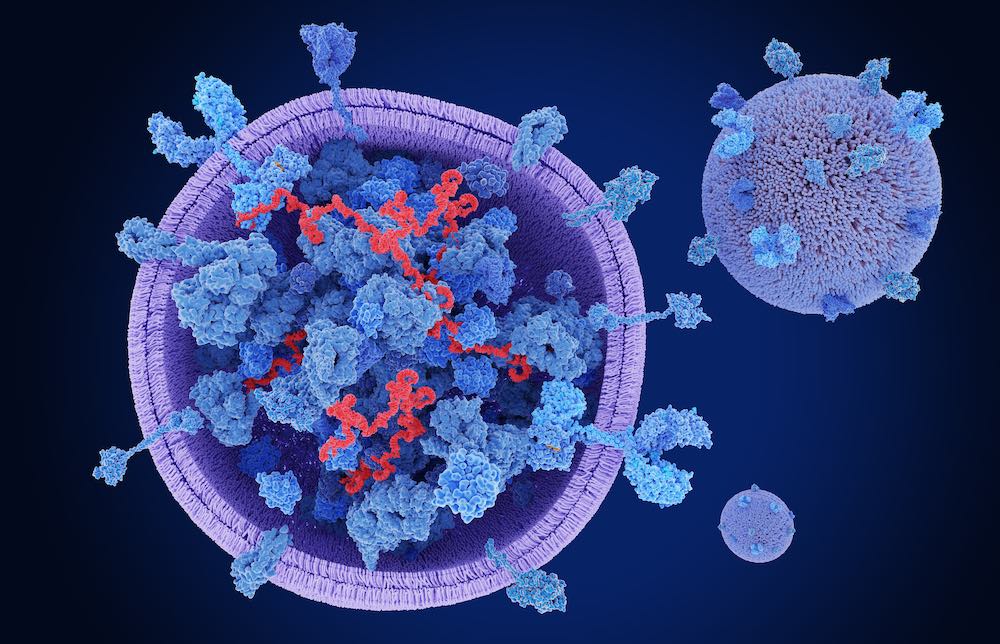
In a previous study, published in Circulation in 2021, Leor and colleagues demonstrated that small extracellular vesicles (sEVs) from human epicardial fat (fat covering the heart) carry pro-inflammatory, pro-fibrotic, and pro-arrhythmogenic factors that precipitate atrial fibrillation (a heart condition causing irregular heart rates). This work led Leor to hypothesise that sEVs from injured hearts might also play a role in the link between cardiovascular disease and cancer. Recently, sEVs – lipid-bound vesicles that are secreted by every cell in the body – have emerged as a new and powerful mechanism of communication between cells and their environment, through their ability to transmit multimolecular biological messages. sEVs, measuring <200 nm, are known to carry multiple factors (including proteins, nucleic acids, and lipids) involved in paracrine, endocrine, and autocrine roles, as well as pathological processes.
To undertake the current study, the team generated mouse models that could include both myocardial infarction (MI) and implanted lung cancer. Some of the mice were subjected to ligation of a coronary artery (mimicking MI), while others underwent a sham procedure (controls). The implanted cancers could be either orthotopic (where tumours were implanted in the lungs) or heterotopic (where tumours were implanted in different locations). “The orthotopic model allows us to assess the tumour in the context of its microenvironment; while the heterotopic model is more isolated and looks at the impact on cancer cells,” explains Tal Caller, the first author, who is an MD PhD student at Tel Aviv University and Sheba Medical Center. The study focused on sEVs secreted 10 days post MI. “This is a stage involving the resolution of intense inflammation with many similarities to cancer pathogenesis,” says Caller.
First, they showed that mice with both orthotopic and heterotopic transplanted cancers, who also had MI, had 1.5 times the growth of tumours cells in comparison to control mice with transplanted cancers but no MI.
Next, they measured the number of sEVs secreted by the entire heart and by cardiac mesenchymal stromal cells (cells that play a role in cardiac remodelling) following sacrifice 10 days post MI. Using size exclusion chromatography (to isolate sEVs from other substances secreted by cardiac cells), the team showed that post-MI mice had double the number of sEVs compared to control mice.
The team used proteomic analysis to measure the specific content of sEVs, finding that MI mice had higher expression of growth factors, pro-angiogenic factors, and pro-inflammatory factors (including interleukin 6 and tumour necrosis factor alpha) than control mice. Additionally, sEVs derived from cardiac mesenchymal stromal cells in post-MI mice switched macrophages to pro-tumorigenic states, with pro-angiogenic, pro-inflammatory, and immunomodulating traits.
When they incubated sEVs from MI mice in vitro with specific types of cancer cells, they found lung and colon cancer cells both proliferated and migrated more, but there was little effect on aggressive breast cancer and melanoma cells. “This suggests that the effects of cardiac sEVs on tumour cells are probably also dependent on type of cancer,” Caller tells Cancerworld. Similar observations, Leor adds, have been observed in the clinic, where heart disease has only been found to be associated with certain types of cancer.
Finally, the team explored whether inhibiting the renin-angiotensin-aldosterone system (a hormonal system regulating blood pressure and fluid balance) would influence the effect of MI on cancer. “We hypothesised that if we effectively treated heart failure and reduced remodelling, we would reduce the effect of heart disease on the progression of cancer,” explains Leor.
Results showed post-MI mice treated with the aldosterone receptor antagonist spironolactone had reduced numbers of sEVs derived from cardiac mesenchymal stromal cells (down by 28%) and suppressed tumour growth in comparison to untreated post-MI mice. No such effect was found for control mice treated with spironolactone. While the spironolactone experiments provide proof of concept that they can affect the link, the team believe that there are likely to be more effective drugs.
“We conclude that cardiac sEVs, especially those secreted from cardiac mesenchymal stromal cells, carry multiple factors and uptake by cancer cells accelerates tumour growth and treatment with spironolactone reduces the accelerated tumour growth. Our results provide new insights into the mechanism connecting post-MI heart failure to cancer, with the possibility of pharmaceutical options to reduce this deadly association,” says Caller.
While the team did not directly test for a role of sEVs in initiating cancer, they believe that they are likely to have an effect. “We showed sEVs influence the tumour microenvironment, affecting factors such as macrophages and expression of programmed-death ligand 1 [PD-L1]. Such factors increase the chance of tumour cells escaping the immune system and have been associated with the initiation and development of cancer,” says Caller.
The next step, says Leor, is to reproduce the mechanistic results seen in the mouse models in human cardiac tissue. Currently, the team is collecting human samples from open heart surgery at the Sheba Medical Center, including heart tissue taken from patients with end-stage heart failure and those undergoing mitral valve repair (with healthier hearts). Comparisons of the tissue will enable them to explore differences in sEV production and also whether a range of different drugs deliver benefits. While Leor and colleagues focus their expertise on biological and molecular mechanisms, they ultimately hope to inspire clinicians to perform clinical trials.