Across Latin America, indigenous women experience the highest cervical cancer death rates in the region. Geographic, economic, and cultural barriers hinder their access to screening and treatment follow-up. Now, a group of researchers is trying to change that, by mapping the problem and involving the communities in their research and healthcare initiatives.
In 2017, after a year of evaluating a government healthcare initiative in an Indigenous community in Colombia’s Amazon, María Inés Sarmiento-Medina, a researcher at Fundación Universitaria de Ciencias de la Salud in Colombia, received an unexpected visit from the women she and her group had come to know. They asked them to check if their heavy menstrual bleeding was a sign of cervical cancer. Sarmiento-Medina agreed, on the condition that the testing program included Indigenous women’s active participation. “We want an intercultural dialogue, and for women to participate in the project, we are not going to do anything by ourselves,” Sarmiento-Medina told them.
For nearly a decade, the WHO has ramped up efforts to eliminate cervical cancer. In 2018, it issued a global call to action, followed by the launch of the Global Strategy for Cervical Cancer Elimination in 2020. By 2022, cervical cancer remained the fourth most common cancer among women worldwide, claiming nearly 350,000 lives. For indigenous women in Latin America, it is the leading cause of cancer deaths.
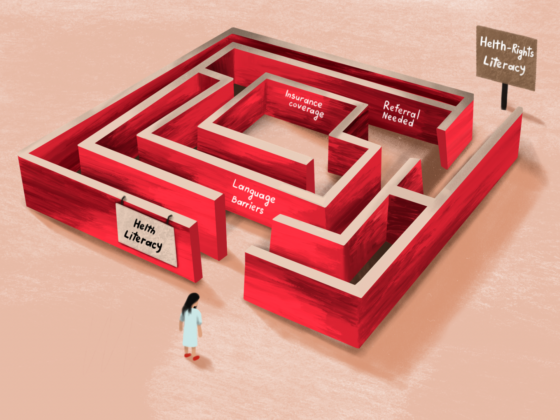
Women in these communities face persistent barriers to accessing prevention and treatment programs, including language differences, geographic isolation from health clinics, and cultural disconnects with healthcare providers. Although there is some isolated research on the epidemiology of these communities, there are still many gaps to be filled. “We don’t know what is happening,” said Diama Bhadra, a researcher at the Department of Obstetrics and Gynaecology, University of Campinas in Brazil. But some researchers like her are striving to change that.
Bhadra’s team recently published a systematic review of cervical cancer epidemiology among Indigenous women in the region. Their final analysis included 25 studies, most of which came from South America, with Brazil being the primary country conducting research, highlighting significant information gaps in Central America.
Researchers found HPV prevalence among Indigenous women to be over 30%, significantly higher than the global rate of 12% and nearly twice the rate in Latin America (16%), yet rates of high-grade precursor lesions (HSIL) were lower than expected. Since early detection of precursor lesions is crucial for preventing cervical cancer, researchers looked deeper into this issue in a follow-up study and concluded that the lower rates of HSIL may be due to the ineffectiveness of screening programs for Indigenous women.
For Bhadra, screening isn’t just about conducting tests—it’s about ensuring follow-up and treatment. “This is a complex health action. You need a lot of steps,” she said. However, limited healthcare access continues to hinder the process. “This process is too complex for an indigenous woman, so public policies should target this as a main challenge to provide treatment.”
Furthermore, research and policy efforts must avoid a one-size-fits-all approach, as Indigenous populations—particularly in regions like the Amazon—are often dynamic, with frequent migration and change. “If you want to go back in time to see how they have evolved, you will find very different populations,” said Sarmiento-Medina.
Therefore, the best way to carry out this work is by involving communities, which ultimately can empower women to demand what they need from health services. “With our work, we tried to train the women so they could become aware of those cultural needs,” said Sarmiento-Medina. “Even they expressed [these needs] when we did the research, and they can demand from the health services that all services be provided according to their cultural needs so that there is greater accessibility.”
Working with indigenous groups to better understand cervical cancer and the factors leading to it can also help dispel some common misconceptions about why these women are more vulnerable to cervical cancer and how to protect them… “There is a lot of prejudice in this topic,” Bhadra said. For example, people say that indigenous women have more cervical cancer because they have sexual contact earlier than non-indigenous women, but as her research showed, precursor lesion rates in young women were not higher than in non-indigenous women.
Another thing both researchers have found was high HPV rates in older women. Sarmiento-Medina’s clinical analysisof the women she worked with showed that HPV infections peaked in younger women and again after age 40. This makes the case for the necessity to expand the target age for vaccination.
Ultimately, if Latin America is serious about addressing this issue, governments must take the lead in gathering better, more comprehensive data, but they can’t do it alone. As Bhadra emphasized, the most effective solutions will come from working within communities themselves. “We need to have researchers coming from the community to help us in this challenge.” It’s time to invest in the people most affected, empower them with tools and training, and treat their insights as essential. The call is clear: listen, include, and act.