In a disease as complex as cancer it seems the most logical way to ensure uniform standards of high quality care for all patients. Team meetings can also offer opportunities for education, provide a way to increase the number of patients entered into clinical trials, facilitate communication between primary, secondary and tertiary care, and provide team members with opportunities for professional development.
In general, members of MDTs that function effectively can barely imagine working in any other way.
Many MDTs however do not function effectively. In some places, MDT meetings are seen as merely ‘rubber stamp’ or ‘tickbox’ operations – something of little intrinsic merit that the system obliges you to go through, where every case is rushed through and the decision reached within the space of a few minutes. In others, discussions are allowed to drag on interminably, for no good reason, with too long being spent on relatively straightforward cases, and many contributions being unduly lengthy or off the point. Sometimes the problem is that one or two voices dominate every discussion, sidelining the contribution of others who have information and expertise that could impact on the recommendation. In some places key team members are often missing from the meeting, because they – or the team organisers or hospital administration –have not prioritised ensuring they can and do attend. Then there’s the whole question of what happens to the discussion and recommendations. How do these feed into the decision making process with the patient, if they do at all?
Sadly, large numbers of cancer practitioners across Europe end up resenting the time they are obliged to spend at MDT meetings, because it seems like an unnecessary and bureaucratic waste of time that yields little of benefit to either patients or doctors.
In an effort to challenge this perception, and explore the realities of team meetings in different places across Europe, Cancer World’s Janet Fricker asked the core members of a well-functioning prostate cancer multidisciplinary team at Addenbrooke’s Hospital in Cambridge, to describe from their own perspective why their team meetings matter to the quality of patient care. Specifically she asked each member of the core team about their role, about what they contribute that their colleagues need to know, about the information they need to receive from their colleagues, and general observations about what makes the meetings work well or how they might be more effective.
We hope to follow this up with a further article where we ask readers to comment on how the functioning of this team compares – the good and the bad – with their own experiences.
Addenbrooke’s multidisciplinary team meetings
 The Addenbrooke’s prostate cancer MDT, one of around 40 different MDTs convened every week at this Cambridge hospital, meets on a Monday afternoon to discuss treatment plans for newly diagnosed prostate cancer patients. Attending the meeting are members of the core team composed of urologists, oncologists, pathologists, radiologists and specialist nurses.
The Addenbrooke’s prostate cancer MDT, one of around 40 different MDTs convened every week at this Cambridge hospital, meets on a Monday afternoon to discuss treatment plans for newly diagnosed prostate cancer patients. Attending the meeting are members of the core team composed of urologists, oncologists, pathologists, radiologists and specialist nurses.
The meeting is divided into two parts. The first part considers patients from regional hospitals, whose healthcare teams dial-in using conferencing facilities. For these patients (usually around 15 are reviewed), local hospitals have already made a diagnosis, but require expert opinions to explore whether patients are suitable for brachytherapy or robotic surgery, which is only provided at Addenbrooke’s. In the second part the team considers local patients, who are listed for discussion when their imaging and pathology results are ready. For these patients (usually around 40 are reviewed), the team decide between recommending surveillance or active treatment in the form of surgery and radiotherapy. Altogether the MDT meeting takes around three hours.
Key to the smooth running is the EPIC system where the patient information is entered on to the computer system by the MDT coordinator prior to the meeting. “This allows us to view all the information on one screen and saves having to spend time hunting it down,” says Veneeta Thankappannair, the prostate cancer specialist nurse. Other important facilities needed are teleconferencing to communicate with external hospitals, a microscope and projection system for the pathologist to show slides, and screens to display the EPIC patient information and radiology images.
Fundamental to the approach of MDTs is that the MDT makes recommendations, rather than taking decisions, with the final decision about the way forward made by the patient in face-to-face discussions with the urologist or specialist nurse in clinic after the meeting.
Urologist – Vincent Gnanapgragasm
 What does your role involve?
What does your role involve?
“In Cambridge the urologist leads the MDT because they are the team member who first sees the patient in clinic and records their medical history and takes the biopsy specimen. Prior to the MDT, the urologist spends about an hour reviewing the notes, biopsy results and imaging, and brings everything together to suggest a treatment plan for each patient that the MDT can discuss.”
What does the team need from you?
“The biopsy specimen and the patient’s medical history, which is important in balancing whether the patient is likely to die of something else sooner than prostate cancer.”
What information do you need from colleagues?
“Their advice about the different treatment options and whether they are aware of any suitable trials.”
Other thoughts
“In Cambridge we’ve pioneered the Predict Prostate tool for the MDT to use at the point of prostate cancer diagnosis for patients with non-metastatic disease (PLOS Med 2019; 16: e1002758). The tool, developed using data from over 10,000 men diagnosed with non-metastatic prostate cancer between 2000 and 2010 with a median follow-up of 9.8 years, estimates survival with and without treatment. The model helps patients and clinicians to decide between active surveillance and radical treatment. For radical treatment it does not distinguish between surgery and radiotherapy. It is really important in balancing whether the patient is likely to die of something else sooner than prostate cancer. The Predict Prostate tool has been endorsed by the UK National Institute for Clinical Excellence as a decision aid in prostate cancer management.”
Clinical oncologist – Yvonne Rimmer
 What does your role involve?
What does your role involve?
“In the UK, clinical oncologists combine the role of radiation oncologist and medical oncologist. Our role is to consider the whole patient and their prostate cancer in the context of comorbidities. We provide in-depth knowledge of radiotherapy and systemic anticancer therapies (hormone treatments and chemotherapy) and know about associated toxicities. We can also let them know about relevant trials. As well as treating patients in the curative setting, oncologists are responsible for treating metastatic disease.”
What does the team need from you?
“They need the clinical oncologist’s view about whether the patient is suitable for radiotherapy and systemic treatments.”
What information do you need from colleagues?
“We need information about the patient’s fitness for treatment and existing comorbidities. Essentially, someone who is fit enough for curative radiotherapy needs to be walking into the clinic unaided. I also need to know about urinary frequency and flow, as a large prostate or bladder insufficiency can affect their ability to have radiotherapy, as can some bowel conditions, such as inflammatory bowel disease. It is also valuable to know about social circumstances, as elderly patients with caring responsibilities may not wish to travel daily for radiotherapy.”
Other thoughts
“To help make things clearer within the busy and time-constrained MDT discussion, it would be valuable to have patients grouped together, for example to have a section in the meeting for men presenting with raised PSA, another for localised prostate cancer and a third for those presenting with metastatic disease.”
Pathologist – Anne Warren
 What does your role involve?
What does your role involve?
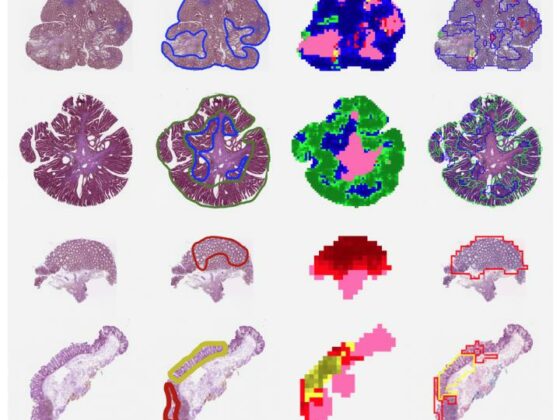
“Throughout the week, sub-speciality pathologists assess microscopically prostate biopsies that have been processed into paraffin wax blocks and cut into thin sections and stained. For each specimen pot (containing fine ‘cores’ of tissue representing different parts of the prostate) we screen for cancer foci. If cancer is found, we provide a histology report detailing the number of cores with tumour, the maximum length of the cancer in a single core and architectural appearance (known as grade) of the tumour. For tumour grading we use both the traditional Gleason Grading system and a new ‘Grade group’ system (proposed by Jonathan Epstein from John Hopkins University) that help to guide the most appropriate treatment options for patients.
For each patient, the whole biopsy reporting process takes between 30 minutes and two hours, depending on the number of biopsies taken. On the morning of the MDT, the pathologist attending the meeting does a quick review of cases to check that no mistakes have been made. Even if the patient has a negative biopsy (~ 30% of patients) they still need to be discussed in the MDT due to the possibility that the biopsies could have missed the cancer.”
What does the team need from you?
“Information about whether cancer is present in the prostate biopsies, and if so the number of cores involved, the maximum length of the tumour present in a single core, the tumour grade (Gleason score and Grade group), and whether there’s evidence of extra prostatic spread.”
What information do you need from colleagues?
“The patient’s clinical history. Many people think biopsies give black-and-white results (like a blood test), but in reality it’s an interpretation of the image you see before you. We can get that interpretation completely wrong if we don’t consider it in context of the patient’s clinical history. We need to have information such as whether the patient has had prior radiotherapy or chemotherapy, whether they have known metastatic spread of the prostate cancer or even a different type of tumour arising in another organ.”
Other thoughts
“Going forward it would be helpful to always undertake the biopsy after the MRI scan, as this would allow you to screen out the patients where there are no visible lesions on imaging and to focus on biopsying patients with visible ‘target’ lesions.
The difficulty with biopsying everyone is that you identify lesions that aren’t clinically significant and don’t need to be treated. Doing an MRI scan first would be better for patients and allow us to improve efficiency by rationalising the amount of pathology we need to do.”
Specialist nurse – Vineetha Thankappa Nair
 What does your role involve?
What does your role involve?
“The nurse provides the first point of contact for prostate cancer patients and their families at Addenbrooke’s Hospital, ensuring that the pathway runs smoothly with tests undertaken in a timely fashion, and helps to counsel patients through the decision making process after the urologist has broken the bad news. Specialist nurses provide holistic support and signpost patients to other support services, such as psychological support services.”
What does the team need from you?
“I act as the patient’s advocate and provide information about the patient to other team members and communicate the recommendations with patients.
A nurse will have met the patient prior to the MDT and found out about comorbidities, their social situations, and any treatment preferences.”
What information do you need from colleagues?
“We need information about diagnosis and treatment recommendations to relay to patients, including how different treatments would impact on comorbidities. It’s also helpful to know whether there are research studies that the patient might be suitable for in future, allowing us to flag up the possibility to them at an early stage.”
Other thoughts
Patients are normally only considered by the MDT at diagnosis, and referred directly to the oncologist if they have a recurrence. From the nurse’s point of view I would find it valuable to run patients with recurrent prostate cancer past the MDT to discuss benefits of different treatment approaches. For example, this could be when progression is identified and men become eligible for hormone therapy, or when men become resistant to hormone therapy and are considered for second line treatment or chemotherapy.”
Radiologist – Tristan Barrett
 What does your role involve?
What does your role involve?
“Prior to the MDT, a radiologist will have reviewed the MRI and CT scans. MRI is used for local diagnosis to determine where lesions are located in the gland, while CT scans are used for advanced or metastatic disease. While CT is a generalised radiology skill, MRI is much more specialised and needs radiologists who are proficient at interpreting different anatomical areas. For example, I am experienced in prostate, bladder, and kidney MRIs, but am not nearly so expert at analysing liver and gynaecological MRIs.”
What does the team need from you?
“Information on TNM staging, which describes the size of the tumour, and whether the cancer has spread to the lymph nodes, or different parts of the body. Radiology can also provide a definitive answer to say no disease is present here and further investigations are not required.”
What information do you need from colleagues?
“We need information from the urologist about the specific focused question they want answered, as this can help reduce the number of images that we need to view. Also, it’s useful to know whether the patient has any other relevant clinical history that may make a tumour likely, or indeed information that may make a benign process more probable, such as a treated prostate infection and a subsequent reduction in the PSA levels.”
Other thoughts
“The MDT process could be streamlined, removing straightforward cases and allowing longer slots for patients who need more time for discussions. When I worked in the US and Canada they limited MDT discussions to four or five cases that are considered to be management or diagnostic conundrums.”












2 comments
An interesting read but very disappointing to see that no member of the MDT takes specific responsibility for identifying any research opportunities (eg clinical trials, tissue donation etc) for which the patient might be eligible and which then might be discussed with him alongside treatment options. The NHS Constitution says that patients should be made aware of research opportunities, and the 2012 report Action on Access from the NCRI Consumer Forum (https://www.ncri.org.uk/wp-content/uploads/2013/07/2012-NCRI-Action-on-access-report.pdf) places the onus squarely on the MDT. So it is sad not to see anyone taking responsibility at the MDT meeting. I am sure this hospital does try, but nationally only 30% of cancer patients have discussions about research (based on CPES and NIHR data). We can all do better.
An interesting read but although there’s a cmment that “We can also let them know about relevant trials,” it is very disappointing to see that no member of the MDT takes specific responsibility for identifying ALL research opportunities (eg clinical trials, tissue donation etc) for which the patient might be eligible and for making sure that these are definitely discussed with him alongside other treatment options. The NHS Constitution says that patients should be made aware of research opportunities, and the 2012 report Action on Access from the NCRI Consumer Forum (https://www.ncri.org.uk/wp-content/uploads/2013/07/2012-NCRI-Action-on-access-report.pdf) places the onus squarely on the MDT. So it is sad not to see anyone taking direct personal responsibility at this MDT meeting. I am sure that this hospital does try, but nationally only 30% of cancer patients have discussions about research (based on CPES and NIHR data). We can all do better.
Comments are closed.