The UK National Health Service (NHS) announced on the 27 November that it would be piloting an early detection multi-cancer blood test next year. This represents an important advance because “every year, nearly 200,000 people in the UK die from cancer. Many of these people are diagnosed too late for treatment to be effective,” said Lord David Prior, Chair of NHS England.
In a press release, the NHS detailed plans to roll out the pilot in two separate phases and involve 165,000 people. The first phase will include 140,000 people over the age of 50 without any suspicion of cancer, and the second phase will enrol 25,000 people aged 40 and above with suspicious signs or symptoms of cancer. If results of initial studies, expected by 2023, prove positive, the NHS aims to expand the programme to around one million people between 2024 and 2025, and beyond that to larger populations.
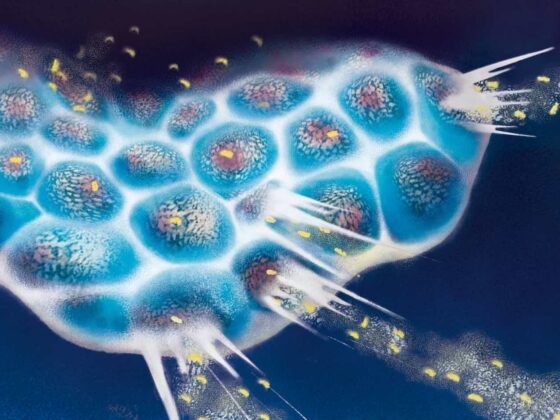
The selected Galleri blood test, developed by GRAIL. Inc. (Menlo Park, California), utilizes next-generation sequencing to analyse clusters of methyl chemical groups attached to specific sections of DNA shed into the blood when tumour cells die. The methyl groups help to control whether genes are active or inactive. For development of the Galleri test, machine learning has been used to enable identification of distinct patterns of DNA methylation relating to different types of cancers and to show how these differ from the methylation of DNA shed by normal cells.
The selected technology, which will be the first cancer screening blood test to be widely deployed, claims to be capable of identifying 50 different types of cancer from a single blood draw. “Early detection, particularly for hard to treat conditions like ovarian and pancreatic cancer, has the potential to save many lives. This promising blood test could therefore be a game changer in cancer care, helping thousands more people to get successful treatment,” says Sir Simon Stevens, NHS England’s Chief Executive.
In a study published earlier this year, Geoffrey Oxnard and Minuetta Liu, from Dana–Farber Cancer Institute, Boston, used the Galleri test to analyse 6,689 blood samples taken from 2,482 people diagnosed with cancer and 4,207 healthy controls without cancer. For the study, samples were divided into training (n=4,720) and independent validation sets (n=1,966). The samples from people with cancer represented more than 50 cancer types, including breast, colorectal, oesophageal, gallbladder, bladder, gastric, ovarian, head and neck, lung, lymphoid leukaemia, multiple myeloma and pancreatic cancer.
Results showed the overall specificity of the validation test was 99.3% meaning that only 0.7% of results incorrectly indicated that cancer was present. For all cancer types for the validation test sensitivity was 18% (CI: 13–25%) in stage I, 43% (CI: 35–51%) in stage II, 81% (CI: 73–87%) in stage III, and 93% (CI: 87–96%) in stage IV. To put this in context, the results indicate that for patients with stage I cancer, 18% of patients with cancer would correctly receive a positive result, but 82% would receive a false negative result (meaning that their cancer was not identified). Furthermore, performance varied markedly between cancers, with the validation sensitivity test in stage I cancer being 63% for pancreatic cancer, but for breast, oesophageal, and kidney cancers it came close to 0%.
On the basis of these results Paul Pharoah, Professor of Cancer Epidemiology at Cambridge University, UK, questions why the NHS are now embracing a screening test that has not been demonstrated to work. Speaking to Cancer World, Professor Pharoah says, “A sensitivity of 18% in stage I cancer represents a completely inadequate level of performance for a screening test. You would need to achieve sensitivity levels nearer 80% to have any confidence in a test.” There can be devastating consequences, he adds, if clinicians wrongly tell patients that their test is negative when they do in fact have cancer. “There’s a real danger that if patients have a false-negative screening test and get symptoms 2 months down the line, like a breast lump, they’ll take much less notice and won’t get them properly checked out.”
Pharoah further suspects the overall intentions of the NHS pilot. A pilot study, he explains, is designed to evaluate the feasibility of a process. “It’s not necessary to use the test 165,000 times in order to pilot feasibility. This suggests that the aim of the ‘pilot’ is to address scientific questions, like effectiveness of the test. However, these questions are not described in the press release. It’s not the role of the NHS to roll out clinical services before the important scientific questions have been appropriately addressed.” Several other technologies identifying cancer biomarkers in the blood are in the process of development for early detection by a number of companies and organisations.