Nearly one billion people in Africa depend on polluting fuels like wood, charcoal, and kerosene for cooking, lighting, and heating their homes. The resulting household air pollution leads to approximately 700,000 premature deaths every year, constituting about 10% of the continent’s total mortality. In Kenya alone, an estimated 23,000 lives are lost annually due to household air pollution.
,Women and children in sub-Saharan Africa are the most affected because they spend long hours cooking breathing in unhealthy smoke. If they are pregnant, the exposure is also passed on to the unborn child.
“Most of the people who are sick today were already exposed when their mothers were cooking while they were still pregnant with them,” says Sumi Mehta, Vice President of Environmental and Climate Health at Vital Strategies, a global health organisation that partners with governments on public health initiatives in low- and middle-income countries.
“Household energy is not just an environmental or climate concern. It’s a health concern”
“We need increased awareness about the fact that household energy is not just an environmental or climate concern. It’s a health concern. Even if there are anticipated long-term impacts on the climate, addressing this issue now can yield short-term benefits for public health.”
Polluting cooking fuel can cause cancer
Risks associated with exposure to smoke from biomass fuel, and its components, are well established, particularly for oesophageal and gastric cancers. A 2020 study by the WHO’s International Agency for Research on Cancer, IARC, concluded that, “there is strong evidence that household burning of biomass and kerosene fuels, especially using stoves without a chimney, increases the risk of developing several cancers of the digestive tract.”
Alfred Jatho, head of community cancer services at the Uganda Cancer Institute, says that, given that 70% of the African population relies on biomass for lighting and cooking, the health implications are substantial. Respiratory and lung diseases such as pneumonia, stroke, ischaemic heart disease, and chronic obstructive pulmonary disease are linked to exposure to cooking smoke. While there is some evidence for a link with lung cancer, the more significant risks are associated with oesophageal and gastric cancers, especially in East Africa.
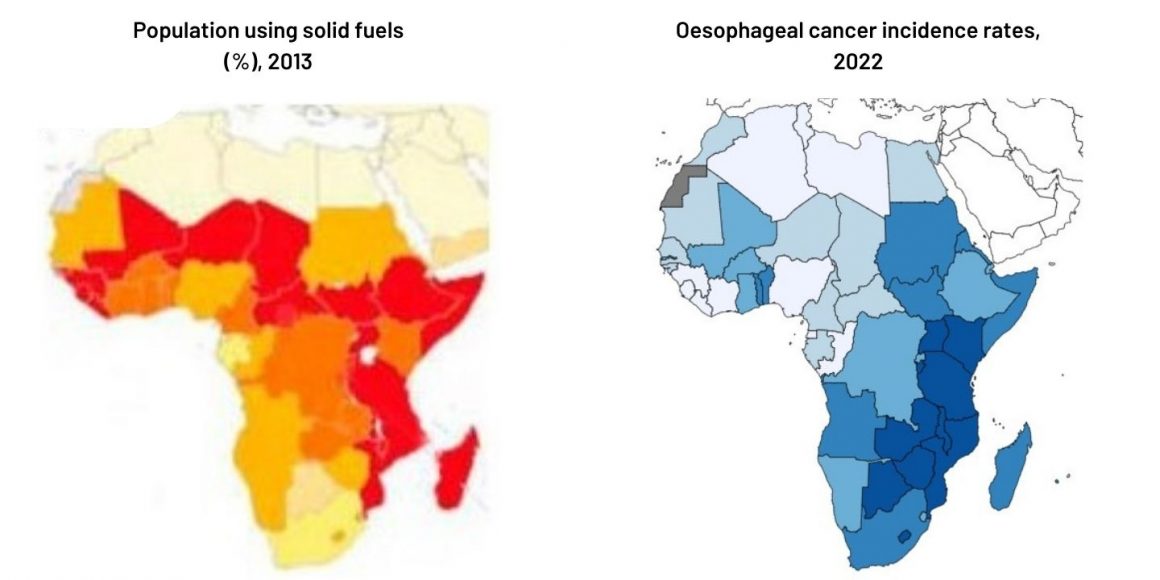 Oesophageal cancer incidence rates correlate with use of biomass for cooking Left: Heat map showing use of solid biomass fuels for cooking; Right: Heat map of oesophageal cancer incidence rates in 2022
Oesophageal cancer incidence rates correlate with use of biomass for cooking Left: Heat map showing use of solid biomass fuels for cooking; Right: Heat map of oesophageal cancer incidence rates in 2022
Sources: Left: Adapted from Silent suffocation in Africa. UNICEF 2019 © United Nations Children’s Fund (UNICEF) June 2019; Right Cancer TODAY. International Agency for Research on Cancer. Data version: Globocan 2022.Downloaded 5 February 2024. © IARC WHO 2024
Oesophageal cancer ranks as the third leading cause of cancer deaths in Uganda, though it is the sixth in terms of incidence. Unfortunately, it exhibits one of the poorest treatment outcomes among all cancers. While women face a higher risk because of the time they spend cooking, risk is shared throughout the household when cooking and sleeping occur in the same space.
“Individuals should aim to cook outdoors when possible and not remain in the same area while cooking is taking place to allow the smoke to disperse,” says Jatho.
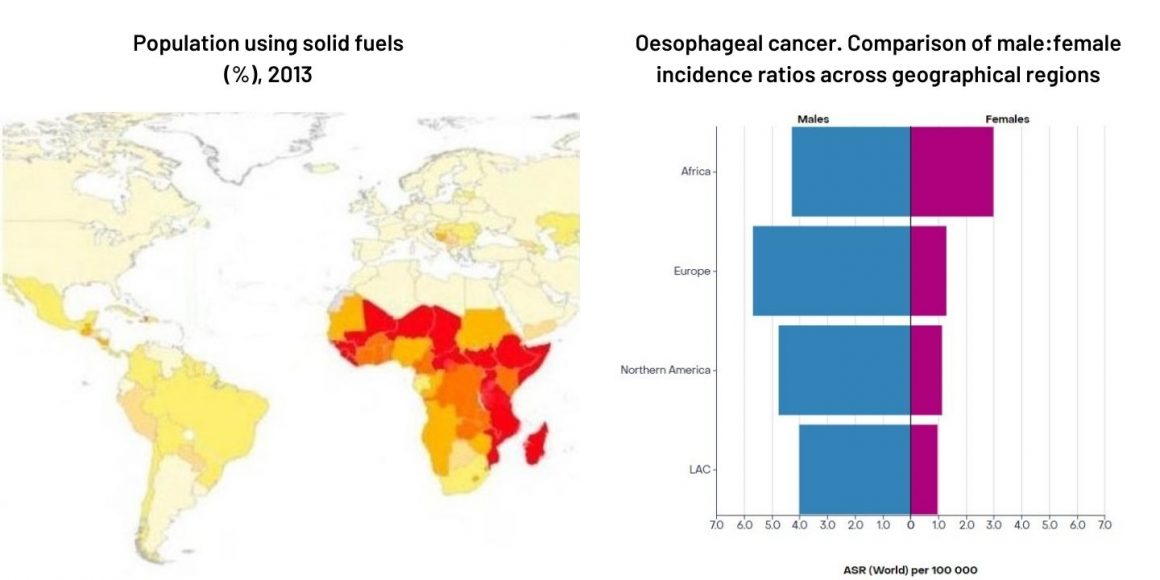 The association between exposure to polluting cooking smoke and oesophageal cancers is reflected in the disparity in male:female incidence ratios between Africa and regions that use cleaner cooking fuels. While in Europe and the US, where smoking and drinking are the major risk factors, the male:female incidence ratios are 4:1 and 5:1 respectively, in Africa that drops dramatically to 1.5:1.
The association between exposure to polluting cooking smoke and oesophageal cancers is reflected in the disparity in male:female incidence ratios between Africa and regions that use cleaner cooking fuels. While in Europe and the US, where smoking and drinking are the major risk factors, the male:female incidence ratios are 4:1 and 5:1 respectively, in Africa that drops dramatically to 1.5:1.
Sources: Left: Adapted from Silent suffocation in Africa. UNICEF 2019 © United Nations Children’s Fund (UNICEF) June 2019; Right Cancer TODAY. International Agency for Research on Cancer. Data version: Globocan 2022.Downloaded 5 February 2024. © IARC WHO 2024
Creating awareness
Clean air initiatives in various African countries are attempting to create awareness of the problem and educate the public. But alerting people to the risk, and changing behaviour, is not always as easy as it may sound, says Jatho. Perceptions and responses to the risk depend on the audience, he notes, “In rural areas where people may lack smoke sensors, the air might not be perceived as bad. In city centres, on the other hand, individuals may attribute more pollution to factories.”
In Kenya, the MaMa Doing Good initiative, partnered with the University of Liverpool and the Kenya Medical Research Institute, is promoting the use of household clean energy.
The CLEAN-Air Africa initiative, co-led by the University of Liverpool and the Kenya Medical Research Institute, is a collaboration between health authorities and institutions in Kenya, Tanzania, Rwanda, Uganda, and Cameroon, which is now training village health traditional workers and community health workers to create awareness in both Uganda and Kenya. Around 2,500 instructors across all 47 counties of Kenya have now been trained, and these instructors will go on to train 120,000 community health workers, with the aim of reaching Kenya’s entire population.
In Uganda, under the CLEAN-Air (Africa) Programme, the Ministry of Energy and Mineral Development is set to collaborate with the Makerere University Lung Institute, the University of Liverpool and the Ministry of Health to raise awareness about clean cooking practices and the risks associated with household air pollution. It will train Village Health Teams to encourage change, incorporating issues about cooking smoke and air pollution into their toolkits for educating communities and households.
In a meeting held in Kampala, there was discussion on ways in which doctors might “prescribe” clean cooking as a treatment for respiratory morbidities.
Cooking with polluting fuel and lung cancer
While lung cancer is not very prevalent in Africa, there is evidence to show that cooking with polluting fuel could be a significant risk factor.
- A 2015 systematic review published in Thorax found exposure to household use of biomass fuel almost doubled the risk of lung cancer in women (OR 1.95, 95%CI 1.16–3.7), with a lower impact on men (OR 1.29, 95%CI 1.05–1.39). The authors concluded that “There is now stronger evidence for biomass fuel use causing lung cancer, but future studies need better exposure assessment to strengthen exposure–response evidence.”
- A 2023 paper in Nature, threw new light on this association, with its findings that the key mechanism linking air pollution to lung cancer is inflammatory effects caused by inhalation of small particulate matter (PM2.5) rather than chemical carcinogens.
- PM2.5 particles during cooking indoors with biomass fuel have been found to be five times higher (176.13 μg/m3) than the maximum level considered safe by the World Health Organization (<35 μg/m3).
“Understanding that not everything natural is necessarily good for you is key – just because wood is natural doesn’t mean it’s entirely safe”
“I believe that, in terms of the messaging, ensuring that this is seamlessly integrated into public health awareness efforts is crucial,” says Mehta. “People’s interest will peak when they realise that it directly affects their health and their children’s health. Understanding that not everything natural is necessarily good for you is a key realisation – just because wood is natural doesn’t mean it’s entirely safe.”
But there is also the need for guidelines and regulations concerning indoor air quality, particularly in schools and healthcare facilities. According to Bruce Kirenga, a senior respiratory physician, and Director at the Makerere University Lung Institute in Uganda, implementing such regulations would significantly reduce exposure to indoor pollutants. Speaking during a recent air pollution webinar, he highlighted the significance of air quality monitoring and early warning systems.
Helping schools in Kenya to transition away from using wood to cook for staff and pupils is currently a particular focus for CLEAN-Air Africa, where they are distributing air pollution monitors for use in kitchens, classrooms and playgrounds.
Ultimately, says Mehta, when people have access to clean fuels, they genuinely prefer using them – not just for health reasons, but also for convenience.
Promoting access to alternatives
Government action would have an impact. Matt Shupler, a Postdoctoral Research Associate at Harvard Chan School of Public Health, says that governments need to increase the affordability and accessibility of cleaner fuels like electricity, ethanol and liquefied petroleum gas (LPG), so that households can switch to these fuels.
“The first step is to scale down the cost of electricity – a connection costs UGX 700,000, which is a full year’s income for a farmer”
According to Uganda’s Ministry of Energy and Mineral Development, one of the primary targets of its energy policy is to enhance access to clean cooking technologies, such as electricity, LPG, biogas, ethanol and solar, aiming for an increase of around 30%. The plan also aims to provide improved cooking stoves to an additional 3 million rural households. Shupler suggests that cooking demonstrations, recipes and education could help increase uptake, “Because some families are not used to cooking with these cleaner fuels.”
To promote switching to cleaner energy options, the government has removed VAT on solar panels and LPG and brought in a price subsidy for extra units of electricity used in cooking. Yet, they remain largely out of reach for the majority of the population. According to Samuel Opio, Deputy Chairperson of the Parliamentary Health Committee in Uganda, the biggest challenge on air pollution is that the people using firewood cannot afford clean energy. “The first step is to scale down the cost of electricity – a connection costs UGX 700,000 (US$ 194), which is a full year’s income for a farmer.” He proposes that cooking gas should be subsidised.
Mehta argues that part of the barrier lies in having to purchase a full LPG cylinder. She points to efforts to find “innovative ways to make LPG more affordable and accessible.” In East Africa, entrepreneurs are making use of mobile money platforms, such as M-PESA, to create pay-as-you-go models. This would allow users to incrementally purchase fuel in smaller amounts, mimicking the regular purchasing patterns of charcoal users.
Taking basic steps to avoid kitchens becoming traps where smoke pollution cannot escape could also make a significant difference, suggests Opio. “We… need to make simple structural designs on houses in the villages,” he said. “Kitchens do not have plans. They end up with no ventilation – no chimneys, no windows, only doors,” he said.
Shupler warns, however, that the health impact of tackling air pollution from household use of solid biomass fuels may be limited unless measures are also taken to tackle environmental air pollution from other sources, particularly in the light of the rapid pace of urbanisation in many part of Sub-Saharan Africa. This is a key finding of a study he co-authored, which has just been published in Lancet Planetary Health.
“High outdoor air pollution in urban sub-Saharan Africa is likely reducing the ability of use of clean cooking fuels to reduce fine particulate matter exposures to levels that are deemed safer for public health. Providing households with clean cooking fuels might not, by itself, lead to meaningful health benefits, if they are exposed to high PM2.5 levels when spending time outdoors,” Shupler told Cancerworld. “More policies that target reductions in outdoor air pollution are needed. This relates to regulations on traffic emissions, and reductions in other local sources like outdoor trash burning.”
The opening illustration shows monitoring of air pollution levels (PM2.5 particles and carbon monoxide) in an enclosed cooking area in Kenya. It is taken from a video about the CLEAN-Air (Africa) Centre of Excellence at the Kenya Medical Research Institute (KEMRI), published by the NIHR CLEAN-Air(Africa) Global Health Research Unit at the University of Liverpool, and is used here with their kind permission












