Telemedicine, in addition to patient convenience, offers the environmental benefit of reducing greenhouse gas emissions, with knock-on benefits for people with chronic conditions. The study, presented at the annual meeting of the American Society of Clinical Oncology (ASCO), held May 31 to June 4, and published simultaneously in JAMA Oncology, suggests that delivering cancer care using telehealth and local care, as opposed to traditional models of more centralised in-person care, would reduce greenhouse gas emissions in the US by one third, and furthermore save a few lives.
“Tele-medical and decentralised cancer care does provide a large relative reduction in emissions. It’s potentially a gain downstream for human health and planetary health,” says lead author Andrew Hantel, an oncologist from the Dana-Farber Cancer Institute.
In the process of treating people, healthcare services produce substantial amounts of greenhouse gas emissions that fuel climate change and downstream harms to health. Studies have recently began assessing greenhouse gas emissions related to the delivery of healthcare, with one study published in JCO Oncol Pract in 2023, finding emission reductions of up to 20% for alternative dosing schedules of the breast cancer drug trastuzumab. However, emissions related to a central component of oncology care, outpatient visits, have not been explored.
The current study set out to assess potential reductions in greenhouse gas emissions and downstream health harms associated with telemedicine and fully decentralised cancer care, using the ‘natural experiment’ of the Covid-19 pandemic, which shifted in-person healthcare to telemedicine.
The team calculated the amount of carbon dioxide emitted per visit-day at Dana-Farber Cancer Institute over two time periods: March 2015 to February 2020 (when the traditional in-person model was in place) and March to December 2020 (when Covid-19 prompted a shift to telemedicine).
The first objective was to calculate the difference in greenhouse gas emissions between the first period of the study and the pandemic period, defined as: all the cancer-related clinical care received by one patient over one day.
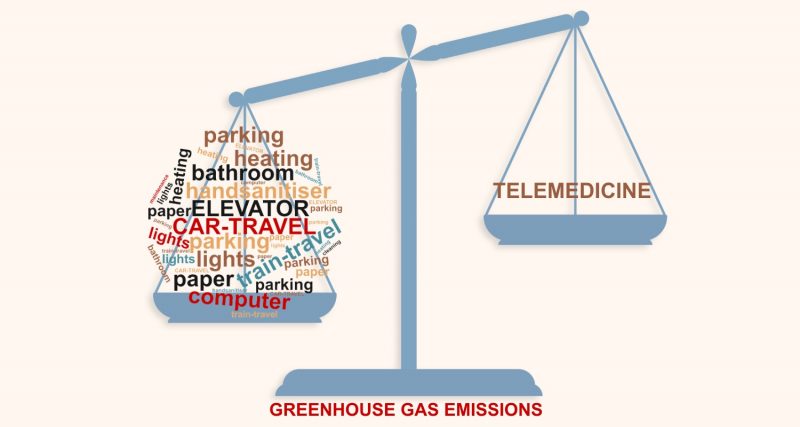
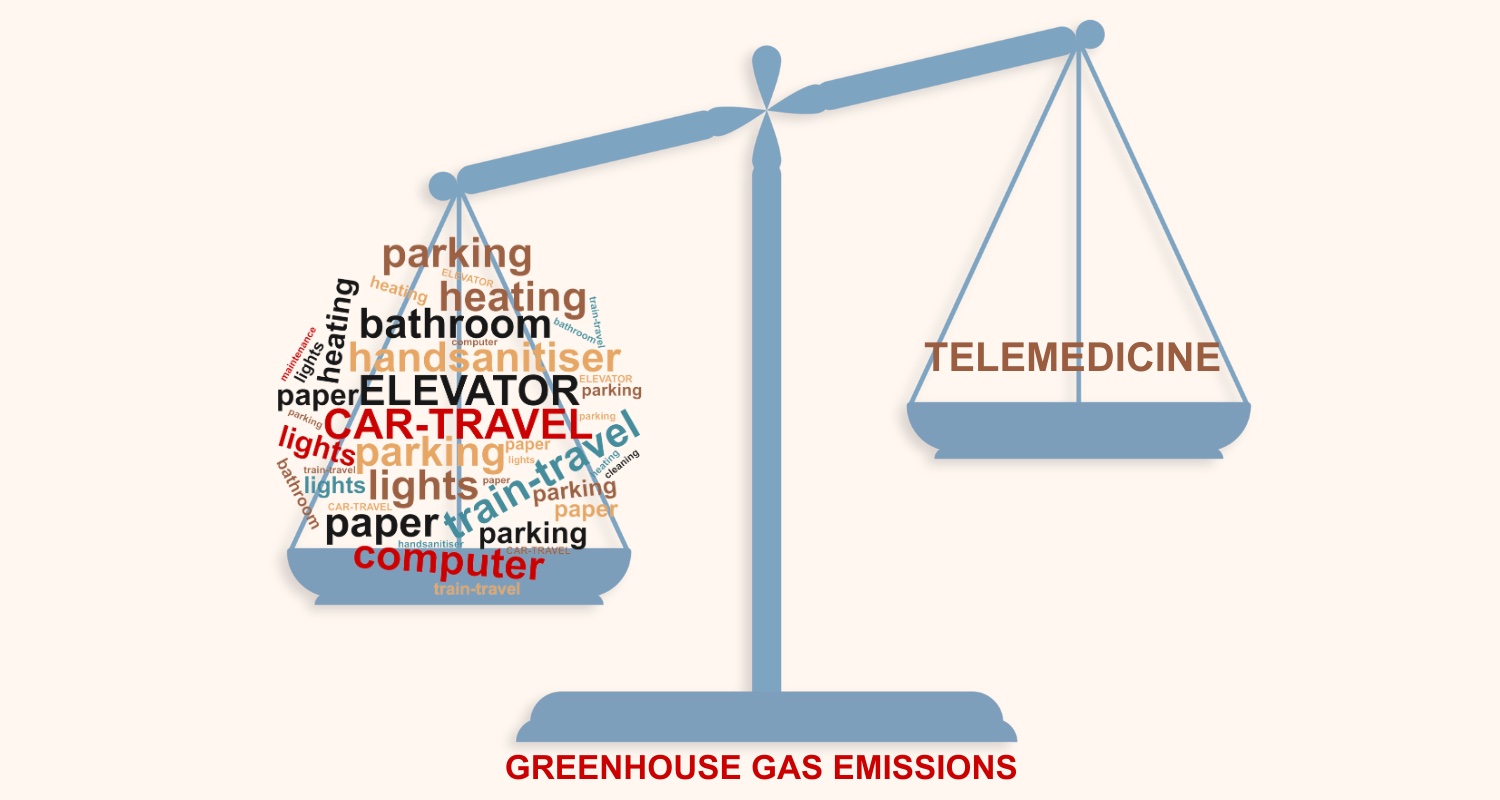
The methodology involved listing all the components of clinical contact for both in-person and telehealth appointments. For clinical visits, this included the patient driving to the hospital, parking the car, taking the elevator, using hand sanitiser, and using the bathroom. They also factored in the use of electricity for lights and computers, and even the paper that covered the exam room table. For telehealth visits they considered computer and internet usage by the patient and clinician. All categories of environmental impact were converted to greenhouse gas emissions in kilogrammes of carbon dioxide (CO2) equivalents.
Altogether 123,890 patients were seen – 110,180 in the pre-pandemic period and 61,691 in the Covid period. Using mixed-effects log-linear regression, the mean absolute reduction in per-visit-day CO2 equivalent emissions between the pre-pandemic period and Covid period was 36.4 kg (95%CI 36.2–36.6), representing a reduction of 81.3%.
Next, the team calculated what emissions levels during the pre-pandemic period would have been if telemedicine had been in place, and they extrapolated their findings to the entire US population. They calculated that CO2 emissions would have been reduced by 75.3 million kg – representing a 33.1% drop.
The more modest percentage decline in emissions calculated for entire US in comparison to the Dana-Farber Institute, suggest the authors, may be due to more people at the institute having rare cancers, requiring them to travel further to receive care.
On the national scale, the 75.3 million kg decline in CO2 corresponds to a modest reduction in human health harms, equating to between 15.0 and 47.7 disability adjusted life years, calculated using a conversion method outlined in a 2018 paper in the American J Public Health. “We used disability adjusted life years, a standard metric for assessing the ‘years of healthy life lost; as opposed to lives saved’, because lives saved does not account for the number of years the person saved could have lived, which is generally very different for an eight-year-old as opposed to an 80 year old,” Hantel tells Cancerworld.
“While much in-person and tertiary oncology care is essential, these data show that decentralizing care when possible can meaningfully reduce visit-related emissions, which in turn can have downstream impacts on human health,” conclude the authors. Since emissions have a greater adverse impact on people with chronic conditions, such as cancer, they add, reductions are likely to disproportionately benefit these patients.
Limitations of the study, write the authors, include the cohort coming from a single cancer care system, which might limit generalisability due to variations in travel patterns according to geographic region, urbanicity/rurality, and other factors.
Next, the team plan to assess the impact of other types of care delivery changes on emissions, such as different chemotherapy schedules and changes to radiotherapy dosing (hypofractionation). “We are also conducting studies on what patients and physicians think about environmental health and how they might incorporate it into their oncology practice,” says Hantel.