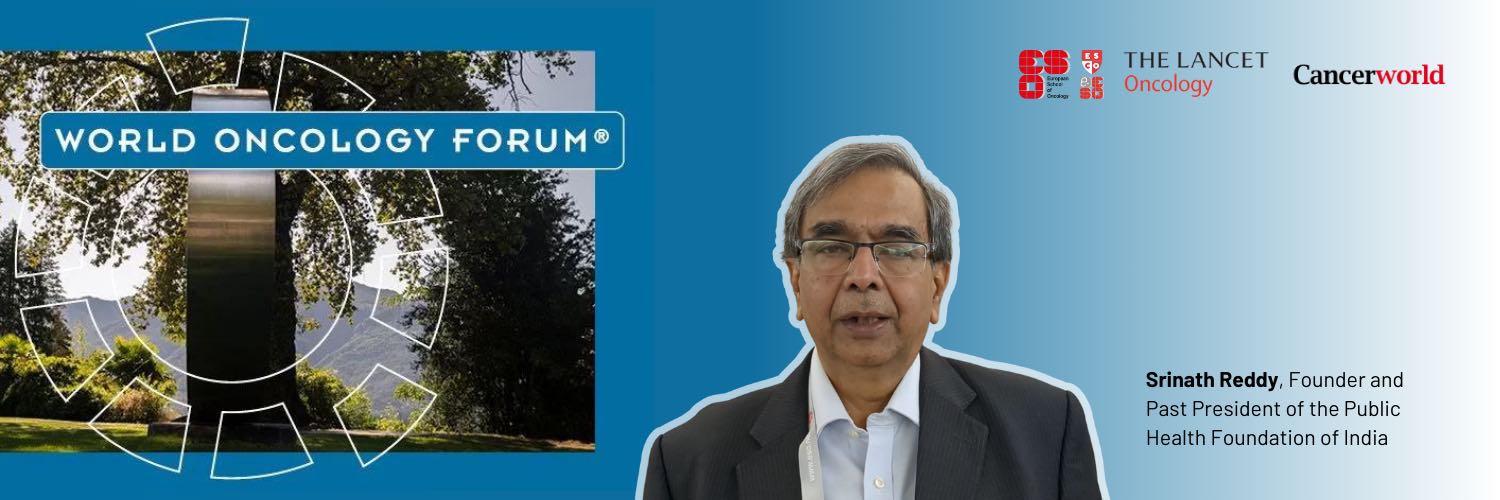
What progress can we point to? I think there has been a tremendous amount of progress in understanding the dimensions and distribution of cancer as a growing global threat. Not only about the types of cancer in each region, but also the magnitude of the problem – how it is affecting larger numbers in terms of cases, deaths and quality of life, with gender distribution and social economic distribution also understood, and some of the causes of etiological factors also identified. There has been also a great deal of advance in diagnostics and treatments. We now have a fair amount of knowledge about the causes and a reasonable amount of knowledge about what are the effective interventions.
Where are we failing? The ability to effectively introduce what we know into the health system and efficiently deliver them for the benefit of people is certainly lacking. Preventive services have not been adequately incorporated into primary care. The same is true for diagnostic services, because you need an early pick up for effective treatment. Then even where primary care has succeeded in picking up cases, connectivity of care to higher centres when needed, and affordability of care, have all been considerable challenges. So, despite the advances in our knowledge, the utilisation of that knowledge for the benefit of people – for the prevention of cancer, for diagnosis of cancer, for treatment of cancer, rehabilitation, palliation and supportive care, all of these elements – has not happened.
What should we be advocating for today? The way forward is very clear. We need to implement primary care led universal health coverage very strongly, so that many of the preventive measures as well as early diagnosis are possible as part of that. But we also need to build in competent services at secondary and tertiary care levels and connect them to primary care. Most important of all, we need to make care affordable, and we also need to strengthen our health workforce so we can have people who can deliver the wide range of services that are needed, with the required efficiency and empathy. These are some of the things we need, particularly if we are aiming for equitable delivery of efficient services.
This was one of eight interviews with participants of the World Oncology Forum that were conducted by Cancerworld. Click on the links below to see what the others had to say.
Advocating for accessible cancer care in the global South: are we doing this all wrong?
Nirmala Bhoo Pathy, Public health physician, University Malaya, Kuala Lumpur
“What is not being discussed is how do we improve wellbeing?”
See interview summary | See video
Miriam Mutebe, Breast cancer surgeon, Agha Khan University, Nairobi, and President Elect of AORTIC, the African Organisation for Research and Training in Cancer
“We need to think critically about how our healthcare system can deliver the best for patients”
See interview summary | See video
Felicia Marie Knaul, Co-chair of the Lancet Commission on Cancer and Health Systems, Sylvester Comprehensive Cancer Center and Director of the Institute for Advanced study of the Americas, University of Miami, Florida, President of the Mexican breast cancer advocacy group Tómatelo a Pecho
“In this post-Covid world we have the opportunity to harness technology in ways that we have never seen before”
See interview summary | See video
Bente Mikkelsen, WHO Director for Non-Communicable Diseases
“We should think through what is needed to ensure we have accountability, and simplify the metrics on what success looks like”
See interview summary | See video
Franco Cavalli, Founder & organiser of the World Oncology Forum, past Chair of the Scientific Committee of the European School of Oncology, past President of the UICC
“We need another approach, where governments, public spending, taxes, together with development banks play the overarching role in financing the global fight against cancer”
See interview summary | See video
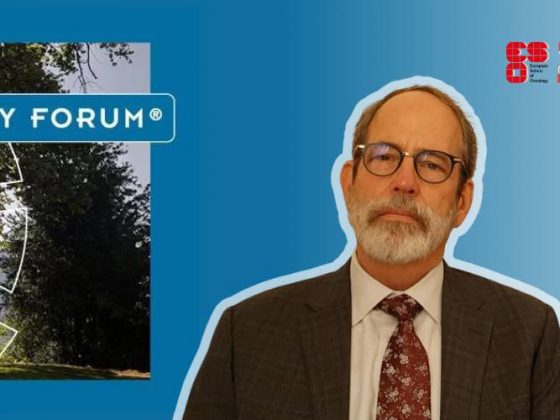
Ben Anderson, Breast Cancer Surgeon, WHO Global Breast Cancer Initiative lead
“Our role is not to tell everybody what to do; it’s to create tools so they can do this in the way that is most effective in their environment”
See interview summary | See video
Mary Gospodarowicz, Radiation oncologist at Princess Margaret Cancer Centre, University of Toronto, co-chair of the Lancet Commission on Cancer and Health, Past President of the UICC
“We’ve been talking to decision makers for 20–30 years. It hasn’t worked. I think we now have to engage better with the public”