This is a particularly worrying time for people going through chemotherapy and other treatments that suppress the immune system. So what advice is being offered by oncology departments and what extra measures are being taken to keep their patients safe? We hear from the partner of a woman who is being treated for ovarian cancer at a hospital in England.
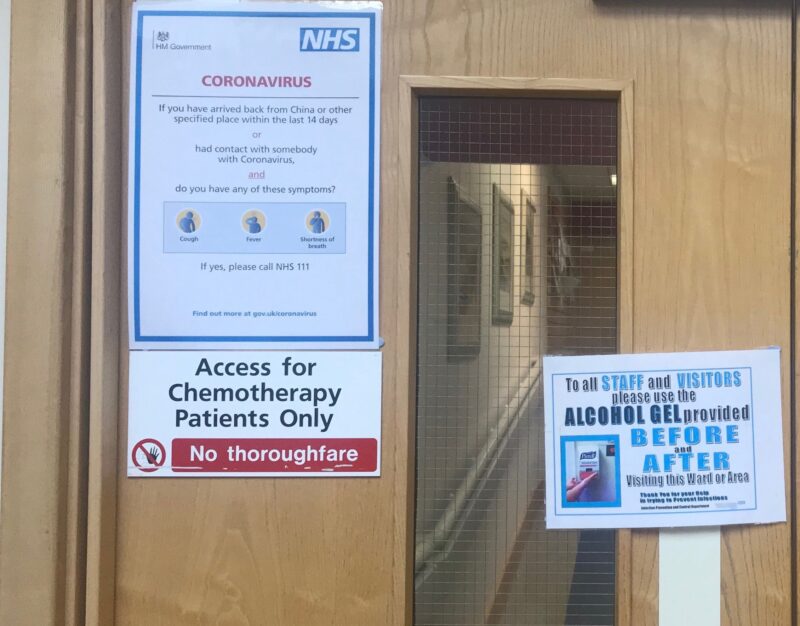
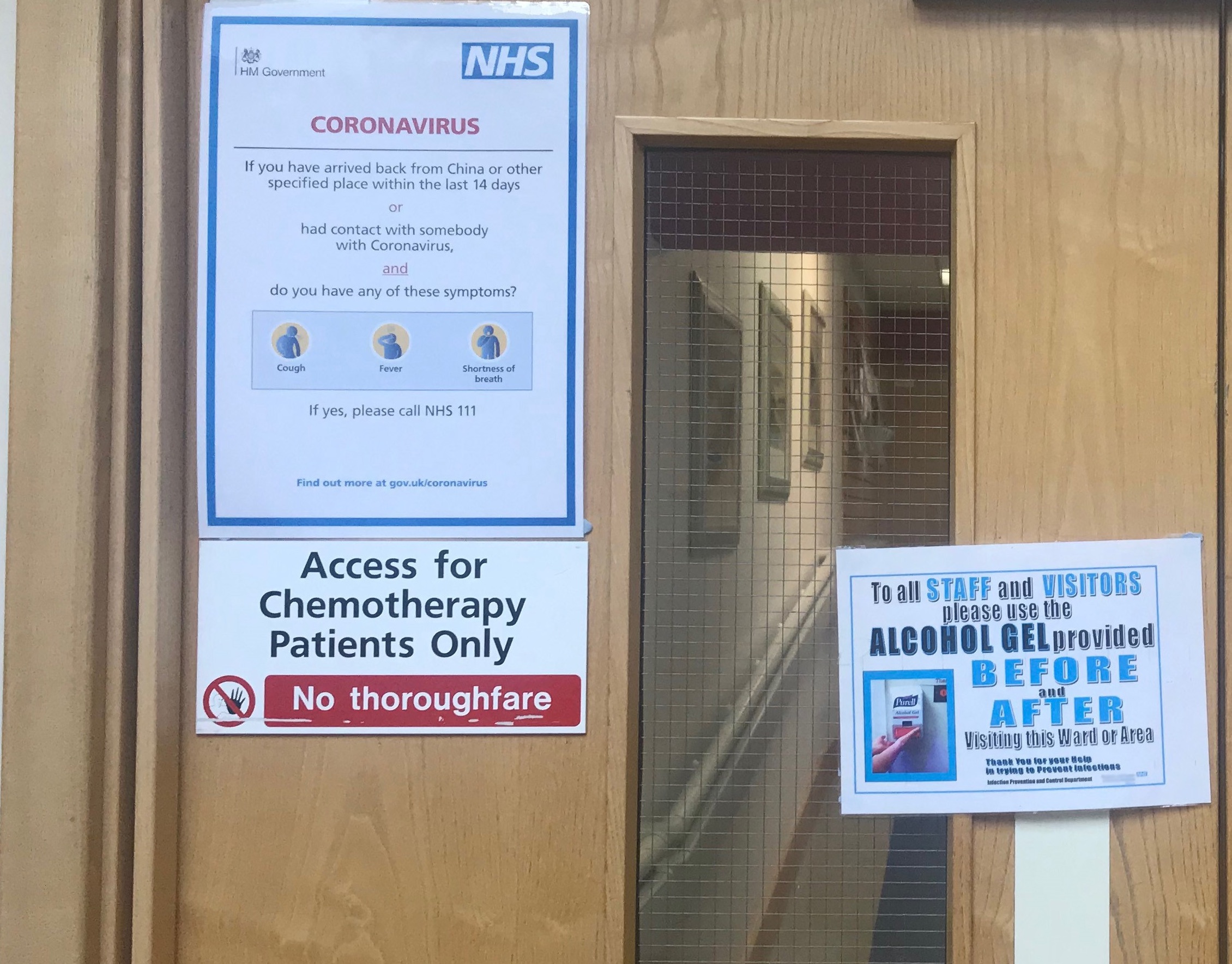
I am at the Cancer Centre, typing while my partner receives her fourth chemo cycle at (what seems to be) the height of pandemic panic. There’s no sign of anything different from the first chemo round in January, when no-one was even talking about COVID-19 – apart from notices on the door of the chemo room encouraging everyone to sanitise and wash their hands.
Our lovely chemo nurse is quite “life must go on” about the whole thing, and I suppose he has to be. He was saying “No matter what you do, there’s a chance you’ll get it.” The main priority here, I think, is that if you need chemo, you need chemo, and you run the risk like everyone else. I think it’s partly because staff can’t actually cope any other way. The alternative is that everything stops.
I was half expecting someone to phone us before the chemo appointment, just to tell us whether COVID-19 would change anything. I was half expecting to be swabbed for the virus, and for nurses and patients to be wearing face masks None of this happened. We have an outpatient clinic appointment with the oncologist next week, and there’s no sign of that being cancelled, postponed or conducted by phone. Is this good or bad? I have no idea.
I expect things are totally different in a country like Italy, but in the British NHS my impression is that it’s genuinely a case of keep calm and carry on. Possibly that’s because it is simply impossible, financially or practically, to introduce special measures for those whose need for treatment is urgent and important.
That doesn’t mean there aren’t strains on individuals and families. My partner had to be admitted to hospital with neutropenia earlier on in her treatment cycle, and she and I are constantly discussing what to do: whether we should ask about suspending treatment, how the risk/benefit equation adds up, whether we should call the consultant. But I think the fact is no one, not even COVID-19 experts, have the knowledge on which to base decisions. It’s an evolving virus and an evolving pandemic: no one knows what to do.
Just next to us in the chemo room, a lad of about 20 is in with his mum, having been battered by a course of intensive chemo for the past couple of weeks. He doesn’t seem bothered about the hand sanitising stuff, though he is shocked at the state of the toilets. His mum wipes the chairs before they sit down.
Next to him is a poor woman virtually frozen by anxiety. All she can do is talk about cleaning things, and how worried she is, and how she doesn’t know what to do given the risk of neutropenia. Some nurses have just come to clean her chair and the area around it.
Next to her is a man over the age of 70 who we’ve seen and spoken to at each of our sessions. He’s not well. He’s had a constant cough, and he’s just told the nurse he’s been feeling poorly and hadn’t eaten properly since the last chemo three weeks ago. His nurse, unlike ours, was giving him a lecture about taking every type of precaution to avoid catching a bug: basically told him to self-isolate.
So there’s no clear message. Maybe the nurses are being stricter with some people than others because they’re trying to assess relative risk. But I suspect it’s not that thought-through. Different nurses simply have different outlook on life, and the current risk the virus poses to cancer patients. Like we patients and families, they’re just struggling on in the dark, doing what they believe to be best.
If you want to share your experience of either providing or receiving cancer care during this COVID-19 epidemic, then please scroll down to the end of this page and leave a comment, or email us at [email protected]
Sources of advice and information
Some general information and advice for cancer patients and survivors regarding COVID-19 is available on the websites of many cancer organisations and charities, including:
ASCO has published a helpful “FAQ for clinicians” COVID-19 Clinical Oncology
The Cancer Letter is offering some helpful coverage aimed principally at clinicians, including a Guest Editorial on COVID-19 and the cancer patient: A call to action for balancing cancer care and viral risk.






1 comment
Comments are closed.