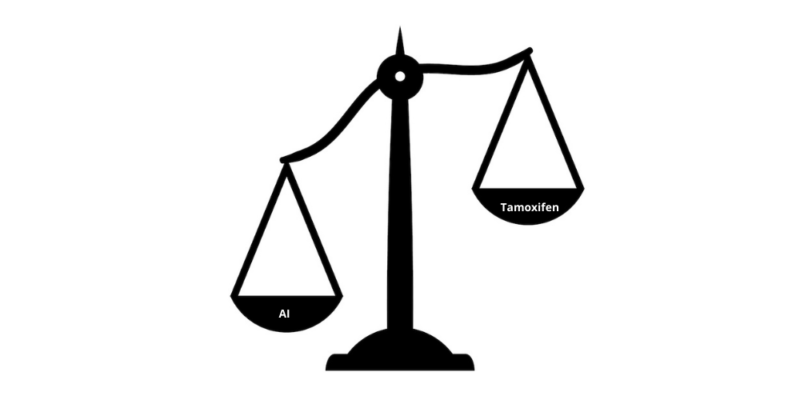
Giving aromatase inhibitors (AIs) instead of tamoxifen to premenopausal women with oestrogen receptor positive breast cancer, who have undergone ovarian suppression, significantly reduces risk of recurrence. The study, published in The Lancet Oncology (3 February), found that breast cancer recurrence was reduced by 21% and distant recurrence by 17% among the group receiving AIs.
“Our aim was to find out whether premenopausal women treated with ovarian suppression could benefit more from AIs than tamoxifen, and these findings conclusively show this is the case for preventing breast cancer recurrence,” says lead author Rosie Bradley, from Oxford Population Health, at the University of Oxford. “However, we need to follow patients for longer to find out whether breast cancer deaths are also reduced.”
For women with hormone-sensitive, operable breast cancer, giving tamoxifen treatment after surgery reduces risk of dying from breast cancer by around one third. AIs are even more effective in postmenopausal women where risk is reduced by a further 30%. In the absence of ovarian suppression AIs, which block conversion of androgens into oestrogens by targeting the aromatase enzyme, are ineffective for premenopausal women due to compensatory physiological responses inducing ovarian oestrogen. However, in premenopausal women treated with ovarian function suppression or ablation, this physiological response can be overcome. In contrast tamoxifen works by blocking oestrogen receptors on breast cancer. Studies have, however, demonstrated conflicting results over whether AIs or tamoxifen are more effective in premenopausal women treated with ovarian function suppression or ablation. “Guidelines generally already include consideration about ovarian suppression in premenopausal women but can be a bit vague about whether to add tamoxifen or an AI,” explains Bradley.
To better characterize relative benefits of tamoxifen and AIs, researchers from the Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) undertook a meta-analysis of individual patient data from four trials of 7,030 premenopausal women with early-stage oestrogen-receptor-positive breast cancer treated with ovarian suppression or ablation and randomized to AIs or tamoxifen. The AIs used were anastrozole in the ABCSG XII trial, exemestane in SOFT and TEXT and letrozole in HOBOE. Women were treated for either three years (ABCSG-12 trial) or five years (SOFT, TEXT, and HOBOE trials). Over all four trials, which took place between June 1999 and August 2015, median follow-up was eight years. Results show:
- Of 7,030 women included in the analysis, 888 (12.6%) had breast cancer recurrence and 418 deaths occurred (of which 54 were from causes unrelated to breast cancer),
- The rate of breast cancer recurrence was lower for women allocated AI than tamoxifen (RR 0.79, 95% CI 0.69-0.90, p=0.0005),
- Distant recurrence was reduced with AIs (RR 0.83, 95% CI 0.71-0.97; p=0.018),
- AIs were just as effective in women < 35 years, who have a higher risk of recurrence than older women,
- No significant differences were observed between treatments for breast cancer mortality (p=0.94), death without recurrence (p=0.34) or all-cause mortality (p=0.68),
- 6.4% of women in the AI group had a bone fracture in the follow-up period vs 5.1% in the tamoxifen group,
- A sub-group analysis showed recurrence reductions for AIs were seen in women with 0-3 nodes affected, but not in women with ≥ four nodes affected.
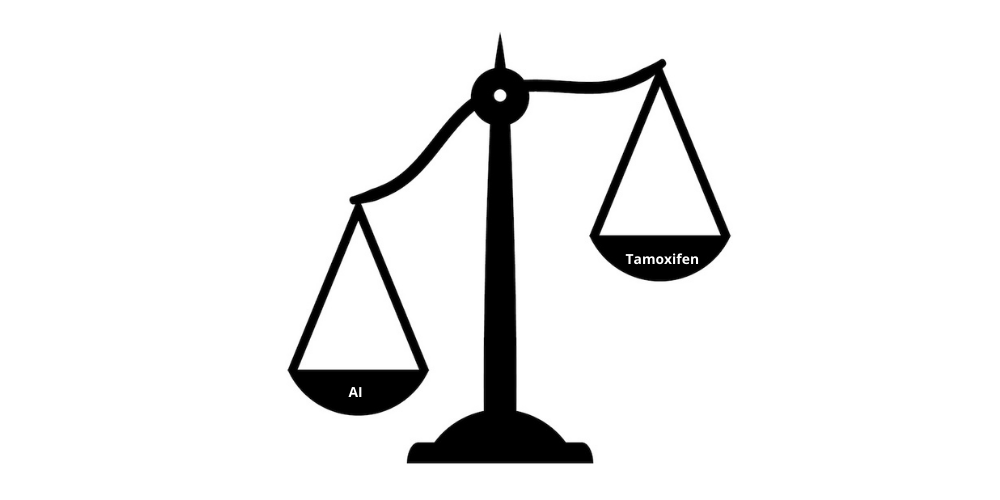
Although the meta-analysis found no difference in breast cancer or all-cause mortality between the treatment groups, the authors believe this may be explained by limited duration of follow-up (eight years). “Given the significant reduction in distant recurrence with aromatase inhibitors (p=0.018), it would be premature to conclude that survival is not improved with aromatase inhibitors,” write the authors.
The importance of long-term follow-up in breast cancer, they add, has been demonstrated by a previous EBCTCG meta-analysis of trials comparing adjuvant AIs versus tamoxifen in postmenopausal women which showed no significant survival advantage after a median follow-up of five years, but did establish reductions in breast cancer mortality and all-cause mortality when analysed later.
Two of the four trials included in the current meta-analysis are still following up the women in their trials. “EBCTCG would like to do a second meta-analysis of these trials with more mature data to reliably assess the impact of AIs plus ovarian suppression on breast cancer mortality compared to tamoxifen plus ovarian suppression. There is a great need for longer term follow-up of these trials to fully assess any impact on breast cancer mortality,” says Bradley.
Effects of endocrine therapy and ovarian function suppression on quality of life, she adds, will also need to be considered alongside improvements in disease outcomes. “There are known to be higher rates of osteoporosis in those receiving AIs while endometrial abnormalities are more frequent in those receiving tamoxifen,” says Bradley. Side effects, such as bone fractures, she adds, can be mitigated by use of bisphosphonates to preserve bone density and reduce fractures in women receiving AIs.
The most unexpected subgroup finding was apparent lack of superiority of AIs over tamoxifen in women with four or more involved nodes. “Studies in postmenopausal women found no suggestion of any difference in AI benefits according to number of lymph nodes affected. The lymph node finding in premenopausal women was unanticipated, and quite possibly a chance finding due to the large numbers of subgroups investigated,” says Bradley.