A patient visits their local primary care facility with symptoms that could indicate a possible cancer. What happens next could determine their chances of survival. In the event that it turns out to be a cancer, a quick and accurate diagnosis could be essential.
Primary care doctors can look and feel and make a judgement on the need for further investigation, but they have neither the equipment nor the skills to make the diagnosis. The question is whether there is diagnostic service that is reliable, affordable and not too far away, to which they can refer their patient. If not, the pathway that should lead the patient from their local doctor to accessing the treatment they need at a specialist hospital could be fatally broken.
While in higher income countries, issues of inequalities at the level of diagnostics focus primarily on access to molecular testing or even next generation sequencing, in sub-Saharan Africa, as in other resource-poor parts of the world, access to even basic histology and immunohistochemistry tests is extremely patchy.
The recently published Lancet Oncology Commission report on Cancer in Sub-Saharan Africa noted that, “Many potential patients with cancer have to wait for an initial histology then pay extra for further immunohistochemistry, resulting in major treatment delays, and, in many cases, stage shifts from curable to incurable disease.”
Lack of adequate pathology services is a significant factor contributing to the relatively poor cancer survival in Africa (see box), according to Isaac Adewole, a professor of gynaecology and obstetrics at the University of Ibadan, Nigeria, and one of the co-authors of the Lancet Oncology Commission report.
“Accurate and timely screening and early diagnosis could prevent thousands of cancer deaths in Sub-Saharan Africa,” he said. “However, in most countries in the region, referral systems are absent or inadequate due to poor infrastructure. Furthermore, unregulated laboratory practices have led to a plethora of misdiagnoses or late diagnoses.”
Building sustainable and accessible cancer pathology and diagnostics capacity will be essential to improving survival rates. Making that happen will require better recognition of the role of pathology within a cancer system, and of the extent of unmet need, which can be hidden by (largely unregulated) private pathology services available to the urban middle classes who dominate policy making.
Sub-Saharan Africa has some of the poorest cancer survival rates in the world
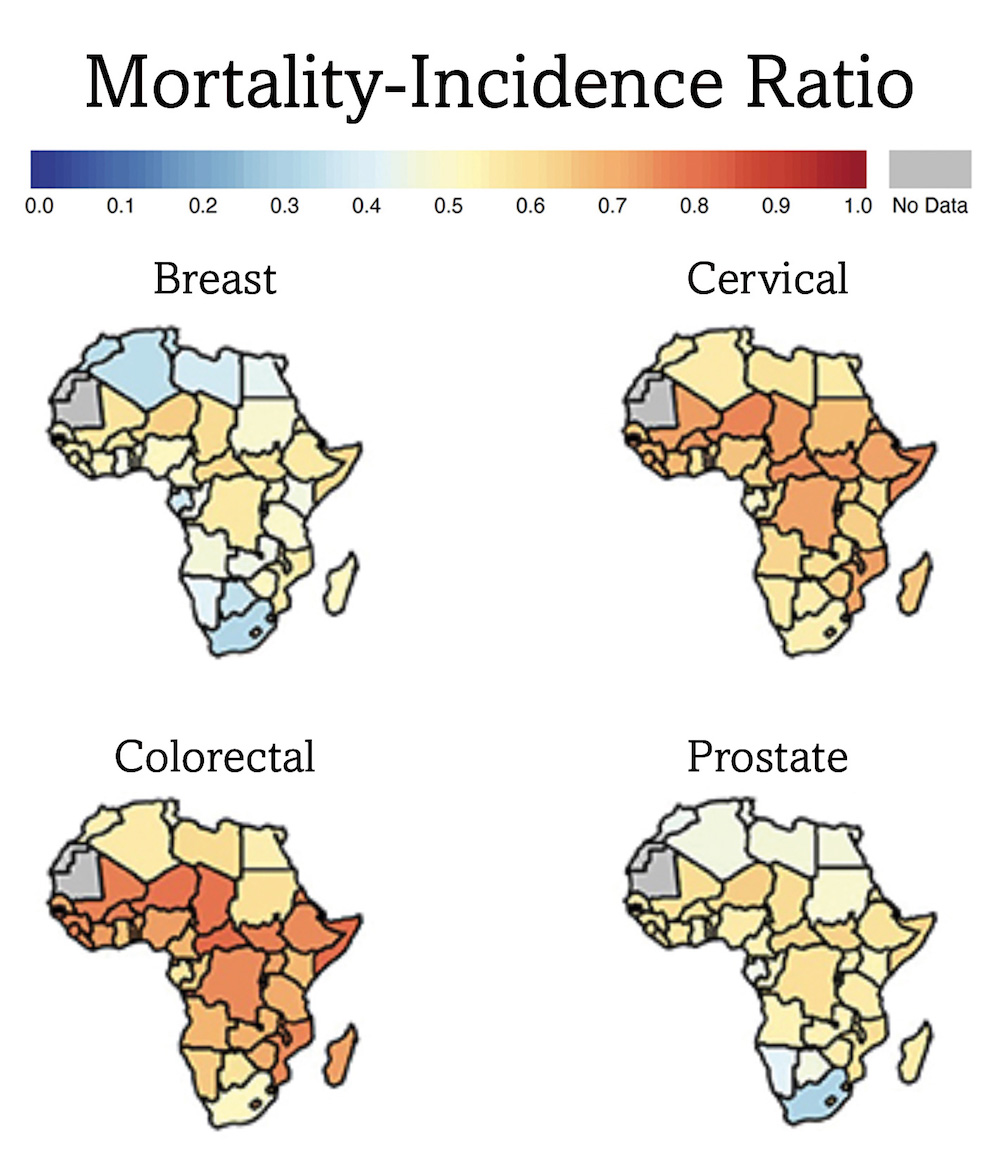
These maps, which show the ratio between deaths and incidence (a surrogate for survival) by country, for four main cancers, indicate that survival, particularly in sub-Saharan Africa (i.e. all but the most northerly countries on these maps) is much poorer than typical survival rates in high-income countries (not shown here). Lack of reliable and accessible pathology services is one factor, alongside public awareness, screening programmes and treatment capacity.
Problem? What problem?
A 2020 survey of 34 healthcare centres offering specialist cancer treatment services across sub-Saharan Africa, conducted by the African Consortium for Cancer Clinical Trials (AC³T), revealed that all sites were equipped to perform X-rays and ultrasound examinations and all bar two of them were equipped to perform CT scans. Two-thirds could also offer MRI scans, though only four were able to perform PET scans.
In terms of lab pathology, almost all (33 of 34) said they performed basic histology on suspected cancer samples, with 24 also performing immunohistochemistry and just over half performing flow cytometry .
It’s not perfect, but also not so bad ‒ so long as you happen to have access to the expert services of one of those centres. Many general hospitals are affiliated with specialist cancer hospitals in the area, and some have frequent visiting specialists or in-house specialists, says Omolola Salako, a Clinical Radiation Oncologist and university lecturer in Lagos, whose efforts to promote more equal access to cancer care in Nigeria earned her the Best CEO award from the Union for International Cancer Control (UICC) in 2020. But this tends to happen only within cities where these specialist centres are located, she says, with the result that cancer is better diagnosed in cities than in rural areas, where the majority of the population of sub-Saharan Africa reside.
In rural areas, when it comes to pathology, the capacity to harvest, store, transport, track, record and analyse samples, and the guidelines and quality control needed to support such a service, are very limited. It then comes down to local health workers take a piece of tissue or lump out of a breast or bowel or skin and put the tissue in a tube and use whatever means are available to send it wherever they can for analysis, and hope the harvesting was done right, the sample doesn’t degrade or get lost on the way, the analysis can be relied on, and that an answer comes back in time.
That rural‒urban divide becomes infinitely worse when you take into account private diagnostic services, according to Richard Sullivan, a Professor of Cancer Policy & Global Health at Kings College London and Director of the Kings Institute of Cancer Policy.
“Governments don’t often appreciate the importance of diagnostics, and it is taken for granted, because the private providers have filled this vacuum”
The pressure to get a timely and accurate diagnosis, if cancer is suspected, opens up a big market for private diagnostic services, he says, and profit margins can be high. But this is true only in geographical localities where the wealthy people who can afford to pay for their services live – the urban middle class elites and above.
“There is a massive distributional inequality,” says Sullivan, which becomes entrenched because policy makers live in areas with access to services. “Governments don’t often appreciate the importance of diagnostics, and it is taken for granted, because the private providers have filled this vacuum,” he says. “If all your diagnostics are privately provided, all in urban areas, they serve the political elites in those urban areas, therefore, they’re happy. So government asks: ‘Why should we provide lots of services in rural areas?’”
The problem is not just about costs and affordability, he adds, “It’s also how the money interfaces with politics.” One consequence is that few national cancer control plans in sub-Saharan Africa include provision for laboratory pathology and radiology services.
The attitude among some governments that “we have better things to spend our money on,” is one Sullivan finds quite frustrating. “I do understand the kind of arguments put to me which is: this is complicated, lots of competing interests… But if you haven’t got the diagnosis right, you cannot treat cancer correctly.”
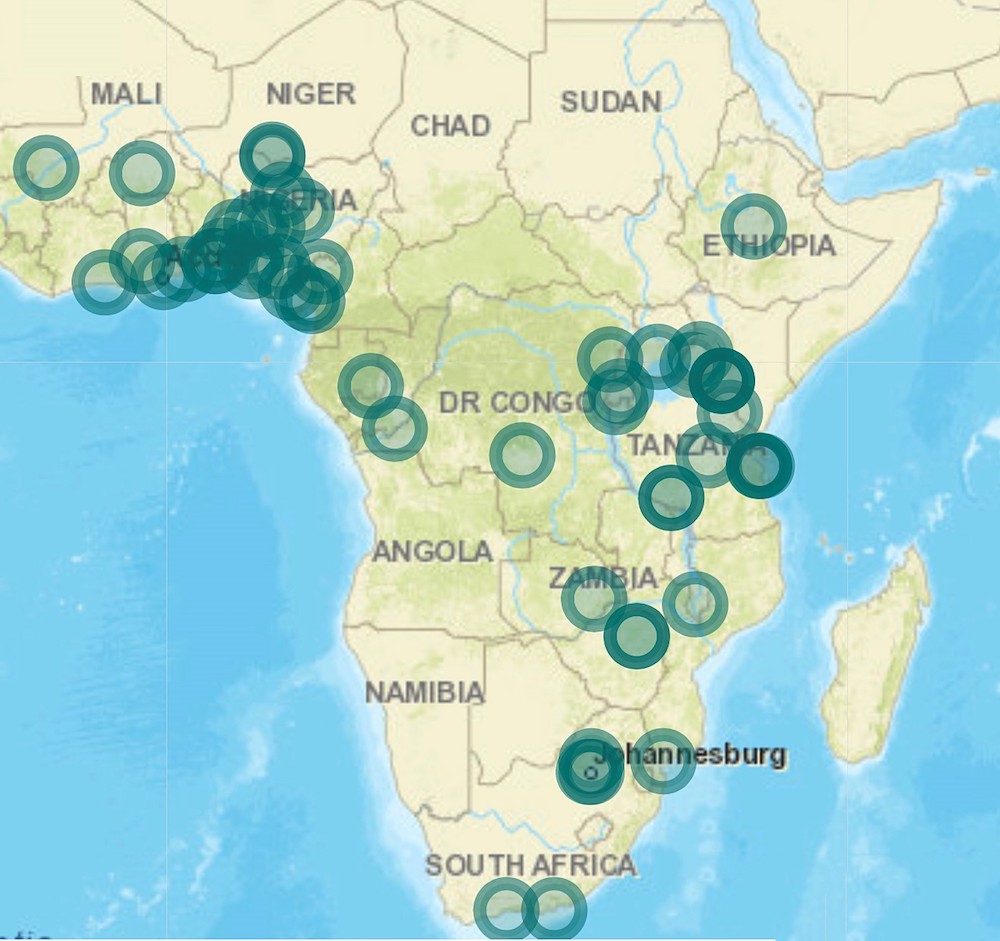
Distribution of specialist cancer treatment centres
This map shows the location of hospitals offering specialist cancer treatment that were surveyed by the African Consortium for Cancer Clinical Trials. It shows major disparities in access to specialist services, with large parts of the continent having no specialist facilities at all. Almost all hospitals featured on this map are located in major cities, while the majority of the population of sub-Saharan Africa still live in rural areas. Building cancer capacity at primary and community care levels, with effective referral pathways, is therefore essential to ensure people have the access the services they need, when they need it.
Towards cancer diagnostics for all
One approach to building cancer diagnostic capacity that is being tried in countries including Zimbabwe and Kenya, is to extend the remit of diagnostic infrastructure, such as the laboratories set up to support work around HIV, tuberculosis and malaria, many of which were set up with funding from the US President’s Emergency Plan for AIDS Relief (PEPFAR).
The potential contribution of these facilities can be seen, for instance, in the findings of a 2020 systematic review of the evidence relating to Routes to diagnosis of symptomatic cancer in sub-Saharan Africa, where Kaposi sarcoma ‒ strongly associated with HIV infection ‒ was reported to be the only cancer type that was definitively diagnosed “at various primary care-based specialist clinics”, before the patient was referred to a specialist cancer centre, For all other cancer types, “the definitive diagnoses of cancer were made by specialists in large tertiary healthcare centres.”
Having capacity to diagnose one particular type of cancer is very different from being equipped to accurately diagnose multiple different types and subtypes of cancer, so efforts to ‘repurpose’ these clinics to also handle cancer pathology is seen more as a temporary measure to overcome a systemic shortage problem. But the concept of “primary care-based specialist clinics” providing diagnostic capacity within the infectious diseases setting could be something to build on for cancer.
“We have created an ecosystem which encompasses three things: digital, medical expertise and artificial intelligence”
Developments in digital pathology and in the use of artificial intelligence to read diagnostic imaging or digitised pathology slides are also opening up new possibilities for overcoming geographic barriers to high-quality cancer diagnostics.
One new start-up looking to take a lead in that space is Data Pathology, a company specialising in pathology health-tech solutions, based in Casablanca, Morocco.
“We have created an ecosystem which encompasses three things: digital, medical expertise and artificial intelligence,” says the company’s co-founder, data specialist Mohammed El Khannoussi. After a biopsy is turned into a digitised image and sent to Data Pathology from a laboratory based anywhere in sub-Saharan Africa, it is shared on the web platform. “Our team of doctors provide a diagnosis. We also have artificial intelligence algorithms to help doctors diagnose faster,” he says. For instance, at Data Pathology, he claims, a diagnosis of cervical cancer takes just about 30 seconds, and using validated AI the accuracy is about 99%.
“What we are trying to do is to connect pathologists with local patients everywhere, because they need the service, but there is no one to do this,” says Khannoussi.
But while the expert analysis may be done remotely, an expert quality-controlled service is still required near the patient’s home, to harvest and handle and prepare the tissue, and to prepare the slides and carry out the digital scanning for uploading onto the Data Pathology web platform.
Currently the company provides analysis services to 10 private pathology labs across the continent, and they are currently looking to assist in setting up two new labs ‒ both in Francophone Africa. One of these will be in Djibouti, a country with a population of 2 million people which currently has no private pathology facility or specialist cancer treatment centre. The other is in the Democratic Republic of Congo, which has a population of 100 million, and only one centre that treats cancer ‒ the Mbujimayi Presbyterian hospital, which according to the African Consortium for Cancer Clinical Trials survey, “lacks a full-service pathology laboratory, though there is a pathologist working on staff.”
These labs will be connected to the ecosystem in Morocco.
In terms of cost, the service offered by Data Pathology, at around $50, is around a quarter of the cost of sending the same sample to Europe for analysis, says Khannoussi. Savings are made by minimising handling fees and avoiding the use of FedEx or other specialist air courier services ‒ on top of which, the expert pathologists they work with are cheaper, purely because they are local and don’t charge European rates.
Digital services like this one could well help make pathology services more affordable and accessible for many. The logic of the market, however, makes it unlikely that poorer people and those living in more rural areas will be the prime beneficiaries.
Responsibility for ensuring these people have access to reliable cancer diagnostics when they need it cannot be left to the market, says Sullivan. It is up to governments, which is why it is so important to convince policy makers that pathology is worth investing in. There’s still a lot of persuading to do, he adds, because pathology doesn’t have the status ‒ or the pay ‒ of other medical disciplines, despite requiring a full 15 years of study.
“Pathology is an orphan area, politically, economically and I would argue culturally as well. Pathology and laboratory medicine and radiology, which underpin diagnostics, are seen as technical and somehow there’s always a substitute … somehow you are seen as not a real doctor.”
“You have to you have to build basic pathology services and radiology services into your primary and district clinics”
The 2019 Lancet Commission report on diagnostics highlighted the need for advocacy to make the case for reliable and accessible lab pathology and diagnostic imaging services to be integral components of the cancer care pathway planning.
While those services do require high-level specialists, able to interpret the complex mix of diagnostic data that can have a bearing on clinical decision making, adds Sullivan, there is also plenty of scope for involving people with less expertise in basic diagnostic work, which may be better done much closer to home.
“You have to build basic pathology services and radiology services into your primary and district clinics,” says Sullivan. “I think you need a place where people can come to and they’re not going to pay out of pocket.”
“Medical technicians can be trained to quite a high degree in terms of doing diagnostics… People can be brought up to a level where they can make basic diagnoses,” he adds. “Nurses and community health workers, who are often underestimated, can also take on these basic cancer diagnoses, with sufficient training, and using a basic set of technologies, which have now gotten easier to use.”
Salako, the Lagos-based clinical radiologist, who is leading efforts to improve access to screening and treatment through a variety of digital health initiatives, is clear that definitive diagnoses will normally have to be done at a specialist centre. “We are not promoting cancer diagnosis at the primary health care level, simply because it’s a complex disease and it’s treated by specialists who are usually not available at that level,” she says.
But she is also a strong proponent of building capacity and expertise at a local level to deliver aspects of a cancer service that are best done closer to home ‒ which could include screening, early detection using basic diagnostic tools, and above all prevention.
“In an ideal situation, every community should have a community oncology centre or a community cancer centre for which the entire cancer continuum can be offered,” she says, “I’m an advocate for cancer care at the community level… We have to come down to that primary health care level and provide community clinics that are centres of excellence.” She gives a particular mention to information and support services on prevention. “That’s a key component because a big percentage of cancers are preventable.”
Technical innovations will be important here. An example mentioned in the Lancet Oncology Commission report is the GeneXpert platform, which uses plug-in cartridges to deliver molecular testing, for instance for the BCR-ABL gene that drives certain chronic myeloid leukaemias. It can also be used to screen for HPV infection, at primary or community healthcare centres, obviating the need to involve pathology labs and the associated storing, transporting and tracking challenges.
These sorts of innovations could make an important contribution, particularly for African women, who make up around one in seven of the world’s female population, but account for more than one in three of all deaths from cervical cancer.
The cost remains a barrier to rolling out to primary care in most resource-poor countries, however. The Lancet Oncology Commission report on Cancer in sub-Saharan Africa suggests setting up a ‘global alliance for diagnostics’ to “improve availability and affordability through market shaping”, and highlights the potential of including cancer tests in universal health coverage schemes, to improve access to these services.
Sullivan would like to see more research focused on access to diagnostic pathways in low- and middle-income countries. He argues for “a comprehensive research programme” to examine the role of primary care and other alternatives in cancer diagnosis, “as this may contribute to the development of possible diagnostic guidelines.” This could start with breast, cervical and colorectal cancers.
Salako needs no convincing about the contribution that digital health technology can make to transforming access to early diagnosis as well as prevention and care. The big issue for her will be getting policy makers to listen with open minds and be more flexible in their approach. “We just need the government to be more responsive, intuitive with adopting technology as a solution to the cancer care crisis that we have,” she says.