Key messages from the e-ESO faculty

On March 18, the European School of Oncology presented an interactive webinar on how to do this, drawing on the limited data available, the lessons from the Italian experience, and basic principles of good cancer care. The webinar on The Impact of Coronavirus on Oncological Care (18 March 2020) can be seen at e-eso.net.
The key messages are presented below.
The COVID-19 challenge
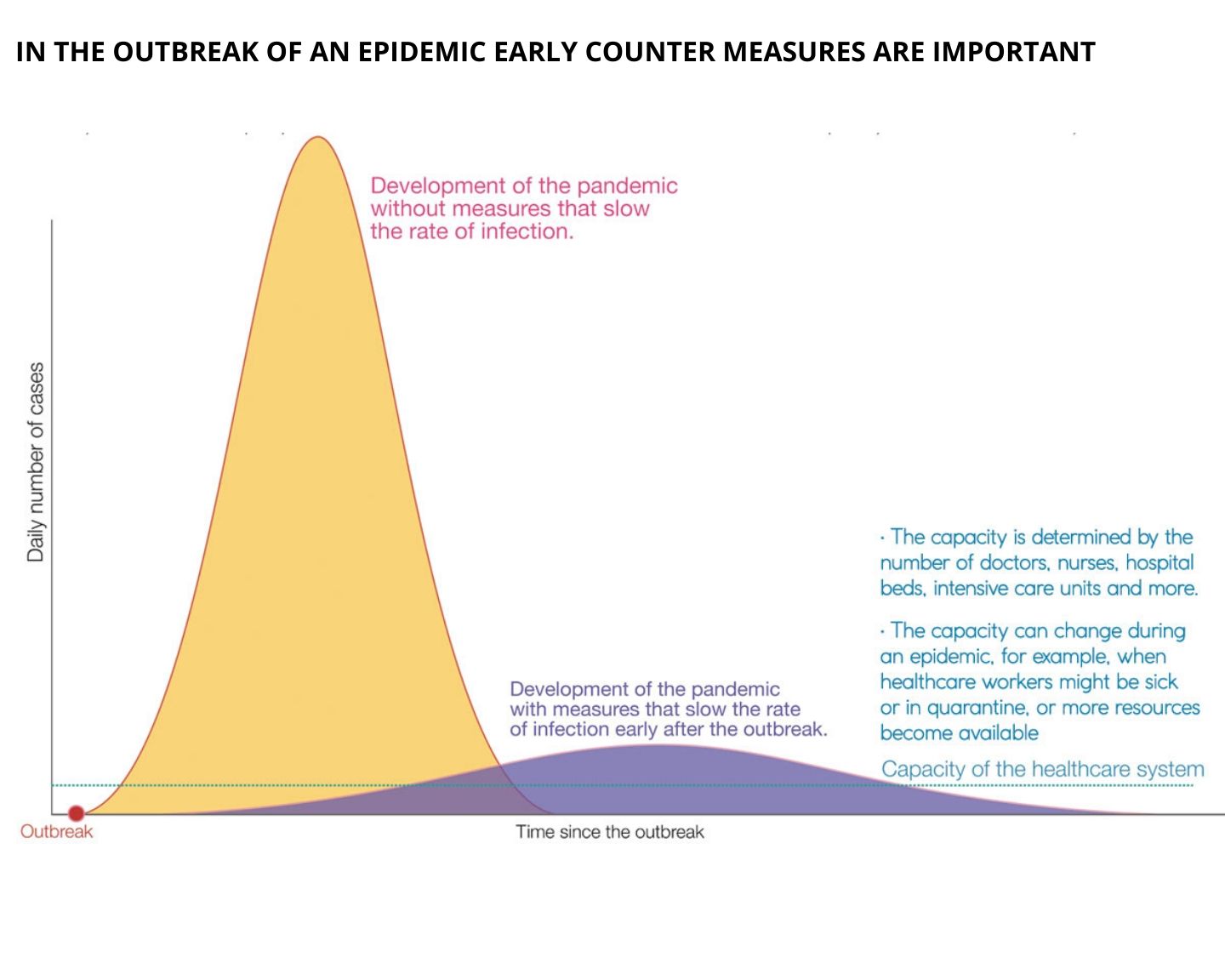
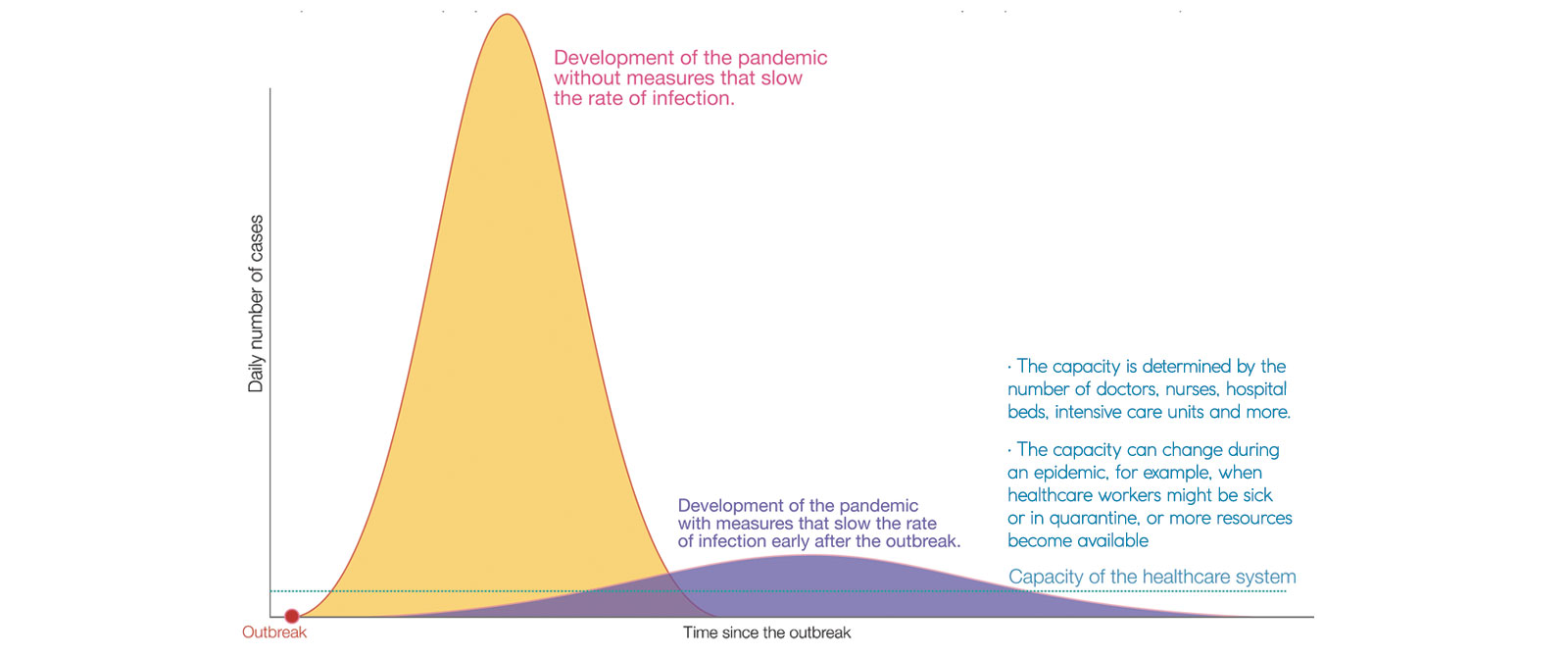
Coronavirus disease 2019 (COVID-19) is spreading across the globe, with Europe currently the epicentre. Health systems will struggle to cope. The Italian experience is not an exception, Italy is merely further along the curve of the epidemic. Intensive care units risk being overwhelmed by a surge of patients critically ill with COVID-19 complications. Cancer patients whose immune systems are compromised by their disease or treatment are at heightened risk.
- Cancer patients who contract COVID-19 are significantly more likely than the age-matched general population, to experience severe events including death. Data from China and Italy indicate that around half of cancer patients with COVID-19 experienced “severe events” (defined as admission to the ICU, the need for ventilation or death).
- In Italy the risk for hospitalisation with COVID-19 is around four times greater in cancer patients than patients in matched age groups without cancer. Most cancer patients hospitalised with the virus in Italy were within one month of surgery or chemotherapy.
- Patients with cancers or treatments that impact on their immune systems are at particular risk of experience severe events, including those with haematological malignancies, those being treated with chemotherapy, bone marrow transplant patients, and patients who have recently undergone surgery.
- There is little robust evidence on the best way to manage cancer patients during this epidemic.
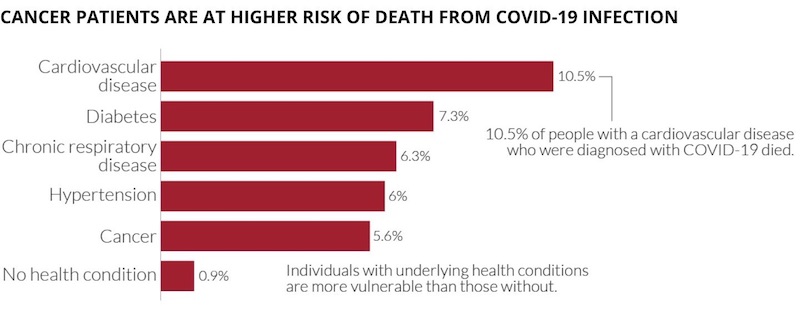
Data source: Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological aspects of an outbreak of 2019 Novel Coronavirus (COVID-19) ‒ China 2020. China CDC Weekly. Accessed at https://ourworldindata.org/coronavirus on 22 March 2020. Licensed under CC-BY by the authors.
Meeting the challenge:
The key messages from the e-ESO faculty are:
- Don’t panic.
- Plan ahead.
- Protect, inform and prepare staff and patients.
- Personalise management of patients. Weigh the potential benefit of the cancer treatment against the potential added risk of contracting COVID-19, working from the available data and experience and using common sense to apply basic principles of care.
Protecting patients and staff
Cancer services will need to provide existing and new patients with the best possible cancer care in safe conditions.
At population level
- Reducing the rate of new cases in the general population is vital to minimising exposure faced by cancer patients and other vulnerable people. The World Health Organization has issued guidelines on how to do this, based on the best evidence available, and many governments have issued their own guidelines and instructions. Oncology services should actively promote and follow that guidance
- Oncologists can play a role advocating for authorities and the general population to implement guidelines on social distancing, hand washing, and self-isolation following contact with a known case or on developing symptoms such as fever and cough.
Among cancer patients
- Oncology services should inform patients of the importance of following guidelines to minimise the chances of exposure, and what to do if they develop symptoms.
- Screening is not generally being recommended for all patients in the absence of symptoms that could suggest infection with COVID-19 (principally fever and cough).
- So far no prophylactic treatments have been identified that are effective to mitigate the risk of contracting COVID-19 or the severity of its symptoms.
- At this stage of the epidemic it is not advised to use a pneumococcal vaccine to protect patients with COVID-19 from developing pneumonia, as the symptoms from reaction to the vaccine would be hard to distinguish from symptoms of the virus itself.
At service level
- Follow-up visits should be cancelled or postponed for patients who can safely be managed via a phone consultation or telemedicine.
- If patients receiving palliative care are well followed by supportive and palliative care units outside the hospital, they can be taken care of at a distance. Advice can be given by phone or telemedicine.
- Selection of patients who really need to visit the hospital should be made by a senior oncologist who knows the patient well, according to a standard set of criteria.
- Treatment for cancer patients who develop serious COVID-19 symptoms should be concentrated in designated hospitals with all the necessary mix of expertise.
At in-patient/out-patient level
Patients and oncologists need to be protected from being infected when coming into hospital.
- The WHO has issued guidance for health workers (2 pages) on the rights and responsibilities of health workers, including specific measures needed to protect occupational safety and health.
- The WHO has also issued guidance on getting your workplace ready for the COVID-19 pandemic.
- Patients on active treatment should have separate access routes and waiting rooms at outpatient clinics to ensure the highest level of protection from exposure to the virus during their hospital visit.
- Visits by family and friends should be severely restricted. Where visits are allowed, protective clothing must be provided and worn.
- Access to high-quality personal protective equipment such as face masks, respiratory support devices and sanitising products such as hand disinfectant is essential, and urgent pressure is needed on all governments to ensure that is rapidly put in place.
- Oncologists can amplify at a national level the call ECCO has made to the EU and national level emergency planning structures to “direct the most urgent attention towards resolution of reported shortage of [such] critical healthcare equipment.”
- In addition to the standard recommendations of sanitising hands and equipment, staff on oncology wards should be encouraged to wear masks at all time, and also practice social distancing.
- Other sensible precautions include reducing the number of people attending tumour boards to a single rep from each team.
- Timely information and communication with team members is crucial to keeping everyone up to date and being able to manage in a rapidly changing situation.
- Regular staff meetings to discuss any symptoms, illness or logistical or other problems have an important role in maintaining the wellbeing of the whole department.
- Screening is not generally being recommended for staff in the absence of symptoms that could suggest infection with COVID-19.
Managing existing patients during the pandemic
At this early stage, any clinical guidelines have to rely more on observational data and the experience of countries like China and Italy.
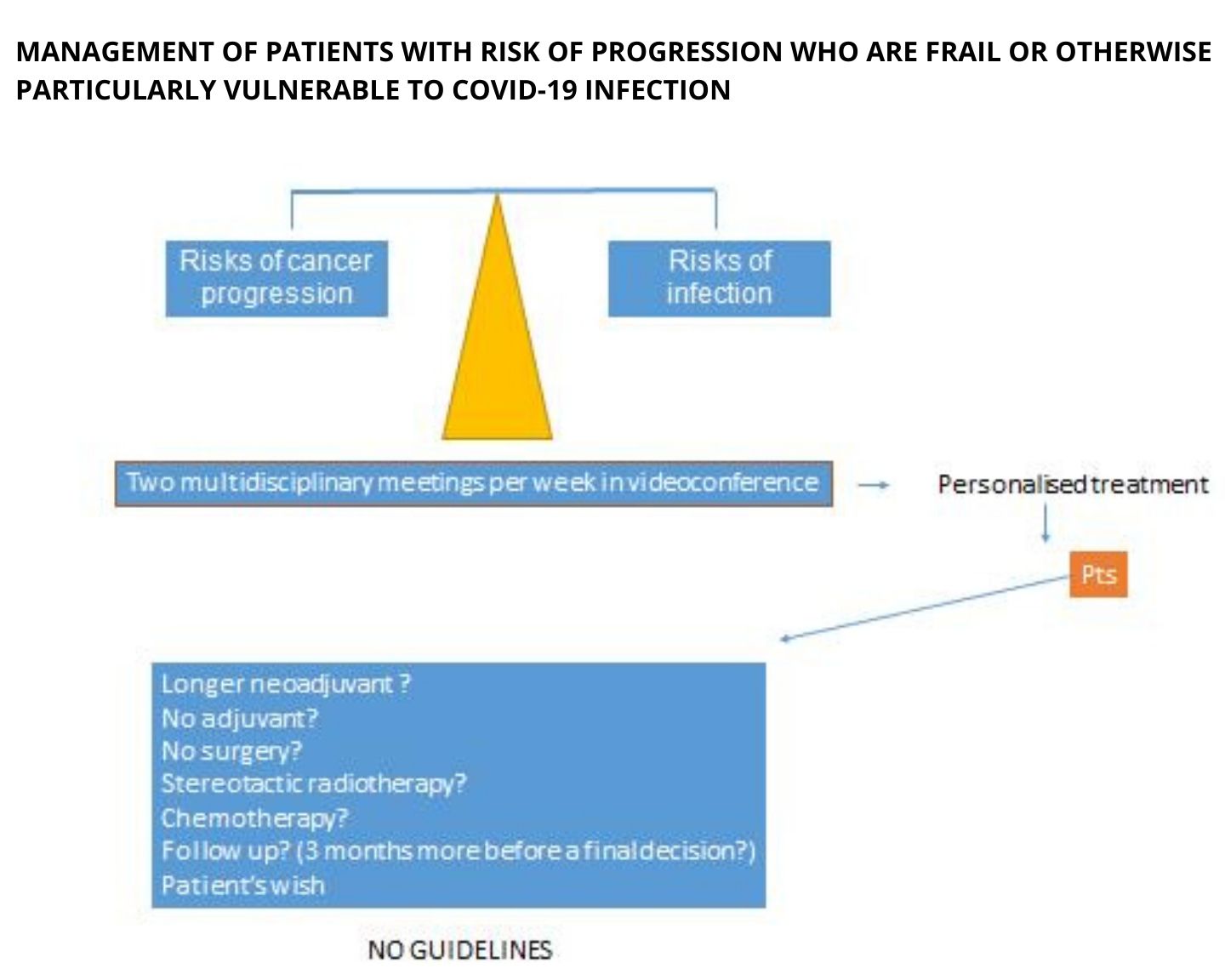
The general principle is to balance the risk of cancer progression against the risk of infection.
- As a general rule, and where adequate precautions are in place, it is important to continue cancer treatment rather than delay for fear of infection. This is the clear message coming from most institutions that have published guidance, including the NCCN (US National Comprehensive Cancer Network), and ASCO. There is no evidence to indicate stopping or changing a certain type of treatment a patient is receiving just because they might get infected with the coronavirus.
- Use clinical judgement and individualise treatment decisions, as always. Consider the prognosis of the patient: what is the chance the therapy will really help them? In the curative setting or even adjuvant and neoadjuvant setting, it is important not to compromise potentially large benefit.
- As usual, all decisions should be reached in full and open discussion with the patient.
CLINICAL JUDGEMENT & PERSONALISED DECISION MAKING IS KEY
- In the case of a patient undergoing treatment for metastatic testicular cancer, for instance, the recommendation would be for treatment to proceed as normal.
- Recommendations on adjuvant chemotherapy should also take into account the potential benefit, which is greater for instance where a breast cancer is HER2+ or triple negative, than for ER+ breast cancer.
- Recommendations on palliative therapy should also be individualised. Some patients receiving palliative chemotherapy may derive marginal benefit and have many other symptoms. In such cases the benefit of giving another cycle of treatment may not justify the added risk.
AVOID OVERTREATING
- Avoid overtreating patients who are frail, who have symptoms from other comorbidities, and who are not looking to prolong their life at whatever cost to their quality of life.
- It is essential that conversations about how patients want to manage their end of life are had early on in the course of their treatment.
- The information needs to be clearly marked on their notes to ensure that ER colleagues do not spend precious time and resources giving treatment to people who have clearly indicated they do not want it.
- If limited capacity means some patients need to be prioritised over others, and in the absence of any political guidance, oncologists will have to weigh up the risk‒benefit equation for each individual patient. It is important to be honest in team discussions and discussions with the patients about how the benefit they might derive compares with the benefits for other patients competing for the same resources.
- This will be a particularly stressful time for patients. It is important to take time to listen and help them manage that stress.
MANAGING PATIENT STRESS
- Where counsellors and psycho-oncologists are available, those resources should be used.
- However, these colleagues are more used to dealing with other cancer-related issues than this kind of situation, where there are so many unknowns.
- The important thing is to be there for your patients. If patients call because they are worried, take the phone yourself, do the triage, and calm them down.
- If survivors are worried, they should be reassured that there is no evidence that they are at greater risk than the general population, and they should follow the WHO guidance on what to do if they have been exposed to known cases or develop symptoms.
Managing newly diagnosed cancer patients during the pandemic
Decisions on initiating treatment in newly diagnosed cancer patients should be made using the same approach as for existing patients.
- No one should be excluded from starting treatment merely on account of fears of contracting COVID-19 if the potential oncological benefit is clinically significant ‒ if it is potentially curative, or effective against metastatic disease, or if there is an immediate need for palliating symptomatic disease.
- However, the decision must be personalised, in discussion with each patient, according to the risk‒benefit factors of the patient and their disease.
- There are no guidelines, and decisions are made on the basis of basic principles, ethics and common sense, with thorough discussions involving all multidisciplinary team members, taking the patient’s own wishes as the starting point.
- During the pandemic, it is important to take into account the massive added pressure on Intensive Care Units.
DON’T COUNT ON INTENSIVE CARE UNIT CAPACITY
- The huge demands the epidemic is putting on ICU capacity should be taken into account in weighing up risks and benefits of different treatment options.
- Clinical decisions on selecting patients for immediate surgery, for instance, should use risk models for morbidity and mortality, such as the European (Brunnelli) criteria for lung resections.
- Surgical resection of early stage NSCLC, for instance, can be curative without the need for chemotherapy or radiotherapy. In selected patients, this treatment should not be delayed during the pandemic where there is a low risk they will need to be transferred to intensive care following surgery.
- Decisions on whether to delay or not should depend in part on what stage the COVID epidemic has reached, and estimates of how soon the pressure on intensive care units may reduce – which are currently very uncertain.
- At the IOSI Lung Cancer Centre in Southern Switzerland, the discussion is whether to go ahead immediately, or to keep the patient under constant review to delay the surgery until the first wave of the epidemic has receded, relieving the pressure on intensive care units.
- One option being considered in these cases is to prolong neoadjuvant treatment while the surgery is delayed, or to use stereotactic radiotherapy as an alternative to surgery.
Diagnosing and managing patients who develop COVID-19
Cases of cancer patients developing COVID-19 will happen and cancer services will need to be prepared to manage them.
- Patients suffering from active cancer are at much higher risk than the general population of experiencing severe events in the event of COVID-19 infection, due to ongoing treatments and potential immunosuppression.
- Symptoms of COVID-19 can be difficult to differentiate, for instance, from symptoms derived from immunotherapy toxicities.
- Protocols and pathways must be in place defining exactly where to take the patients, what to do, what the next steps are.
- Treatment of cancer patients with COVID-19 should ideally take place in designated specialist centres, with input from specialists in treating the virus and its complications, as well as from the oncology team.
- There is little evidence to guide management of cancer in patients with COVID-19. Many important prospective studies are now being undertaken, but it is unlikely that the results will be available in time, at least for the first wave of the epidemic.
- Basic principles indicate that administration of immunotherapy should be stopped for patients diagnosed with COVID 19 because of the risk of enhancing immune-response leading to acute respiratory distress syndrome (ARDS) – a common and potentially fatal complication of COVID-19. The possibility of starting the patient on steroids, to damp down that immune response, should be discussed early.
- The cancer community will need to share experiences and evidence using online platforms to try to rapidly share experience, data, and evidence as it becomes available. e-ESO and other platforms offer webinars that can potentially be of value in this setting due to rapid organisation and free worldwide access.
- Fast track approval and early online publication of data is another way to go











1 comment
Comments are closed.