In a 2016 Voices post, Geta Roman wrote about the daily struggle to deliver timely and high-quality diagnostics and care in a health system with a per capita healthcare expenditure of only €400 a year ‒ the lowest of any European country.
With the coronavirus crisis now testing the resilience of even the best resourced healthcare systems, she asked cancer professionals and advocates how services for Romania’s 120,000 cancer patients are being affected.
Safety first
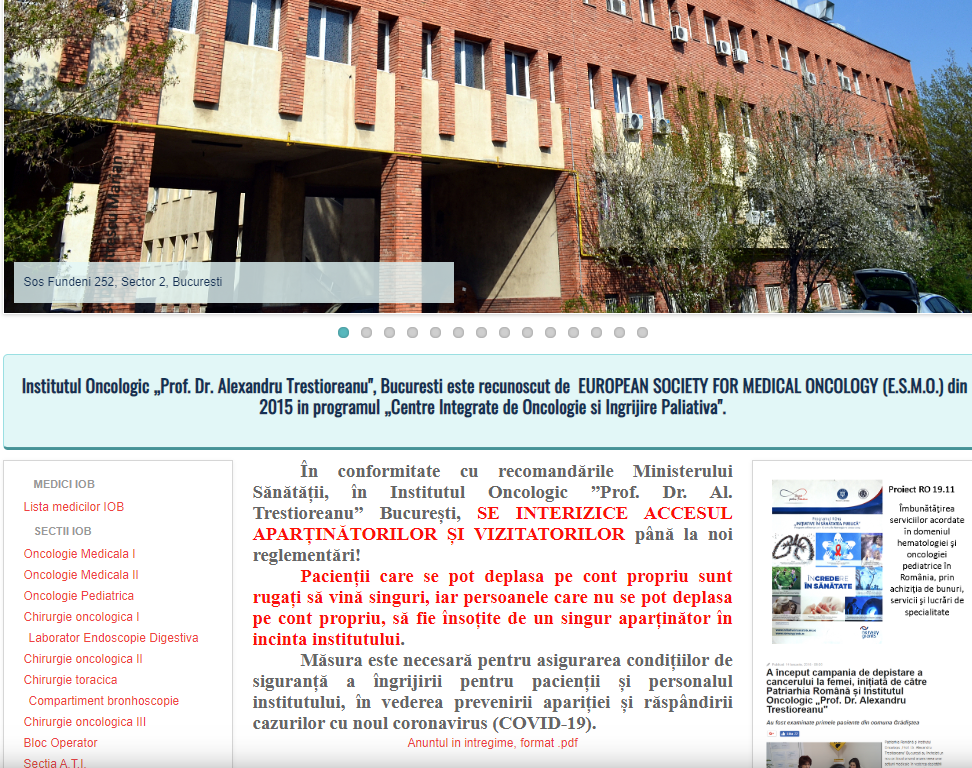
Strong measures are in place to safeguard staff and patients from exposure to the coronavirus, at least in the main cancer centres in Bucharest, Cluj and Iasi, according to one cancer nurse who works at Bucharest’s Prof. Dr. Alexandru Trestioreanu Institute for Oncology.
Staff work with personal protective equipment “a special mask, protection for the eyes and gloves,” and they work in shifts, she says. This is partly to reduce the number of staff on site at any one time, to make it easier to maintain social distancing, and partly because staff numbers are markedly down, as people with potential COVID symptoms self-isolate to minimise the chances of spreading the infection.
While the system works well, she says, “Our activity is clearly less than before.”
To further reduce the risks of infection, visitors are no longer permitted and patients are not allowed to bring anyone to accompany them when they attend consultations or treatment sessions.
Surgeries and CT-scans are postponed
In general, it seems that patients who are already on treatment are still following the protocol for their chemotherapy. However, while surgery for some cancer patients is continuing, it is less than before. Many non-emergency surgeries have been delayed, and a new protocol requires that all cancer patients who need surgery must be isolated and tested for COVID 19, twice, before the operation.
Cezar Irimia, President of the Federation of Cancer Associations of Romania, says the delays are a matter of concern. “From my point of view there is a big problem because a lot of surgeries are postponed. Patients are following the chemo treatments, but delaying the surgery, the effect of the treatment will be lost.”
Delays to imaging investigations are another major worry, he says. “We’ve had complaints from patients who received calls telling them their appointments have been postponed or cancelled.” The reason for these cancellations is not clear. “I suspect they are afraid to continue investigations because of the risk of spreading the coronavirus,” says Irimia, who adds that many scheduled appointments at oncology hospitals are also being cancelled or postponed.
While the Federation of Cancer Associations of Romania backs measures to reduce the risk of exposing patients to COVID-19 infection patients, it has stressed the importance of appropriate safety measures that can allow diagnostic and treatments to carry on as far as possible. Irimia says it was the patient groups who insisted that all cancer patients who go for treatment and surgery are tested for COVID-19.
He has been impressed by the way some of the large cancer institutes have responded to the challenge, but he says that, away from the major cities, smaller hospitals are struggling. “The Oncology Institute in Cluj took the lead,” he says. “I must say that they are really well organised. Some older problems we had are still here ‒ we do not have enough oncologists, some basic medication is not available. In smaller cities there are problems ‒ in Onesti, for instance, the local hospital was dedicated to COVID-19, so cancer patients have had to find other places to follow their treatments. There are not enough places for bronchoscopies, and pathology services are limited as well.”
Bringing healthcare delivery into the digital age
The impact of the coronavirus on patient care has not been all bad, however, says one oncologist from Bucharest’s Prof. Dr. Alexandru Trestioreanu Institute for Oncology. One change welcomed by many, she says, is that prescriptions can now be issued online, so patients do not have to visit their oncologist every time. “We reduced the number of patient visits, and they mainly come if they are on treatment. Those who need consultations send us their investigations by email, and in case of progression we call them to come to the hospital. If they are in good shape, we schedule a visit in three to six months… We are organised very well to limit our patients’ movement. We work in an incredibly fast rhythm so that they can spend less time in the hospital when they need to come to us.”
Oncology centres are also working with GPs to deliver care closer to the patients’ home where possible, she says, which many patients may find preferable, particularly at a time when new regulations oblige them to make the journey to consultations unaccompanied by a friend or relative.
Most commentators would agree that greater use of digital communication and a move to deliver more care closer to the patient’s home are important moves in the right direction for Romania’s cancer services. However, the speed of change means that GPs and other local services may lack the training and preparation to take on more of a role in caring for cancer patients, while patients themselves may feel scared and abandoned by the steep reduction in face to face contact with their oncologists. A question for the future is how these changes will play out as Romania’s cancer services emerge from the coronavirus emergency.
Cancer and COVID-19 deaths
So far (April 30th 2020) almost 700 deaths from COVID-19 have been registered in Romania. Almost 10% of them were cancer patients, according to official data provided by the Romanian Centre for Prevention and Control for Transmissible Diseases.