This year European Cancer Nursing Day ECND2020 on 18 May will be special because this is the World Health Organisation’s Year of the Nurse and Midwife; but also because it takes place in the midst of the current COVID-19 crisis.

Months ago, before the pandemic, EONS decided that the theme of ECND2020 would be the principle of Universal Health Coverage and the need to address inequalities in access to and utilization of good quality healthcare. For us, the key issues are nursing workforce shortages, the lack of specialist cancer nurses and poor supplies of Personal Protective Equipment (PPE) in different Member States. The COVID-19 crisis not only exacerbated all these issues but it also led to the rise of new ones and so our theme is unchanged, and perhaps even more relevant.
The numbers on COVID-19 demonstrate that its impact is associated with socioeconomic criteria. Therefore, it appears to be having a greater impact on low income groups, who tend to show higher rates of diabetes, cardiovascular disease and chronic respiratory disease, and often live in more crowded accommodation, heightening vulnerability to the virus. So too, the COVID-19 crisis presents extra challenges for cancer nurses and their patients, as most are classified as being vulnerable groups primarily due to the compromise of their immune system.
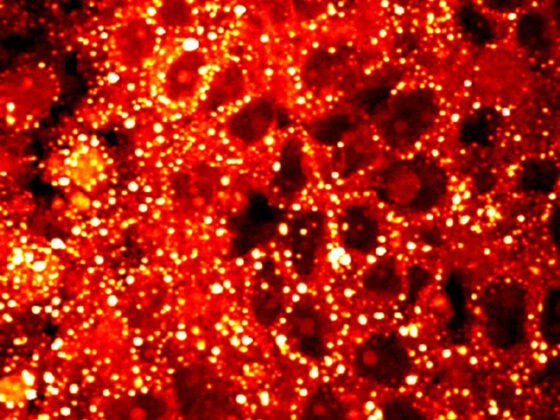
Compromised care
Many cancer nurses are being transferred to assist over-stretched general nursing teams, while others are having to support their patients in very challenging circumstances. The way that cancer care is been delivered to patients needed to go through significant changes so that the patient is not exposed to contracting COVID-19 throughout the cancer care continuum. Cancer patient treatments are sometimes being delayed or cancelled and tele-consultations have become the norm for immunosuppressed patients.
Johan de Munter, a hematology nurse consultant at Gent University Hospital, Belgium, and EONS President Elect, points out the dangers of such compromises: “This way of contact cannot replace all face-to-face consultations where crucial observations and psychosocial support need to be provided for our patients – and postponing a healthcare visit when key signs and symptoms occur or when side effects emerge, or postponing cancer treatments or follow-up visits, can all be associated with increasing health risks for patients with cancer.”
COVID-19 and the cancer ward
Every day, I am hearing worrying reports from cancer nurses on wards across Europe. Former EONS Board member, Sara Torcato Parreira, a specialist oncology nurse working at the Oncology Day Unit at CUF Infante Santo Hospital, in Lisbon, told me about the impact the virus is having in her ward, and how it is showing up some deep systemic problems:
“Covid-19 has brought difficulties and uncertainty in cancer care. Safety is now more important than ever. New strategies have had to be implemented to ensure that we are able to continue to diagnose and treat patients and maintain safety and quality in the care we provide. We work more hours and we get tired more quickly, due to stress, PPEs and because we try to rotate teams, working with minimal resources. And this is hard when we already had a lack of health professionals and infrastructure to treat cancer patients. We need to have enough professionals so that we and our patients can stay safe. Cancer care cannot and must not stop.”
The ‘invisible’ patients
Within the cancer nursing community there is growing concern about people with suspected cancer not presenting for diagnosis and treatment: in some countries rates of new diagnosis are estimated to have dropped by 80%. This is a time-bomb for healthcare systems already overloaded with COVID, and a grave danger to these patients. Again, EONS members report a very worrying picture. A senior UK cancer nurse working on the front line who wished to remain anonymous has already seen a significant rise: “I cannot believe the number of people we are already seeing with new cancers that should have presented a while ago,” he told me.
The picture is the same right across Europe. Head of the Stockholm-Gotland Cancer Centre, Sweden, Lena Sharp (EONS Past-President), reports “a substantial drop in cancer patient diagnosis over the last month, which is completely abnormal and indicates that people are staying at home rather than seeking medical advice – decisions which may increase the cancer burden and at worst, cost them their lives.”
Wendy Oldenmenger, a cancer nurse from the Netherlands recently returned to clinical practice from academia in order to support the increased demands of the pandemic, was driven to make this appeal: “Anyone with existing or suspected cancers should not be afraid to contact and visit health care settings. Trust in your healthcare workers to do everything they can to keep you safe. Do yourself and your healthcare system a favour by preventing the higher personal and economic costs of delaying treatment.”
So, we can see that the pandemic is transforming cancer care in real time, with implications for patients, healthcare workers, policy makers and all sectors of the healthcare industry. However, the solutions will, to a large extent, be the same ones EONS has been calling for over a number of years:
- minimizing cancer nurse shortages by investment in improving working conditions, providing a commensurate financial income and protecting and promoting individual well-being
- recognizing cancer nursing as a separate specialty and ensuring specialist qualifications for cancer nurses across the EU, based on the EONS Cancer Nursing Education Framework
- legally requiring Member States not to compromise on safety equipment and working conditions which threaten patient and occupational safety.
EONS Cancer Nursing Index
The EONS Cancer Nursing Index, launched to mark ECND2020, is a valuable tool which highlights where more needs to be done to address health inequalities in Europe, by indicating where specialist cancer nursing is absent, or available, and assessing standards of occupational and patient safety. ]Appreciative words and applause are not enough. The scale of the impact from the pandemic is largely unknown and unprecedented, with the aftermath however showing that change across all levels of healthcare is now more than ever necessary. Issues such as safeguarding the healthcare workforce and the patients have been elevated as vital priorities to assure continuation of care and effective management of the pandemic. It is only by fully supporting, investing in and recognising all parts of the multi-professional cancer care team – with nurses at its heart – that the battle for universal healthcare will be won. The COVID-19 crisis has demonstrated that deferring action has the most serious of consequences. The time to act is now.
* Support our ECND2020 campaign at #ECND20go4EQUALITY