Throughout human history, the search for a universal cure has captivated the minds of philosophers, healers and scientists across time and cultures. In Greek mythology, the goddess Panacea was believed to possess a potion to treat all afflictions. We still use the term ‘panacea’ to refer to a single remedy that can solve all problems. However appealing this may sound, the concept of a universal cure comes with a complex mix of ethical and philosophical challenges, hopes, and fears.
In recent years, a new class of drugs has dominated the headlines, promising improved health outcomes across an expanding range of conditions, including type 2 diabetes, obesity, cardiovascular conditions, cancer, depression, and addictions. Medications such as Ozempic (approved for managing poorly controlled type 2 diabetes) and Wegovy (approved for some people with weight-related health problems or obesity), which contain semaglutide as their active ingredient, have been hailed as a new milestone in medicine, of similar magnitude to antibiotics and vaccines. They have also sparked animated public discussions and debates, especially in their use as anti-obesity drugs.
Reports of potential adverse mental and physical effects, often merely anecdotal, are constantly investigated by regulatory agencies, healthcare professionals, and researchers to ensure patient safety and to better understand the full range of this medication’s effects. The ‘gold rush’ to access this ‘magic’ weight-loss pill has depleted the supplies in pharmacies, creating significant challenges for patients who rely on these medications for diabetes management.
It has also fuelled a growing black market, with unauthorised sellers offering counterfeit versions online. The World Health Organization has issued warnings about these fake products, which pose serious health risks to consumers. Costs of the treatment, which generally must be taken for life, are also an issue, for instance in the United States, where insurance coverage is often limited or unavailable, especially for weight loss.
Those caveats aside, however, the emergence of this new option, in particular to treating obesity, is attracting considerable interest among medical communities focused across the many different health conditions where overweight and other metabolic issues play a significant role. These include not just diabetes, but also cardiovascular disease and cancer, for which obesity is now set to overtake smoking as the highest risk factor in many countries. By addressing obesity, semaglutide improves not only body weight but also overall metabolic health, reducing the risk of these associated conditions.
Clinical trials, notably the STEP (Semaglutide Treatment Effect in People with Obesity) programme, have shown that this drug induces substantial weight loss, often exceeding 10–15% of total body weight in patients. In the STEP 1 trial, for example, participants treated with semaglutide 2.4mg once weekly experienced an average weight loss of 14.9% over 68 weeks, compared to 2.4% in the placebo group. This degree of weight reduction is unparalleled in pharmacological treatments for obesity, and is comparable to bariatric surgery outcomes.
How semaglutide works
Semaglutide belongs to a class of drugs known as glucagon-like peptide-1 (GLP-1) receptor agonists, also referred to as incretin mimetics. These medications emulate the action of GLP-1, a hormone naturally produced in the gut in response to food intake. GLP-1 plays a fundamental role in regulating blood glucose levels by stimulating insulin release, suppressing glucagon secretion, slowing gastric emptying, and reducing appetite (including via action on GLP-1 receptors in the hypothalamus, the brainstem, and regions involved in the brain’s reward system). The first GLP-1 receptor agonist, exenatide, was approved by the US regulators, the FDA, in 2005, marking a significant advance in diabetes treatment. Semaglutide represents a more recent and powerful iteration of GLP-1 receptor agonists. Its innovative structural design gives the drug greater stability and effectiveness and a longer half-life, than its predecessors. The drug was initially developed as a long-acting alternative to liraglutide for type 2 diabetes, getting FDA approval for this indication in 2017, under the brand name Ozempic. Semaglutide’s effects on reducing appetite and reducing the rate at which food is absorbed also make it a powerful tool for inducing significant weight loss. In 2021, manufacturers Novo Nordisk got approval for the drug to also be used for the chronic management of obesity, under the brand name Wegovy.
What might semaglutide offer cancer prevention and treatment?
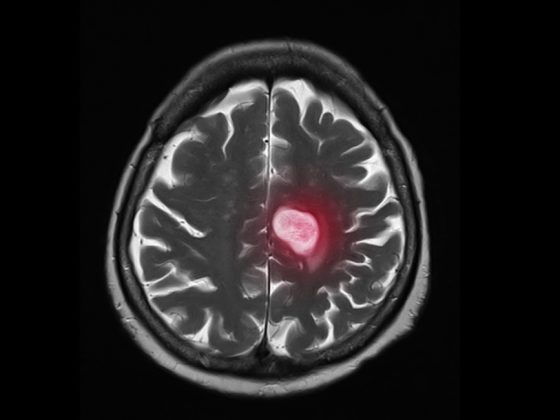
Obesity is a well-established risk factor for several types of cancer, including breast, colon, pancreatic, and liver cancers. Excess body weight promotes a pro-inflammatory environment, increases insulin levels, and leads to hormonal imbalances, all of which can contribute to cancer development.
Given semaglutide’s ability to induce significant weight loss and improve metabolic health, researchers have begun investigating its potential to reduce cancer risk. In addition to showing substantial weight loss, the STEP trials demonstrated improvements in several metabolic parameters, including reduced inflammation and better insulin sensitivity. By lowering insulin levels and systemic inflammation, semaglutide may help create a less favourable environment for tumour initiation and progression.
GLP-1 agonists are not the only modern anti-diabetic treatments repurposable in oncology. Metformin, a very common medication for type 2 diabetes, was the first bona fide antidiabetic drug to gain attention for its potential anti-cancer properties. Epidemiological studies have suggested that patients taking metformin have a lower risk of developing cancers, compared to those on similar medications.
Metformin lowers insulin and insulin-like growth factor (IGF) levels associated with cell growth in certain cancers. It is also an AMPK activator and mTOR inhibitor, both of which can play a role in cancer.
Several clinical trials have been conducted to evaluate metformin in cancer treatment, but results are still controversial. Research has demonstrated that semaglutide and other GLP-1 receptor agonists exhibit direct anti-tumour effects by inhibiting cancer cell proliferation and promoting apoptosis. For instance, in studies using pancreatic cancer cell lines, liraglutide (another GLP-1 receptor agonist similar to semaglutide) was found to suppress cell growth and induce programmed cell death by modulating the PI3K/AKT signalling pathway. Similarly, investigations into breast cancer cells and a mouse model revealed that GLP-1 receptor agonists reduced cell viability and migratory capacity, possibly through its influence on inflammatory mediators.
In animal models, treatment with semaglutide led to a significant reduction in tumour vascularisation and blood vessel density, potentially limiting the tumour’s ability to grow and spread. Furthermore, preclinical studies have indicated that semaglutide and other GLP-1 receptor agonists may enhance anti-tumour immunity. Research in mouse models demonstrated that semaglutide treatment increased the infiltration and activation of natural killer cells in tumour tissues. In vitro experiments also showed that semaglutide enhanced the cytotoxic activity of natural killer cells against cancer cells, suggesting a potential boost to the body’s natural defence against tumours. By improving insulin sensitivity and reducing hyperinsulinemia, semaglutide could decrease the levels of growth factors that promote cancer cell proliferation. This metabolic modulation may create a less favourable environment for tumour growth and development.
Researchers are particularly interested in exploring semaglutide’s effects in cancers associated with metabolic disorders, such as non-alcoholic fatty liver disease and non-alcoholic steatohepatitis, both of which are risk factors for liver cancer. Early studies suggest that semaglutide may reduce liver fat and inflammation, thereby lowering the risk of liver cancer in at-risk populations.
However, there are still concerns about semaglutide’s long-term safety with respect to certain cancers. Early studies in animal models raised the possibility of an increased risk of thyroid C-cell tumours, including medullary thyroid carcinoma. While this risk has not been definitively proven in humans, semaglutide is contraindicated in individuals with a personal or family history of thyroid cancer. Similarly, while some studies suggest that semaglutide may protect against pancreatic cancer, others have raised concerns about the potential for GLP-1 receptor agonists to increase the risk of this cancer in patients with diabetes.
The long search for a weight-loss drug
Awareness of the health risks associated with being overweight dates back at least four and half millennia (see box below). The search for pharmaceutical remedies, however, only started around one hundred years ago, with the advent of dinitrophenol (DNP) in the 1930s.
Originally developed for use in explosives and dye production, DNP was found to stimulate thermogenesis by uncoupling oxidative phosphorylation in mitochondria. This hypermetabolism allowed users to burn fat at an accelerated rate. However, DNP also led to serious side effects, including hyperthermia, cataracts, and death from overheating, leading to its subsequent banning by the FDA.
The 1950s and 1960s witnessed the rise of amphetamines for weight loss. Amphetamines work by increasing the release of norepinephrine and dopamine in the brain, which leads to reduced appetite and heightened alertness. However, chronic use can result in a range of adverse effects, including addiction, cardiovascular complications, and psychiatric symptoms such as paranoia and hallucinations. When these risks became clearer, amphetamines were reclassified as controlled substances.
Other popular products of the time were the ‘rainbow pills’, so named for their multi-coloured appearance. These combinations of drugs included amphetamines, thyroid hormones, diuretics, and barbiturates (to counteract the stimulating effects of the amphetamines). While weight loss was achieved, side effects including heart attacks and strokes were not uncommon.
The 1990s were taken by storm by fen-phen, a combination of fenfluramine and phentermine. Phentermine, a stimulant similar to amphetamines, suppressed appetite, while fenfluramine, a serotonin releaser, provided additional satiety. However, it was soon discovered that fenfluramine was associated with significant adverse cardiovascular effects, such as valvular heart disease and pulmonary hypertension. It was withdrawn from the market in 1997.
With the beginning of the 21st century, the focus shifted towards targeting specific biological pathways. Unlike previous drugs that worked on the central nervous system, orlistat, introduced in 1999, works locally in the gastrointestinal tract to inhibit pancreatic lipase, the enzyme responsible for breaking down fat. By preventing the absorption of dietary fat, orlistat reduces caloric intake, but the unabsorbed fat leads to gastrointestinal side effects, which, while not life-threatening, proved socially inconvenient, limiting its widespread adoption.
GLP-1 receptor agonists, introduced in the 2000s, revolutionised the treatment of obesity by offering a safer, more targeted approach. Liraglutide paved the way for semaglutide, which offers enhanced efficacy with fewer side effects. Unlike earlier treatments that relied on appetite suppression alone, semaglutide works by altering the underlying hormonal and metabolic pathways that contribute to obesity. Most recently, tirzepatide (marketed as Mounjaro), a dual GIP/GLP-1 receptor agonist, has emerged as a potential breakthrough in the field. Early clinical trials indicate that tirzepatide may produce even greater weight loss than semaglutide, with a more favourable side-effect profile.
The comprehensive metabolic effects of semaglutide have led researchers to consider GLP-1 receptor agonists as a potential new class of drugs for managing metabolic syndrome.
From purges to tapeworms: weight management through the ages
Although the obesity epidemic is a modern phenomenon, the pursuit of balanced diet, exercise and pharmacological solutions for weight loss has been a human preoccupation for centuries. Shen Nong, the Yellow Emperor of China’s Han dynasty (c. 2695 BC), is believed to have discovered green tea consumption to help in keeping a healthy weight. In India, around 600 BC, the physician Susruta recognised the problems of a sedentary lifestyle and prescribed exercise, fasting and diet to improve health. He was also the first to link diabetes with obesity. According to Herodotos, Ancient Egyptians used to purge for three days a month to cleanse their bodies from harmful food. In Greek and Roman times, a simple diet and exercise were recommended for health and fitness, but natural remedies for curbing appetite and induce purging were also used. Vinegar, saffron, almonds, violets were among them. In the Middle Ages, many slimming tonics contained dangerous metals, such as mercury and arsenic, which induce gastrointestinal distress and curb appetite through poisoning. In the Victorian era, among the more infamous treatments for weight loss was the tapeworm diet, where capsules containing tapeworm eggs were ingested, in the hope that the tapeworm would burn some of the calories. Medical literature of the time contains many case studies of patients suffering from complications related to this practice.
What semaglutide’s cardiovascular benefits could do for cancer
Semaglutide has demonstrated significant cardiovascular benefits, particularly for patients with type 2 diabetes at elevated risk of heart disease. The SUSTAIN-6 trial provided compelling evidence of semaglutide’s cardioprotective effects, showing a 26% reduction in major adverse cardiovascular events over two years compared to placebo.
The cardiovascular benefits of semaglutide stem from its effects on inflammation, glucose metabolism, and weight management. By reducing chronic inflammation, a key driver of atherosclerosis, semaglutide helps protect against vascular damage. Its ability to improve glycaemic control further reduces the risk of hyperglycaemia-related blood vessel damage, providing additional cardiovascular protection. It reduces LDL cholesterol and triglycerides, which improves lipid profiles and blood pressure, contributing to its overall cardioprotective effects. In patients with resistant hypertension, semaglutide has demonstrated the ability to lower blood pressure levels, probably due to its effects on weight and glucose metabolism. This is particularly significant given the strong association between hypertension, obesity, and diabetes.
These benefits to cardiac health could have a knock-on effect for cancer in two ways. Firstly, in the event that semaglutide – or other GLP1 receptor agonists – get approval for use managing certain cardiology conditions, that could also offer a protective effect against many cancers by lowering the inflammatory and metabolic risk posed by obesity – should such a protective effect be conclusively demonstrated, and with the caveats about a possible raised risk for e.g. medullary thyroid and pancreatic cancer.
Secondly, should this class of drug find a use in the management of cancer, in contrast to the many cancer drugs that pose potential harm to heart health, this treatment could benefit heart health, making its use much safer in patients with cardiac comorbidities.
Creating a stir among cardiologists
Excitement about what semaglutide could do for cardiology patients was evident at the 2024 Congress of the European Society of Cardiology, held in London at the end of August. While molecular biology tends to take a back seat in cardiology conferences, this metabolic drug was the subject of five separate sessions. Evidence was presented of benefits: for heart failure patients; for managing heart failure outcomes among individuals with type 2 diabetes and chronic kidney disease; for the contribution of its anti-inflammatory properties to reducing cardiovascular events; and for the reduction of adverse cardiovascular outcomes in women with obesity. Across these presentations, semaglutide was consistently recognised for its potential to improve both metabolic and cardiovascular outcomes in high-risk patient populations.
What semaglutide’s effect on neurons could do for cancer
GLP-1 receptors are not just distributed throughout the gastrointestinal tract, but also in several other organs and tissues in the body, including key areas of the brain. These include the hypothalamus, the brainstem, and the regions involved in the brain’s reward system, such as the ventral tegmental area and nucleus accumbens, as well as in the hippocampus and olfactory bulb. When GLP-1 receptors are activated in the hypothalamus and brainstem, they can impact on obesity by stimulating neurons that promote feelings of fullness (POMC and CART neurons) and inhibiting those that trigger hunger (NPY and AgRP neurons).
But semaglutide also seems to help normalise dysregulated neural circuits that contribute to addictive and compulsive behaviours, and this in turn could reduce significant risk factors for cancer and many other conditions. Patients have reported decreased interest in activities like smoking, drinking, excessive shopping, nail biting, and skin picking after starting semaglutide treatment. Real-world data analyses have demonstrated that semaglutide treatment is associated with a significant reduction in both the onset and recurrence of cannabis use disorder when compared to alternative medications. It also shows promise to mitigate cocaine addiction.
In animal studies, semaglutide dose-dependently reduced binge-like and dependence-induced alcohol drinking in mice and rats, while also modulating GABA neurotransmission in brain regions associated with addiction. Ongoing studies, such as the STAR (Semaglutide Therapy for Alcohol Reduction) trial, aim to provide more definitive evidence on semaglutide’s efficacy and safety in treating alcohol use disorder.
It all sounds a bit too good to be true, and the evidence for benefit beyond its currently approved indications for type 2 diabetes and obesity is still quite preliminary. That said, oncology has long been searching for a drug that could address the metabolic and inflammatory risk factors known to be important in many cancers. When a candidate looking this good comes along, which might also help improve heart health and at the same time treat the addictive behaviours that raise cancer risk, it surely deserves our full attention.
With the collaboration of Francesca Albini
See also
Drug repurposing: EU legislative changes could speed up new treatment options
Body weight influences breast cancer risk in women with BRCA1 and 2 mutations
Obesity and cancer: 12 things clinicians and patients should know
Cancer could overtake cardiovascular disease as leading cause of death in type 2 diabetes