Many women who undergo breast reconstruction after mastectomy end up disappointed. It is estimated that as many as 30% of women have to live with aesthetic results they are not happy with. On the other hand, some of those who opt against reconstruction may have chosen otherwise had they had a good idea in advance about how it would turn out.
Maria João Cardoso is head breast surgeon at the Champalimaud Cancer Centre in Lisbon. She founded the patient support centre Mama Help and co-leads a research group on improving outcomes in breast surgery at the Institute for Systems and Computer Engineering, Technology and Science in Porto. Using their combined expertise in breast surgery and computing, the group are addressing a new challenge. They are trying to find a way to help patients with breast cancer to foresee the realistic results of breast surgery – any procedure, from conservative to radical, with and without reconstruction – before going ahead with the operation.
“Breast cancer overall survival has increased impressively in the last 20 years. Although improved survival is crucial, quality of life should parallel this endpoint,” says Cardoso.
Quality of life is heavily dependent on the side effects of treatment. In breast cancer, besides the side effects of systemic treatments, there is also the visible and lasting impact of surgery and radiotherapy. “Breast-conserving treatment or mastectomy with immediate breast reconstruction are the most common surgical options. Moreover, with more sophisticated treatments, better aesthetic outcomes are anticipated. Some of the possible causes of patients’ disappointment could be prevented if the outcomes could be measured consistently and possible causes of poor satisfaction identified,” says Cardoso. She wants to develop an evidence-based tool to visualise the range of aesthetic results that are likely following breast reconstruction, in order to allow the women to predict how they could feel with their new body image.
What surveys can and cannot tell us
Recent studies done in North America show that women who opt for breast reconstruction after a mastectomy have a high rate of complications: one in three develops a postoperative complication over the following two years, and one in five requires more surgery; in 5% of cases, reconstruction fails (JAMA Surg 2018, 153: 901–8; ibid pp 891–9). The published findings also showed that women who undergo autologous breast reconstruction are generally more happy with the results in the long term than women who choose reconstruction with breast implants. In order to evaluate satisfaction, the researchers surveyed women on their quality of life 90 days before their mastectomy, and at 1, 2, 3 and 4 years after reconstruction. They asked the women about their perception of their breasts, and their emotional, social, sexual and physical wellbeing. Specific questions addressed how their breasts appeared, how satisfied they were with that appearance, how bras fit, and how their breasts felt to the touch. Emotional and social wellbeing were investigated, asking questions about their body image, their confidence in social settings and their sexual wellbeing. Questions about physical wellbeing, pain and physical difficulty while performing daily activities were also included in the survey.
The surveys revealed that satisfaction is not always related to an objective failure. In a study published two years earlier, Cecilia Dahlbäck from the Department of Plastic and Reconstructive Surgery at Skåne University Hospital in Malmö, Sweden, tried to identify risk factors for poor satisfaction with conventional breast-conserving surgery (World J Surg Oncol 2016, 14:303). “The majority of the women, 84%, were satisfied with the overall aesthetic result. But if we look in detail at the results, we see that the rate of satisfaction regarding symmetry between the breasts was 68% and for skin sensitivity in the operated breast it was 67%,” says Dahlbäck.
Factors contributing to a poor subjective level of satisfaction with overall aesthetic outcome included excision of more than 20% of the preoperative breast volume and axillary clearance. A high BMI (≥30 kg/m2) was associated with complaints related to symmetry. Re-excision and postoperative infection were associated with lower rates of satisfaction regarding both overall aesthetic outcome and symmetry.
According to the researchers, the choice of the surgical technique should take into account both objective data and the patient’s preferences.
The questionnaires used to measure satisfaction in many of these studies were developed in plastic surgery and not specifically for cancer patients (Plast Reconstr Surg 2009, 124:345–53). “The most common evaluation methods on the impact of treatments are patient reported outcomes,” says Cardoso. “They consist almost exclusively of questionnaires, usually with low reproducibility due to the subjectivity inherent to patient’s self-evaluation. That’s why we are trying to find a more objective way to determine the risk factors of poor patient satisfaction in breast reconstruction after cancer therapies.”
A gold standard for evaluating outcomes
It is often very difficult for professionals to fully understand and explain why an excellent result, based on the technical analysis of the starting situation, might still be far from ideal, and more or less satisfactory in the patient’s eyes. This is because there is no standard model for comparison, and other personal factors, such as age, marital and socioeconomic status, and psychological factors, can contribute to the final appreciation.
Reconstruction techniques included in the study
The CINDERELLA project is developing a tool to help candidates for the following common breast surgery procedures predict how they will look and feel about their body:
– Conservative surgery – unilateral
– Conservative surgery with bilateral reduction
– Conservative surgery with LD or LICAP/TDAP flaps
– Mastectomy with unilateral reconstruction with implant
– Mastectomy with unilateral reconstruction with autologous flap
– Mastectomy with bilateral reconstruction with implants
– Mastectomy with bilateral reconstruction with autologous flaps
– Mastectomy with unilateral reconstruction with implant and contralateral symmetrisation with implant (augmentation).
– Mastectomy with unilateral reconstruction with autologous flap and contralateral symmetrisation with reduction
– Mastectomy with unilateral reconstruction with autologous flap and contralateral symmetrisation with implant (augmentation)
– LD – latissimus dorsi, LICAP – lateral intercostal artery perforator, TDAP – thoracodorsal artery perforator
Objective methods, using artificial intelligence (AI), have been tried to circumvent the lack of reproducibility of patient reported outcomes. However, there is a poor agreement between questionnaires and AI.
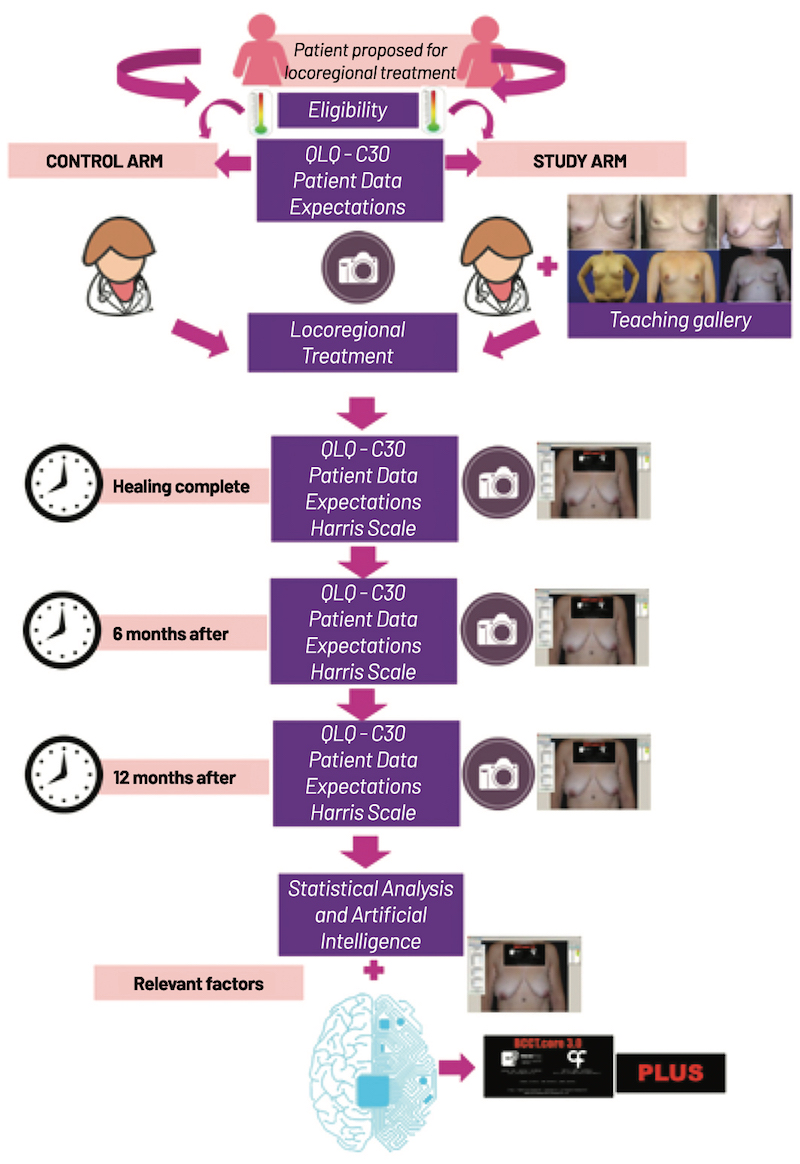
The project Cardoso and colleagues are working on aims to create a gold standard method for the aesthetic evaluation by giving patients a better insight into the outcomes, allowing them to judge more objectively, also using inputs from both objective and subjective factors. Named CINDERELLA (Comparing patient’s decision on aesthetic outcome with the BCCT.core objective evaluation after controlled teaching in patients proposed for breast cancer locoregional treatment), the hope is that the project will “lead to a better choice of locoregional treatments and better quality of life,” says Cardoso.
The CINDERELLA project
Apart from self-reporting, surgical outcomes can be evaluated by an expert assessment. This is ideally done by someone who is not involved in the treatment, to avoid bias, and the evaluation should be preferably be done by more than one person. This type of expert assessment is often done using digital photographs, but it is very costly and time-consuming. If you have a large number of patients, it’s very difficult to ask the experts to look at all the pictures. Then there is the so-called objective assessment, which is usually done through measurements looking at the patient’s images on a screen. “We measure the distance between the nipples, the distance to the arm and the edge, we compare symmetry, etc.” explains Cardoso. “Our research team already developed a software called BCCT [Breast Cancer Conservation Treatment], used by almost 300 centres all over the world, that does it automatically using the pre- and post-surgical photos of thousands of patients, which will allow the analysis and comparison of a large number of pictures in many different centres and countries.”
Within the CINDERELLA study, she explains, candidates for breast surgery who are included in the intervention arm will receive educational training with an expert using a teaching software, while the control group will receive the general information currently provided to all their patients. “We will also be able to evaluate the importance of cultural environment on patients’ satisfaction, as we already know that Eastern and Western countries have a different cultural approach toward body image, but we will also be able to identify objective risk factors for dissatisfaction, including the surgeon performance.”
Beyond photoshop
Digital photo retouching techniques have been used in plastic surgery for many years to anticipate aesthetic results, but Cardoso’s project aims to go well beyond that.
The realistic outcomes that the surgeons can automatically simulate today are based on the photos of the patient and on the expected changes that the surgical technique will introduce. AI allows the system to become smarter and more efficient, by adding more cases and more photos. Any possible confounding or influential factor will be recorded, including age, body mass index, bra size and cup, education degree, profession and hobbies. Marital status, pregnancies and offspring, together with breastfeeding habits and menopausal status, can also influence the results of reconstructive surgery, so they will be included in the analysis. The database will consider also possible complication such as smoking, diabetes and radiotherapy (total dosing and fraction number).
Taking personalised surgery one step further
The trial has been approved in Portugal and has already completed the feasibility phase. A first group of 340 patients and 340 controls will be recruited in the next phase. An expert evaluation of each outcome will be compared with the results from the AI analysis to focus on the determinants of poor outcomes or poor satisfaction, including the kind of training the patient received before the surgery and how it shaped her expectations.
“We hope to modify and upgrade our software to include the patients’ perspective as it comes out from the statistical analysis of the questionnaires and surveys. It will be called ‘BCCT Plus’, and will be available open access to all the surgical centres dealing with breast cancer surgery,” says Cardoso. “We don’t have sponsors and support from companies, as it is an open-access project, even if we have a large number of pictures in our database and enough nurses volunteering to be trained to be educators and to use our teaching tool. But we already have our proof of concept: machine learning can help us get the best possible result out of each surgical procedure – fostering the idea of personalised surgery – and develop a tool that people will be able to use all over the world, in a multidisciplinary team including oncologists, nurses and surgeons and patients, each of them with their own expectations.”