Image: Delivering palliative care in Kerala, India ©Camilla Perkins, camillaperkins.com
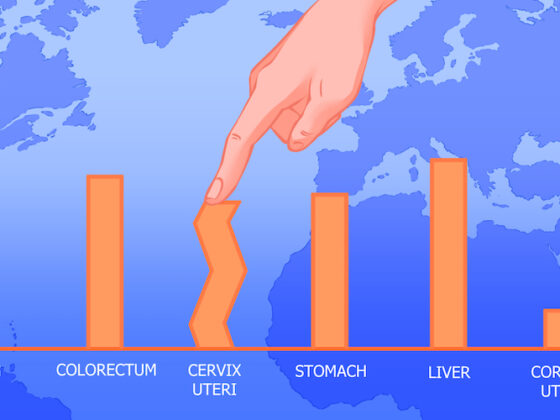
Delivering palliative care to avoid unnecessary health-related suffering is defined by the World Health Organization (WHO) as “a moral imperative and a human right”. Yet only a tiny proportion of the estimated 57 million people who need palliative care each year are able to get the care they need.
To assist countries in their efforts to introduce effective palliative care services, the WHO recently published new guidance. New WHO technical tools and a forthcoming ‘compendium’ of resources will address widely varying international needs and circumstances, assisting resource-poor countries to integrate palliative care into universal health coverage.
Palliative care: what it does, who it’s for
The World Health Organization defines palliative care as: “…an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness or serious health-related suffering. It includes, but is not limited to, end-of-life care. It is not the “last resort”, but should be integrated early in the care of people affected by a life-threatening condition.” For people with advanced cancer, delivering palliative care can help them live more comfortably, and in some cases can help extend their lives.
Recognising that different models are needed for different countries, the WHO is effectively offering a menu of indicators to monitor success in palliative care provision, leaving countries free to adopt what is most suitable for their particular setting. The hope is that governments will be more likely to invest in palliative care because it is more practicable.
“We need to ensure universal access to palliative care, but this is far from the reality,” said Marie-Charlotte Bouësseau, Ethics and Health team leader at WHO headquarters in Geneva. “We know that the great majority of populations around the globe do not have access to palliative care.” Worldwide only about 12 per cent of palliative care need is currently being met.
Emmanuel Luyirika, Executive Director of the African Palliative Care Association, said the new tools could be used to call on African governments to act. “The documents clearly define the actions that governments can use to improve and measure access and delivery of palliative care…Governments do not have to re-invent the wheel. They can adapt and adopt them for better service delivery.”
“Once you are able to measure, you can hold people accountable and improve on service delivery,” said Luyirika. “But the actions also require governments to invest in their health systems.”
World Health Assembly resolutions recognise palliative care as an ethical responsibility of health systems and call for WHO Member States to assure its delivery through comprehensive primary health care services. This mandate is related to the commitment to universal health coverage.
“Governments do not have to re-invent the wheel. They can adapt and adopt them for better service delivery”
The documents released by WHO include a set of actionable indicators that can be used by countries to monitor and assess the development of palliative care and resources on practical approaches to supporting policy, strategy and practice. Countries can select from a set of indicators for monitoring national strategies, policies and plans. These can be incorporated into planning and delivery at the national, district and point-of-care levels.
The WHO documents stress that providing good palliative care is an ethical responsibility for the whole community – not only for health professionals but also the social workers, family caregivers and community caregivers.
“There is very little value in creating access to services that are ineffective, unsafe, are inefficient and not timely enough to provide the care that people need,” said Anna Ray a palliative care expert from the WHO Integrated Health Services Department.
“The model would not be ‘copy and paste’ because building palliative care is like building a house: we should not build the house the same way in Uganda, Japan or Costa Rica. So I think this adaptation is crucial at local level, to maximize the impact and the quality of what we do,” said Ray.
She said that the indicators were the product of a consensus building exercise involving experts from around the world. But their benefits needed to be verified in the real world.
“The important issue here is quality. It takes concerted effort across the health system from all of our different perspectives”
Uganda is one of the countries that has been selected to use these new indicators to see how they work in practice. Mark Mwesigwa, the country director of the Palliative Care Association of Uganda (PCAU), said: “When you look at the new model, it empowers people in the community who know that the service is available and they can seek the services. The issue for us now is how best we can actually develop our own indicators based on the framework that has been laid down.”
“I think the important issue here is quality. It doesn’t happen by accident. It takes concerted effort across the health system from all of our different perspectives,” he said.
Different models for different countries
Image: Roadside palliative care administration, Uganda: Nurse Harriet Birungi meets with a patient.
Credit: Palliative Care Association of Uganda ©PCAU
While not laying down blueprints for the development of palliative care services, the World Health Organization guidance does mention specific examples of good practice.
Panama gets a mention (page 19) as an example of success in developing “a system of sustainable palliative care delivery that is integrated into primary care, deliberately making use of existing health system structures and integration with the country’s broader offer of UHC [universal health coverage] free of charge”.
Uganda is highlighted (page 27) as an example of increasing accessibility to opioid pain relief alongside strengthening education and under a supportive national policy for palliative care. “With inclusion of palliative care in all medical curricula since 1994, Uganda has a medical workforce that is well informed about palliative care, with opportunities for specialisation.” Also mentioned is the priority palliative care and quality of care get within Uganda’s national health plan in the context of its ambitions for universal health coverage.
South Africa’s use of Palliative Care Standards to accredit hospice and community-based palliative care services, and its mentorship scheme are highlighted (page 34). “The district mentorship programme facilitates the fast tracking of compliance with palliative care standards and provides a mechanism to cascade good practice in quality care between hospices and partner organizations.”
India is offered as a good example of using remote learning with mentorship from international experts (page 44), which is seen as a model that could be adapted for other countries to “catalyse the development of initial quality improvement capabilities in palliative care”. The Indian programme promoted quality improvement education and collaborative learning among a number of palliative care centres in the country. “Each palliative care centre was matched with an international partner that provided coaching, education and mentorship in quality improvement methods, meeting regularly virtually for teaching, exchange and problem solving.”
The new WHO Guidance
In its guidance document, Quality health services and palliative care: practical approaches and resources to support policy, strategy and practice, the World Health Organization (WHO) summarises key actions that can be taken at a national, district and point of care level, that can be applied to variety of different palliative care models. These include principles, of policy making, planning, implementation and building in quality control and monitoring systems.
In its document on Assessing the development of palliative care worldwide: a set of actionable indicators, the WHO offers guidance on selecting and implementing palliative care indicators, that can be tailored to the palliative care model and wider health system of each country. This includes addressing questions such as: Are they effective as indicators of how well key aspects of the palliative care system are working ? Is collecting/generating the data feasible? Are the data a good fit within the country’s wider health information system? How will the data be used? Do all parties involved understand their roles in implementing the monitoring?