A combination of existing drugs may inhibit development of bone metastasis in breast cancer patients. The study published in Cancer Discovery, 1 March, found that a combined treatment strategy that activates T cells while at the same time targeting cells inhibiting T cells could prevent metastases from breast cancer forming in the bones.
“Our study maps the dynamic changes in the bone microenvironment during BC [breast cancer] bone metastasis and uncovers a key crosstalk …that facilitates the formation of an immunosuppressive and growth-permissive metastatic niche,” write the authors. The advantage of the strategy is that the drugs targeting T cells are either already marketed for other indications or in clinical trials. “Consequently, the process of obtaining permits to use them against bone metastasis in humans could potentially be relatively short,” says Neta Erez, the corresponding author, from Tel Aviv University.
Mortality from breast cancer is largely due to metastatic relapse in distant organs, with bone metastasis occurring in up to 70% of patients with advanced disease. Bone metastases are mostly osteolytic (bone destructive), with severe morbidities including pathological fractures, hypercalcaemia and spinal cord compression. Since there are currently no efficient treatments to prevent or inhibit bone metastasis, better understanding of the underlying mechanisms is essential to enable development of novel therapeutic strategies. It has increasingly been recognised that the metastatic microenvironment plays a crucial role in supporting metastasis formation. However, studying the microenvironment has proved challenging, due to a lack of animal models that are able to model the different stages of bone metastasis.
In an earlier study, published in 2020 in Scientific Reports, Erez and colleagues developed 4T-Bone, a mouse model of spontaneous breast cancer bone metastasis. “Because metastasis is a multi-stage process, it’s very important to study metastasis in a physiologically relevant setting, where there is a primary tumour metastasising to different organs,” Erez tells Cancerworld. “We recognised that the earlier approach of injecting tumour cells directly into blood or bone skipped the different stages of metastasis. We wanted to develop a mouse model recapitulating the physiological process of the disease.”
For the 4T-Bone model, the investigators injected a breast cancer cell line into mice, then isolated cells from the rare spontaneous bone metastases that developed in a few mice. The metastatic cells were then reinjected into the breast tissue of other mice. “By doing two rounds of selection we obtained more aggressive cells that homed faster to the bone,” explains Erez.
For the current study, the team set out to use their model as a platform to study both early- and late-stage bone metastasis. “Patients are like a black box; we only know they have bone metastasis when it’s well established. By using our mouse model, we could open up the black box and characterise changes to the microenvironment that occurred in the early stages,” says Erez.
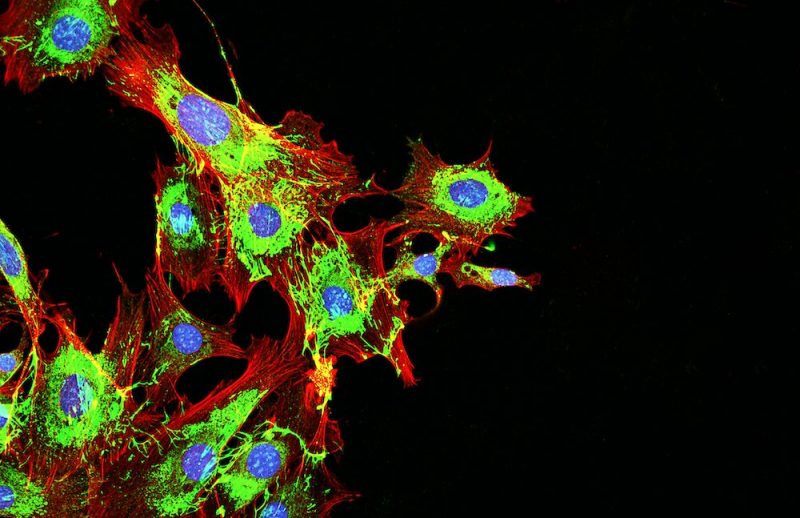
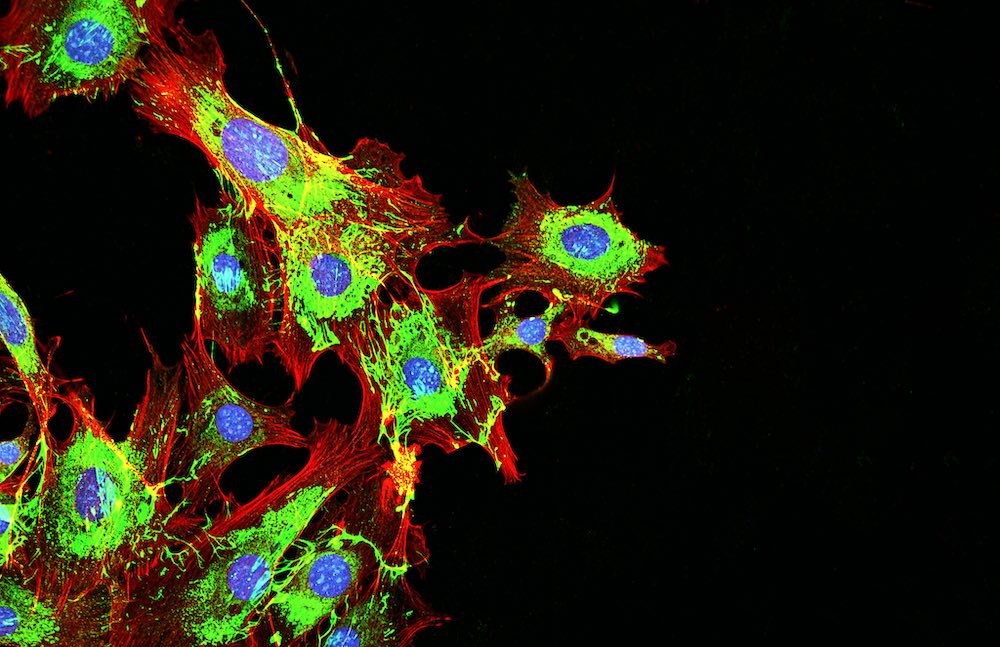
First, the team profiled changes in the transcriptome (RNA gene readouts) for mice with normal bone, early-stage metastasis, and late-stage metastasis, respectively. After identifying a large number of changes in metastatic mice they went on to use multiple algorithms (including GSEA, KEGG, and TRRUST algorithms) to identify the most significant changes. Ultimately, the process led them to focus on interactions between granulocytes and T cells in the bone metastatic microenvironment, and in particular on the TIGIT checkpoint receptor located on the T cells and the pro-inflammatory cytokine IL1Beta secreted by granulocytes, which were both raised in metastatic models.
“In principle, the role of T cells is to kill cancer cells. We found that, in metastatic mice, the T–cells were not working well, and that granulocytes secreted something suppressing T cells,” explains Erez. “Our findings raised the possibility to use two different drugs in combination to both activate the T cells and inhibit the granulocyte cells.”
Next, the team went on to target the TIGIT checkpoint receptor and IL1Beta, with antibodies in mouse models of breast metastasis, and found that, in comparison to controls (who did not receive treatment, or received only one of the antibodies), metastases were significantly reduced, and that the mice lived significantly longer.
Finally, the investigators analysed publicly available datasets and tissue samples of bone metastases from patients with breast cancer, prostate cancer, colorectal cancer, lung squamous cell carcinoma, kidney cancer, and cancer of unknown origin. In all the different tumours they showed that TIGIT was highly expressed. “This suggests that our therapy approach, which we showed worked in mice, might also be useful in human patients with a range of cancers,” says Erez.
“Taken together, these results suggest that combining IL1Beta and TIGIT neutralisation is an effective treatment strategy to attenuate BC [breast cancer] bone metastasis by sustaining and promoting anti-tumour immunity,” write the authors.
Clinical trials, stresses Erez, will be needed to verify the effectiveness of the new therapeutic strategy. Such trials may be facilitated by the fact that human drugs targeting TIGIT and IL1Beta are already available. Specifically, a human anti-TIGIT monoclonal antibody, tiragolumab, is currently being trialled as a first-line treatment in advanced hepatocellular carcinoma; while the IL1Beta receptor antagonist, anakinra, is already licensed to treat rheumatoid arthritis.
In the meantime, the team are extending their approach to develop a range of mouse models to explore pathways involved in brain and lung metastases in breast cancer, and peritoneal metastases in ovarian cancer.