This article is from 2021, if you are interested in prostate cancer you can also read:
- Reversing the rising trend in prostate cancer mortality in Poland
- Increasing cardiorespiratory fitness reduces risk of prostate cancer
- New prostate cancer blood test combining PSA with epigenetic test could reduce biopsies
- Localised prostate cancer: active monitoring offers valid option
- Plant-based diets cut risk of prostate cancer progression and recurrence by over 50%
Five years ago, the idea of national screening programmes for prostate cancer had gone cold. The benefits of PSA (prostate specific antigen) blood testing, introduced as a screening tool in the 1980s, had long been fiercely debated. But by 2015 the United States Preventive Services Task Force had recommended against PSA-based screening, and research had indicated that the potential benefits of reducing mortality probably didn’t outweigh the risks of overdiagnosis, overtreatment – and a resultant damage to men’s quality of life.
Even Europe’s urologists weren’t recommending systematic screening. “Screening for prostate cancer is one of the most controversial topics in the urological literature,” said the European Association of Urology (EAU) in its 2015 guidelines. “The impact on the patient’s overall quality of life is still unclear. It appears to be minimal in some subgroup analyses, but significant in others. This has led to strong advice against population-based systematic screening in all countries, including Europe.”
How times change. In the past two years, the EAU has been trying to convince Europe’s politicians that PSA-based early detection programmes should be implemented at a population level across Europe. The language surrounding PSA-based screening is still heated, but now it is the heat of the campaign.
“There are now game changers that cancel out all the anti-PSA propaganda that we’ve heard over recent years,” says Hein Van Poppel, Adjunct Secretary of the EAU. “It is now possible to overcome all the disadvantages that the use of PSA has brought in the past.”
In March, as a result of campaigning by a coalition led by EAU and the prostate cancer patient organisation Europa Uomo, the European Commission’s ‘Beating Cancer Plan’ included a promise to update the European Council’s recommendation on cancer screening – including the possible addition of prostate cancer – by 2022. The following month, Hein Van Poppel gave evidence to an EU Beating Cancer consultative session on early detection.
Three game changers
His message about why the game had changed was clear. First, prostate cancer deaths are rising in Europe and something needs to be done urgently to turn this around: 107,000 men died from prostate cancer in the European Union in 2018 compared to 92,000 in 2010.
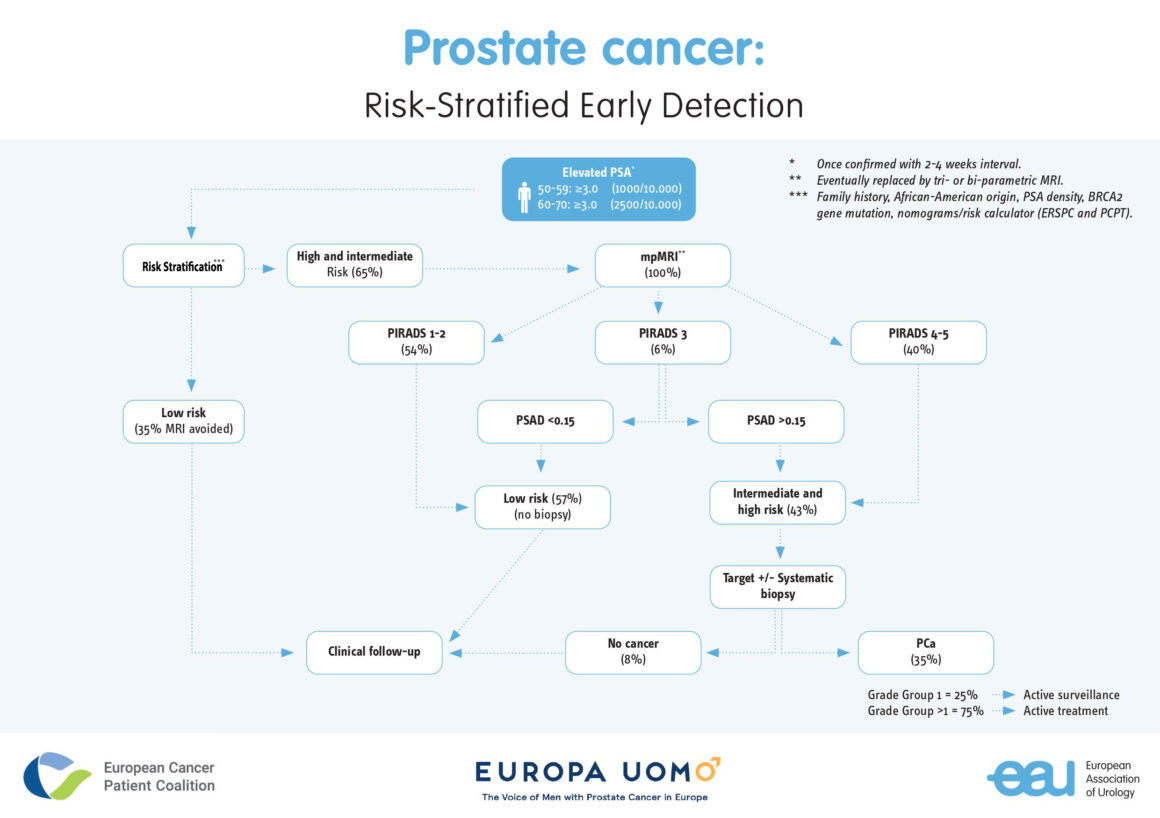
Second, objections to PSA screening are outdated, because they are based on research that pre-dates the introduction of MRI prostate scanning as a follow-up to raised PSA levels. This reduces the need for potentially harmful biopsies and ensures that the biopsies that do take place are more effective at identifying dangerous cancers, because guided by MRI scans.
And third, the use of new risk stratification algorithms can ensure that only men most at risk of severe disease are targeted, reducing the number who will be investigated or treated for prostate cancer when the risk to life is small.
“The biggest argument against blanket PSA testing for men is the risk of overdiagnosis and overtreatment,” says Van Poppel. “The arrival of multiparametric MRI [mpMRI] is the most important counter to this argument. It means we can ignore insignificant cancers and detect more significant cancers before embarking on biopsy, which can cause complications, and treatment, which can have damaging side effects on men’s quality of life such as urinary incontinence and erectile impotence.”
There’s no doubt that the publication of major trials (PROMIS and PRECISION) in 2017–2019 demonstrating the effectiveness of mpMRI at diagnosing prostate cancer was a turning point (see timeline below). This prompted the EAU to change its guidelines on prostate cancer diagnosis in early 2019, recommending mpMRI after a raised PSA reading, thus opening the way for a review of screening.
Not just about survival
The new knowledge base has brought renewed support for PSA-based screening programmes from beyond urology – most significantly from patient organisations. Europa Uomo formally decided to back the case for a Europe-wide PSA-based screening programme for prostate cancer shortly after the EAU changed its guidelines. But it has also decided to avoid the word “screening” in its campaigning: it is too strongly associated with population-wide testing, as opposed to testing of specific, well-informed groups – which is what they are calling for.
For Europa Uomo, which represents prostate patient groups in 27 countries, the case for early detection programmes is intricately linked with the need to improve quality of life of men with prostate cancer throughout Europe – not simply reducing mortality.
“It’s very clear from the data that the more advanced the prostate cancer at diagnosis, the worse the effects of treatment on quality of life,” says Europa Uomo Chairman André Deschamps.
“We must realise that more than 50% of prostate cancer patients in Europe are diagnosed in a metastatic phase, at which stage treatment is expensive, limited in effectiveness and brings very unpleasant side effects,” said Deschamps. “This is due to the lack of early detection programmes.
“We have the scientific knowledge today to prevent prostate cancer deaths and give patients a much better quality of life. It is the duty of policy makers to make that happen.”
Van Poppel recognises that having patients as allies is vital in convincing European politicians that the case for prostate cancer screening programmes must be reconsidered. “We urologists do not have a good voice to claim that we should do more early detection,” he says. “People think we want it because we have a vested interest in more men being diagnosed. The fact that patients want it as well is very important.”
“Compared to the classic diagnostic strategy we can use PSA more cleverly, apply MRI and further risk stratification tools”
Together with Europa Uomo and the European Cancer Patient Coalition, EAU has submitted white papers and scientific evidence, and spoken to many MEPs about the need for early detection. The message has been crafted to reflect changing times. “Compared to the classic diagnostic strategy (that is, PSA and direct biopsies), we can use PSA more cleverly, apply MRI and further risk stratification tools in men at increased risk,” says a factsheet for MEPs. “This combined approach in well-informed men will allow a substantial reduction of the number of men that need to undergo biopsy (up to 70%) and over-diagnosis up to 20%.”
The campaigning has borne its first fruit with the Beating Cancer Plan announcement opening up the possibility of adding prostate cancer to the current European Guidelines on population screening programmes. But now comes the hard part. The European Commission cannot implement screening across Europe, even if it wanted to. It can only encourage member states to take action. And should the same actions be recommended across all member states? What can realistically be achieved?
A blueprint
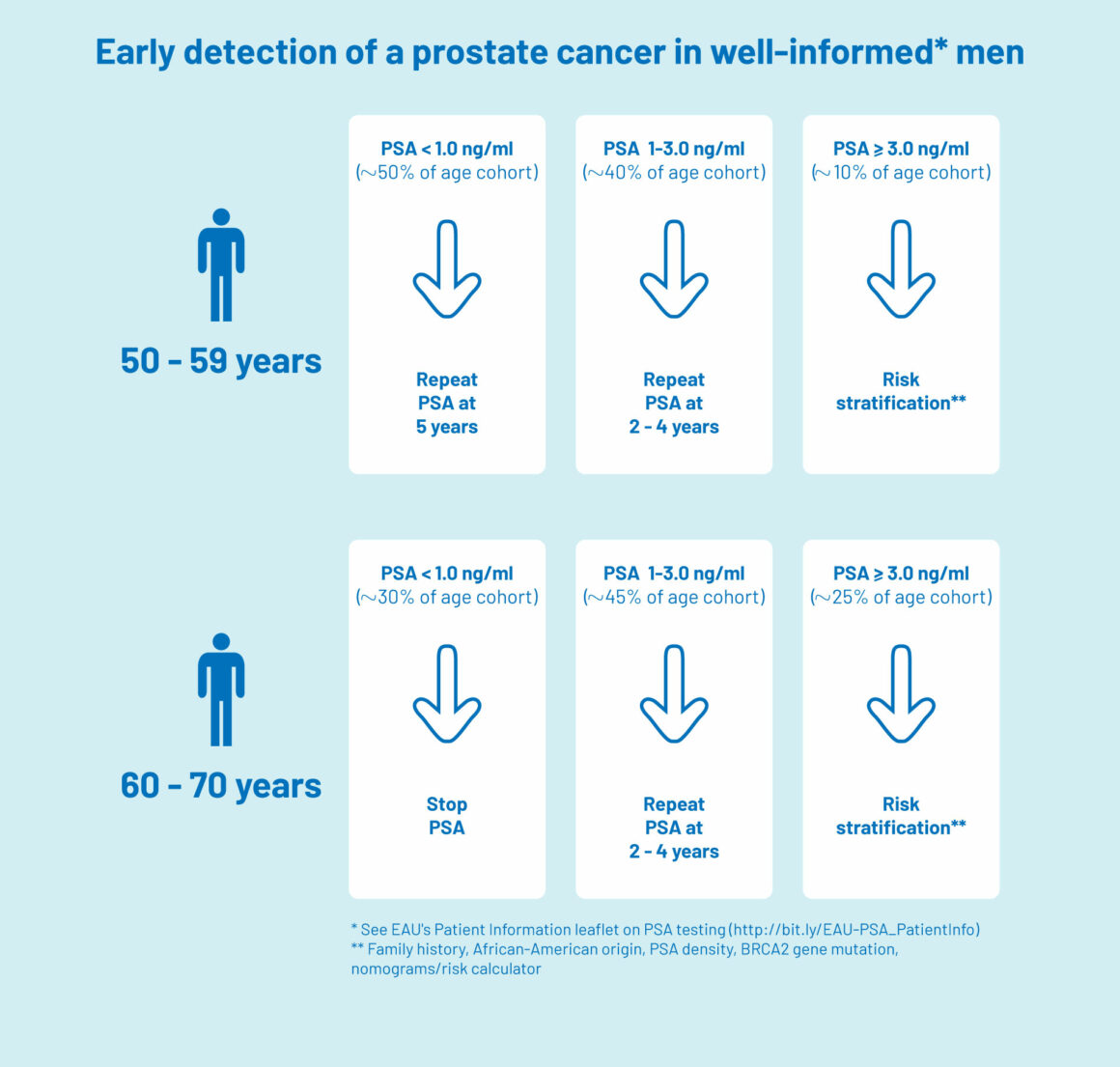
A blueprint for EU action was set out in a paper published in European Urology written by Van Poppel and other urologists and academics, including Monique Roobol who is Professor in Decision Making in Urology at Erasmus University Medical Centre, Rotterdam. It sets out a recommended early detection process (or ‘algorithm’), starting with PSA testing among groups at higher risk, with further actions to follow a raised PSA reading, again varying according to age group and risk factors. A key recommendation is for men to receive counselling on the potential harms and benefits of early detection, before undergoing testing.
Blueprint for PSA-based screening programmes in Europe (simplified version)
The top figure was adapted from European Cancer Patient Coalition, Europa Uomo, European Association of Urology (2021) Early detection of Prostate Cancer: Facts and scientific update for the EU Cancer Plan published on the ECPC website, downloaded 21 April 2021.
The bottom figure was downloaded from the EAU website on 21 April 2021
But a problem has immediately become apparent to European politicians who, having accepted the need for screening in principle, are now faced with cold practicalities. Variations in technologies and skills across European countries are so great that a one-size-fits-all recommendation on screening will simply be impossible. For example, mpMRI scans – already part of the prostate cancer diagnostic process in many northern European countries such as England and Norway – are currently beyond the reach of many countries in central and eastern Europe.
Hein Van Poppel says that these issues were discussed in recent conversations with Stella Kyriakides, European Commissioner for Health and Food Safety since 2019.
“I think she understands the challenges very well. But we are not asking for all men to be given an mpMRI. Yes, we want risk-stratified PSA-based early detection programmes in every country. But, before that we need awareness campaigns among the population and education of GPs, so that everyone understands the risks and benefits of screening based on recent evidence.”
“Dependent on resources, all countries should introduce some sort of stratified screening”
Then, dependent on resources, all countries should introduce some sort of stratified screening. Roobol, who has also joined discussions with European Commission representatives to put the case for screening, says: “We should try to get some kind of programme everywhere. Let’s say that, if you have MRI available you can go for the platinum level algorithm. If you do not have that, you go for the gold algorithm, using other risk indicators such as PSA density. Anything that stratifies risk is better than leaving PSA testing as opportunistic.”
Winning over the sceptics
The new emphasis on using PSA testing in a strategic way, following up only those most at risk, is bringing many who had previously been worried about national screening programmes – oncologists and radiotherapists as well as urologists – over to the cause.
Two years ago, for example, Riccardo Valdagni, Director of the Prostate Cancer Programme at Fondazione IRCC at the National Cancer Institute in Milan, Italy, told Cancer World of his worries about diagnostic processes that effectively made biopsy a last resort. He said that men with a higher risk of prostate cancer (for example because of family history or a PSA level above a certain threshold) should have a biopsy even after a negative mpMRI scan, to minimise the possibility of false negatives.
The risk stratification algorithms being proposed put some of those worries to bed. “I agree with the concepts,” he says. “I think it’s an excellent way to arrive at individualised, risk-stratified prostate cancer screening, combining improved biological and clinical knowledge, and better use of new technology such as mpMRI – not in opposition to biopsy but to improve decision-making on performing biopsies.”
However, there still is resistance to structured PSA screening, mainly from general practitioners. According to Van Poppel, this is a considerable barrier – and is frustrating because, he says, it is often the result of simply clinging on to old beliefs. “They are not well informed,” he says.
Roobol agrees that GPs are fundamental to current problems with early detection. She believes that any official algorithm to guide testing – even if it cannot embrace mpMRI – is better than the current situation, where the influence of personal opinion is often making PSA testing erratic, opportunistic, and likely to lead to both overdiagnosis and under-diagnosis.
“It is known that men are being screened who are too old, or too young, or that screening is done every year or even every six months,” says Roobol. “A GP in one village may never screen anyone, but a GP in the village next door screens every man aged 40 and over.”
“Some still think that screening is not being done at the moment. It is being done and overall it’s doing more harm than good”
GPs aren’t the only barrier. Some key policy makers and influencers still need to be won over. “We have to try and convince people in Brussels and the World Health Organization that what is currently going on is not good. And, you know, they’re currently not convinced. For example, some still think that screening is not being done at the moment. That’s wrong. It is being done and overall it’s doing more harm than good.”
There’s no easy way of changing minds – partly because there’s no definitive piece of research showing that the pro-screening lobby is right. The only completed and authoritative research that exists is all based on wide, non-risk stratified, testing of men who were given biopsies after PSA. And they indicate, not surprisingly, that overtreatment is a significant risk.
This is a problem, acknowledges Roobol. There has simply been not enough time to conduct similar long-term studies looking at the effects of risk-stratified screening. She herself was one of the leaders of the European Randomized Study of Screening for Prostate Cancer (ERSPC), which reported in 2014 that overdiagnosis occurred in at least 40% of the screen-detected cases, indicating a high risk of overtreatment with unavoidable adverse effects. This has provided ammunition to those suspicious of PSA.
But Roobol emphasises that overdiagnosis was the result of the study not selecting according to risk and using systematic biopsies after raised PSA findings. The important point which policy makers need to take away from ERSPC is that it showed that early detection could be effective – reducing prostate cancer mortality by 27% at 13 years. Another smaller study of the same cohort indicated an even greater effect: a mortality reduction of 52% at 19 years.
“What we learned from ERSPC was that we can use the PSA test and make a huge difference. You just need the right risk stratification system afterwards, whether that uses advanced techniques such as MRI, or just uses the PSA level in a smart way, adding if possible prostate volume or digital rectal examination, for example, into the equation.”
Where next for EU policy?
No one believes that, when the European Commission produces its update to cancer screening recommendations next year, it will serve up a fully-formed prostate cancer screening programme ready for Europe-wide implementation. Realistically, what adherents like Van Poppel and Roobol are seeking is movement: a forceful European initiative to educate, correct misunderstandings, and set the foundations for national systems based on the realities of risks and benefits. Even international initiatives to educate men so that they can understand the issues would be a welcome start, says Roobol.
“Then, on that basis, a well-educated man can decide: ‘I really want this’. And then they can enter a national system where they can use an algorithm which is suitable for the setting in that country.”
The coming months will see an intensification of debate and consultation. It’s an opportunity not to be missed, believe Europe’s prostate cancer patient representatives.
“Our campaigning and informing work needs to continue,” says André Deschamps. “The door is half open, but we need to work hard this year to ensure that it is not closed again.”
Simon Crompton is a freelance journalist who provides communications services to many organisations, one of which is Europa Uomo.
Prostate cancer screening timeline
1980s: Prostate-specific antigen (PSA) blood tests introduced. PSA is a protein produced by the prostate gland that is detectable in blood. PSA levels rise when there is a benign enlargement of the prostate, an infection of the prostate, prostatitis or prostate cancer.
Early 1990s: Incidence of prostate cancer peaks as more men tested with PSA, leading to concerns about overdiagnosis. However, prostate cancer mortality also begins to decline.
Late 1990s: Concerns grow that too many men are being diagnosed with prostate cancer, leading to unnecessary treatments with unpleasant side effects, when the disease is not significant enough to kill them or affect their quality of life. Use of PSA testing declines in Europe.
2000s: Declines in mortality from prostate cancer level off, with rises in some countries. Mortality in the UK increases 17% in 10 years.
Research evidence grows that broad-brush screening of men using PSA tests leads to unnecessary biopsies and treatment, because of the difficulties of discriminating between significant cancers (which might kill a man) and insignificant cancers (which might never affect their lifespan or quality of life).
2010 onwards: Development of risk calculators, using multiple factors such as age, family history and PSA density alongside PSA, make it possible to identify those most at risk of serious disease, who may need further investigation and active treatment.
Active surveillance is increasingly recognised as an alternative to active treatment.
2017–2019: Results from two major trials (PROMIS and PRECISION) show that using multiparametric MRI (mpMRI) scans after a raised PSA reading and before biopsy is the most effective way of detecting significant prostate cancer. The scans effectively guide biopsies, leading to significantly more harmful prostate cancers, and fewer harmless cancers, being diagnosed.
2018: British Medical Journal publishes systematic review and guidelines tentatively recommending against prostate cancer screening programmes, on the basis of that harms and benefits are closely matched.
2019: EAU updates its early detection guidelines to recommend mpMRI after PSA testing and before biopsy.
2021: The European Commission announces it will consider the possibility of “extending targeted cancer screening beyond breast, colorectal and cervical cancer to include additional cancers, such as prostate, lung and gastric cancer”.
back to the article