Faced with poverty, low maternal education and fears about treatment effects, many families in sub-Saharan Africa are abandoning cancer treatment for children and young people, harming chances of survival.
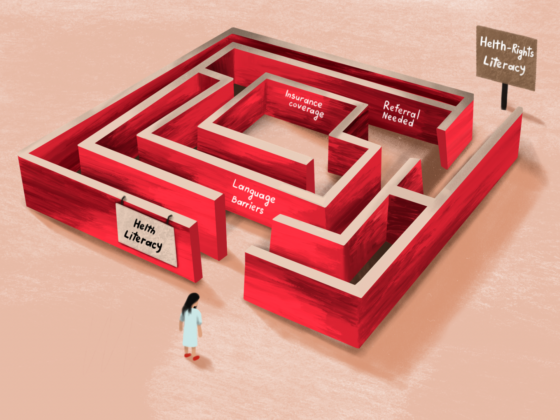
In Kenya and Zambia, for instance, treatments for childhood cancers are abandoned in around half of all cases ‒ 54% in Kenya and 46% in Zambia ‒ according to The Lancet Oncology Commission, reporting on the problem in May 2022. The Commission found that high costs are major barriers to accessing treatment in sub-Saharan Africa, with African countries paying higher prices for cancer drugs on average compared with Latin American countries with a similar income level or disease rate.
The Commission also highlighted the lack of psychosocial support and a shortage of paediatric oncologists, which leaves children to be treated by nurses and medical officers. It recognised that major investments in training and recruitment will struggle to address this staffing shortfall so long as high-income nations such as the UK continue to entice local staff with more lucrative job offers.
But there are other factors at play. The 14th International Society of Paediatric Oncology (SIOP) Africa Continental Congress, held in Uganda in March 2022, heard that lack of transport to health facilities, the choice of traditional healers over clinically trained physicians, and lack of finance and information also play a part in treatment abandonment.
One of the speakers at the congress was Claire Atuhaire from Uganda, mother to a four-year-old child with leukaemia. “I don’t think all these parents understand the big words the doctors tell them,” she said. “I know that the doctors try their best to explain but… For example, when we were told that our child had cancer, we did not understand anything. I just stared at the doctor and heard only the word ‘cancer’. Nothing else. I was just crying.”
The case of John Mubiru (not his real name) was also presented at the conference. He first had tests for cancer when he was 17 years old, with a suspected cancer in his eye, which he then received treatment for.
John’s father was hesitant to continue treatment, because his son’s tests results were not explained, and because of money worries
Then a fast-growing tumour developed on his leg. At a visit to the oncology department with his father two years later, John refused to have a confirmatory biopsy, saying his first biopsy had been very painful and he had been given no pain relief. He flatly refused further treatment.
John’s father was also hesitant about continuing with treatment, because of frustration that the health workers did not explain the results of his son’s tests, and because of money worries. John dropped out of treatment.
Megan Cruise, a psychosocial support advisor working with World Child Cancer told the conference that the organisation’s survey of families found that financial support and good food would be of most value to make child patients’ stay in hospital comfortable. “They said financial support was critical and enabled them to treat their children. Families were also always mentioning the support they needed with nutrition.”
Nicholas Benedicto Chaula, an eye specialist from Tanzania, said that most children come from poor families, and the cost of tests and treatments causes them to seek alternatives like herbal remedies. Retinoblastoma is one of the most common cancers in young children in sub-Saharan Africa and is often diagnosed late, necessitating eye removal.
“If you advise on amputation, say of a leg, that is different from removing an eye,” said Chaula. “When I advise on removing an eye, the parents outrightly refuse because it’s more about appearance and confidence, and a leg is more acceptable.”
While conference participants agreed that psychosocial support could reduce rates at which cancer treatment are being abandoned, the professionals to provide it are not always available in African countries. “Our funders are eager to fund salaries of social workers, claiming they are affordable and their work is more measurable,” said Mawethu Bell, a social worker at CHOC Childhood Cancer Foundation, South Africa. “They also have been around for a while compared to a psychologist or a play therapist, for instance.”
“There’s lack of awareness and less emphasis placed on psychosocial cases because the measurable outcomes are not easily quantified”
Bell explained that, although play therapists play a vital role in the recovery of children with cancer, many providers don’t employ them. “There’s lack of awareness and less emphasis placed on psychosocial cases because the measurable outcomes are not easily quantified,” she said.
Claire Atuhaire’s daughter looks forward to going to hospital every month because she loves playing with her friends. “The journey for her recovery is tough but we are hopeful,” said Atuhaire. “The hospital is a happy place for her because she plays with her friends – but then she knows no other way. She has grown up in the hospital anyway.”
At the Congress, Atuhaire advocated for more awareness about the need for psychosocial support and making contact with parents and survivors with similar challenges. “We are the primary care givers. I learned a lot from a fellow parent and the fact that her child is thriving kept me going and strong,” said Atuhaire.
Featured image credit: Daniel Msirikale for Direct Relief, republished under a Creative Commons licence.